Abstract
The aim of this retrospective, case–control study was to determine the effect of the amphotericin B lipid complex (ABLC) on serum creatinine (SCr), blood urea nitrogen (BUN), sodium (Na), and potassium (K) in very low birth weight (VLBW) infants. Medical records of all VLBW infants who were admitted to our Neonatal Intensive Care Unit between May 1998 and May 2006 and had received ABLC for at least 2 weeks were reviewed for patient demographics, use of medications (ABLC, diuretics, xanthines, indomethacin, vancomycin, gentamicin, pressors, and inotropes), fluid intake, urinary output, and serum electrolytes. Thirty-five patients who received ABLC were identified and matched by gestational age (GA) to 35 patients who served as controls. Infants who received ABLC had an average GA of 25.7 ± 2.1 weeks and a birth weight of 764 ± 196 g. Between day 1 and 14 of ABLC treatment, the BUN decreased from 17.5 ± 11.5 to 10.5 ± 6.8 mg/dl (p = 0.01), the SCr varied between 0.78 ± 0.32 and 0.69 ± 0.32 mg/dl, Na varied between 136.6 ± 5.8 and 137.8 ± 3.6 mEq/l, and K varied between 4.8 ± 0.9 and 4.9 ± 0.6 mEq/l, respectively. Based on these results, we conclude that treatment with ABLC for 2 weeks did not increase BUN or SCr, nor decrease Na or K in VLBW infants.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Renal function is immature in very low birth weight (VLBW) premature infants as compared to adults [1–4]. The amphotericin B lipid complex (ABLC; Abelcet; Enzon Pharmaceuticals, Bridgewater, NJ) has been approved in patients with renal failure or patients with side effects related to amphotericin B deoxycolate (Fungizone). The structure of ABLC consists of non-liposomal lipid bilayers, or “ribbons”, complexed with amphotericin B; as such, it has a selective affinity to fungal (ergo-based) rather than mammalian (cholesterol-based) cellular membranes and, therefore, is less nephrotoxic than amphotericin B [5–7]. However, ABLC may also induce azotemia, a decreased glomerular filtration rate, and severe hypokalemia [8, 9]. The ABLC and other lipid formulations of amphotericin B, such liposomal amphotericin B, have been used in preterm infants, term infants, children, and adults [7, 8, 10–17]. Although a number of studies have compared the different types of lipid formulations of amphotericin B or compared a lipid formulation and regular amphotericin B in infants and adults [7, 9], the effect of ABLC (Abelcet) on renal function and serum electrolytes in VLBW infants has not been fully investigated. Consequently, the aim of the study reported here was to determine the effect of ABLC on serum creatinine (SCr), blood urea nitrogen (BUN), sodium (Na), and potassium (K) in VLBW infants.
Patients and methods
Patients
The medical records of all VLBW infants (≤1500 g at birth) admitted to our Neonatal Intensive Care Unit between 1 May 1998 and 1 May 2006 were reviewed. All VLBW infants who received ABLC for at least 2 weeks were included in the study. Each patient who received ABLC was matched for gestational age (GA) and birth weight (BW) (within 10%) with a previously or consecutively admitted VLBW infant who was not treated with antifungal therapy.
Patients were excluded from the study if they had a severe congenital abnormality or were oligo-anuric (defined as an average daily urinary output < 1 ml/kg per hour during the study period for the control group or prior to the administration of ABLC in the ABLC group). Hemolyzed samples, as identified by the laboratory technicians, were also excluded. Medical records were reviewed for GA, BW, gender, race, Apgar scores at 1 and 5 min, daily fluid intake, and daily urinary output. The medical records were also reviewed for morning laboratory values for BUN, SCr, serum Na, and serum K during the study period. The study period was defined as the first 2 weeks of treatment with ABLC in the ABLC group or the corresponding matched 2 weeks in the control group. For example, if an infant was started on ABLC on his 5th day of life, his medical record was reviewed and data recorded for the next consecutive 14 days (from day 5 to day 19 of life). The matched control infant’s medical record was reviewed for the same period (day 5 to day 19 of life).
The use of medications during the study period that would interfere with renal function, such as indomethacin, vancomycin, gentamicin, xanthines (aminophylline and caffeine), pressors (dopamine), inotropes (dobutamine) and diuretics (furosemide, hydrochlorothiazide and bumetanide), were also reviewed. Medical records were also reviewed for days of mechanical ventilation during the study period.
An increase in SCr or in BUN was defined as an increase in SCr or BUN by 50% from baseline on any day during the study period. Hyponatremia was defined as a serum Na < 125 mEq/l, and hypokalemia was defined as a serum K < 4.2 mEq/l on any day during the study period.
During the study period, it was the treating physician’s preference to use Abelcet whenever a fungal infection was suspected (given the lipid formulation’s lower side effects in older patients). Abelcet was always mixed in dextrose–water and administered over a 2-h period intravenously. In accordance with our unit’s policy, infants were not routinely pretreated with an intravenous saline infusion prior to the Abelcet infusion.
The study was approved by our Institutional Review Board at MetroHealth Medical Center.
Statistical analysis
A t test was used to compare continuous variables, and a chi-square test was used to compare nominal variables. All data were expressed as means ± standard deviations or as medians with interquartile ranges. Statistical significance was set at p < 0.5. A logistic regression analysis was used to adjust for possible confounding. Variables known to affect SCr and serum electrolytes were entered in a logistic regression model using the presence or absence of an increase in SCr > 50% from baseline during the study period as a classifying and dependent variable. Similar logistic regression analyses were also conducted, whereas the classifying and dependent variables were either an increase in BUN > 50% from baseline or hyponatremia (Na < 125 mEq/l) or hypokalemia (K < 4.2 mEq/l) during the study period.
Results
During the study period, 1143 VLBW infants were admitted to our NICU. However, only 35 VLBW infants received ABLC for at least 2 weeks and met our inclusion criteria. Thirty-five infants, matched for GA and BW, served as controls.
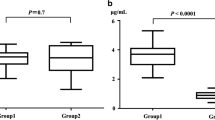
The patients’ demographics and baseline characteristics are summarized in Table 1. There were no differences between the ABLC group and the control group in terms of GA, BW, gender, or race. However, patients on ABLC had a lower Apgar score at 1 min but a similar Apgar score at 5 min of age. The daily fluid intake, urine output, and morning serum electrolytes at different times during the study period are summarized in Table 2. In patients treated with ABLC, the baseline values for fluid intake, urine output, SCr, or serum K did not differ from those at 1 and 2 weeks of treatment; however, there was a decrease in BUN values between the baseline and 2-week measurements. When the ABLC group was compared to the control group, the ABLC group had a higher BUN at baseline and also a higher Na after 2 weeks of ABLC treatment.
There were no differences between the ABLC and the control groups regarding the concomitant use of other medications that can affect renal function during the study period (such as diuretics, indomethacin, gentamicin, and dopamine/dobutamine). However, the ABLC group received more vancomycin and less xanthines than the control group [26/35 (74%) vs. 15/35 (42%), p = 0.007; 14/35 (40%) vs. 24/35 (68%), p = 0.01, respectively]. To adjust for risk factors associated with an elevated SCr, we conducted a logistic regression analysis. Variables known to affect SCr were entered in a logistic regression model using the presence or absence of SCr > 50% of baseline during the study period as a classifying and dependent variable. Among all of the variables that might have affected SCr, ABLC was not found to be associated with an increase in SCr, whereas gentamicin, dopamine, and dobutamine were found to be associated with increased SCr levels (Table 3).
During the study period, 20% (7/35) of the patients in the ABLC group and 20% (7/35) of those in the control group showed a >50% increase in SCr.
To adjust for the higher BUN level at baseline in the ABLC group, another logistic regression analysis was conducted in which >50% increase in serum BUN was set as the dependent variable. The ABLC was also not found to be among the variables that might have affected serum BUN, although xanthines were found to be protective against azotemia (Table 4). During the study period, 26% (9/35) of the patients in the ABLC group and 26% (9/35) of the patients in the control group had a >50% increase in BUN.
To adjust for risk factors associated with hypokalemia or hyponatremia, we also conducted two logistic regression analyses in which the classifying and dependent variables were either hyponatremia (Na < 125 mEq/l) or hypokalemia (K < 4.2 mEq/l) during the study period, and the risk factors were the same as the factors used in the two previous analyses. None of the aforementioned risk factors or ABLC was associated with hyponatremia or hypokalemia: 66% (23/35) of patients in the ABLC group had hypokalemia versus 46% (16/35) in the control group (p = 0.09), and 14% (5/35) of the patients in the ABLC group had hyponatremia versus 6% (2/35) in the control group (p = 0.42).
During the study period, 83% (29/35) of ABLC patients were on mechanical ventilation versus 66% (23/35) of control patients (p = 0.10). Control patients were admitted during the same period (within days, weeks or months) as ABLC patients. On average, control patients were admitted to the NICU within 110 ± 102 days of the admissions of the ABLC patients.
Among the 35 patients who were treated with ABLC, 15 patients had Candida albicans, 14 patients had C. parapsilosis (one patient had both C. albicans and C. parapsilosis), and seven patients did not have an identified organism. Twenty-two patients had a positive fungal blood culture, 13 had a positive fungal urine culture, seven had a positive fungal sputum culture, one patient had a positive fungal cerebral spinal fluid culture, and five patients had other sites that were positive for fungal infections. On average, ABLC therapy was started on 21.46 ± 24.64 days of life at a dose of 5.0 ± 0.1 mg/kg per day, and the duration of therapy was, on average, 25.11 ± 8.15 days (range 14–49 days). Infants who were treated with ABLC had a repeated negative fungal culture 6.6 ± 4.6 days (average) following the initiation of the ABLC therapy (median 6 days, interquartile range 3–8 days). All patients treated with ABLC had clearance of their fungal infections.
Discussion
We have shown that following 2 weeks of treatment with ABLC there was no significant alteration in SCr or electrolytes in VLBW infants. This finding is consistent with previous reports in children and infants [6, 11, 12, 17].
Walsh et al. [6], in a study evaluating the safety and efficacy of ABLC in pediatric patients between the age of 21 days and 16 years, found no significant change in the mean SCr levels, BUN, or K during 6 weeks of treatment. Their patients included 11 infants < 6 months of age (age 3–13 weeks, weight 0.8–5 kg) who received ABLC, and their findings are consistent with ours. We did not find any significant differences in SCr or K following 2 weeks of ABLC therapy. Our patients treated with ABLC had an elevated BUN at baseline; however, their BUN decreased over the 2-week period of antifungal therapy. In another study of six children (age 4–17 years) with hepatosplenic candidiasis and malignancies, ABLC did not induce a significant change in mean SCr throughout the 6-week course of therapy, but one patient developed hypokalemia during the administration of ABLC that resolved after the discontinuation of therapy [12]. In our VLBW infants, we found no significant differences in serum K or SCr between the ABLC and the control group during the 2-week study period. If we were to have followed our patients for a longer period we may have found more patients with significant hypokalemia. Our findings are also consistent with those of Adler-Shohet et al., who reported an improvement or no change in the renal function of eight 8 of 11 infants who received ABLC [17].
Different forms of amphotericin B with less nephrotoxicity have been used in infants. Liposomal amphotericin B (AmBisome), another lipid formulation of amphotericin B, has been used in premature infants. Scarcella et al. [10] reported that absence of side effects in 40 preterm infants treated with AmBisome (mean GA age 28 weeks). Juster-Reicher el al. [13] also found no major adverse effects in 24 VLBW infants treated with AmBisome (mean GA of 26 weeks), and Weitkamp et al. [14] reported the absence of nephrotoxicity related to AmBisome therapy in 21 VLBW infants (GA age 23–31 weeks). In another study of 52 preterm infants, Linder et al. showed an improvement in renal function during treatment with three amphotericin B preparations. They also found that K supplementation during treatment was required in 47% of infants who were treated with amphotericin B and in none of the VLBW infants who were treated with liposomal amphotericin B (n = 6) and amphotericin B colloidal dispersion (n = 14) [16]. To our knowledge, we are the first to report a large series of 35 VLBW infants treated with ABLC (Abelcet, a lipid formulation of amphotericin B).
In newborn and premature infants, amphotericin B deoxycolate has a narrow therapeutic index and can induce nephrotoxicity that is characterized by azotemia and renal tubular toxicity, such as renal concentrating defects, hypomagnesemia, and increased urinary losses of K and other elements [18–21]. Therefore, ABLC can be an alternative to amphotericin B deoxycolate in these infants [22].
We have previously shown that SCr decreases with advancing GA and BW [23]. Therefore, to be able to study the effect of ABLC on SCr that usually decreases with advancing GA, we added a matched control group of patients to our analysis in order to adjust for the factor of time on SCr. However, our study has several limitations. A significant number of our patients were also on other medications that could have affected SCr, BUN, Na, and K levels (such as antibiotics, diuretics, pressors, inotorops, indomethacin, and xanthines). To adjust for the concurrent use of such medications during the study period, we entered variables known to affect SCr and serum electrolytes in a logistic regression model using the presence or absence of an increase in SCr > 50% from baseline during the study period as a classifying and dependent variable. Similar logistic regression analyses were also conducted in which the classifying and dependent variables were either an increase in BUN > 50% from baseline or hyponatremia (Na < 125 mEq/l) or hypokalemia (K < 4.2 mEq/l) during the study period.
The ABLC was not found to be associated with an increase in SCr or BUN or a decrease in Na or K. However, xanthines were found to have a protective effect against an elevation in BUN, a finding that could be consistent with previous reports, whereas theophylline was found to improve renal function in preterm infants with respiratory distress syndrome [24], and in term infants with asphyxia [25].
We conclude that 2 weeks of ABLC (Abelcet) does not significantly change SCr, Na, or K levels in VLBW infants. Treatment with ABLC also does not increase serum BUN. Future larger studies with longer follow-ups (>2 weeks) are needed to establish prospectively the safety of ABLC and to compare its use to amphotericin B deoxycolate in VLBW infants.
References
Sonntag J, Prankel B, Waltz S (1996) Serum creatinine concentration, urinary creatinine excretion and creatinine clearance during the first 9 weeks in preterm infants with a birth weight below 1500 g. Eur J Pediatr 155(9):815–819
Gallini F, Maggio L, Romagnoli C, Marrocco G, Tortorolo G (2000) Progression of renal function in pretern neonates with gestational age ≤ 32 weeks. Pediatr Nephrol 15:119–124
van der Heijden AJ, Grose WF, Ambagtsheer JJ, Provoost AP, Wolff ED, Sauer PJ (1988) Glomerular filtration rate in the preterm infant: the relation to gestational and postnatal age. Eur J Pediatr 148(1):24–28
Vanpee M, Herin R, Zetterstrom R, Aperia A (1988) Postnatal development of renal function in very low birthweight infants. Acta Paediatr Scand 77(2):191–197
Hiemenz J, Walsh JT (1996) Lipid formulations of Amphotericin B: recent progress and future directions. Clin Infect Dis 22[Suppl 2]:S133–S144
Walsh TJ, Seibel NL, Arndt C, Harris RE, Dinubile MJ, Reboli A, Hiemenz J, Chanock SJ (1999) Amphotericin B lipid complex in pediatric patients with invasive fungal infections. Pediatr Infect Dis J 18(8):702–708
Sorkine P, Nagar H, Weinbroum A, Setton A, Istraitel E, Scarlatt A, Silbiger A, Rudick V, Kluger Y, Halpern P (1996) Administration of amphotericin B in lipid emulsion decreases nephrotoxicity: Results of a prospective, randomized, controlled study in critically ill patients. Crit Care Med 24(8):1308–1315
Wong-Beringer A, Jacobs RA, Guglielmo BJ (1998) Lipid formulations of Amphotericin B: clinical efficacy and toxicities. Clin Infect Dis 27(3):603–618
Cannon JP, Garey KW, Danziger LH (2001) A prospective and retrospective analysis of the nephrotoxicity and efficacy of lipid-based amphotericin formulations. Pharmacotherapy 21(9):1107–1114
Scarcella A, Pasquariello MB, Giugliano B, Vendemmia M, de Lucia A (1998) Liposomal amphotericin B treatment for neonatal fungal infections. Pediatr Infect Dis J 17(2):146–148
Knoppert DC, Salama HEM, Lee DSC (2001) Eradication of severe neonatal systemic candidiasis with amphotericin B lipid complex. Ann Pharmacother 35(9):1032–1036
Walsh TJ, Whitcomb P, Piscitelli S, Figg WD, Hill S, Chanock SJ, Jarosinski P, Gupta R, Pizzo PA (1997) Safety, tolerance, and pharmacokinetics of amphotericin B lipid complex in children with hepatosplenic candidiasis. Antimicrob Agents Chemother 41(9):1944–1948
Juster-Reicher A, Leibovitz E, Linder N, Amitay M, Flidel-Rimon O, Even-Tov S, Mogilner B, Barzilai A (2000) Liposomal amphotericin B (AmBisome) in the treatment of neonatal candidiasis in very low birth weight infants. Infection 28(4):223–226
Weitkamp JH, Poets CF, Sievers R, Musswessels E, Groneck P, Thomas P, Bartmann P (1998) Candida infection in very low birth-weight infants: outcome and nephrotoxicity of treatment with liposomal amphotericin B (AmBisome). Infection 26(1):11–15
Friedlich PS, Steinberg I, Fujitani A, deLemos RA (1997) Renal tolerance with the use of intralipid-amphotericin B in low-birth-weight neonates. Am J Perinatol 14(7):377–383
Linder N, Klinger G, Shalit I, Levy I, Ashkenazi S, Haski G, Levit O, Sirota L (2003) Treatment of candidaemia in premature infants: comparison of three amphotericin B preparations. J Antimicrob Chemother 52(4):663–667
Adler-Shohet F, Waskin H, Lieberman JM (2001) Amphotericin B lipid complex for neonatal invasive candidiasis. Arch Dis Child Fetal Neonatal Ed 84(2):F131–F133
Ward MD (1984) Amphotericin B (Fungizone). Crit Care Nurse 4(6):7–11
Walsh TJ, Hiemenz JW, Anaissie E (1996) Recent progress and current problems in treatment of invasive fungal infections in neutropenic patients. Infect Dis Clin North Am 10(2):363–393
Baley JE, Meyers C, Kliegman RM, Jacobs MR, Blumer JL (1990) Pharmacokinetics, outcome of treatment, and toxic effects of amphotericin B and 5-fluorocytosine in neonates. J Pediatr 116(5):791–797
Fanos V, Cataldi L (2000) Amphotericin B-induced nephrotoxicity: a review. J Chemother 12(6):463–470
Leibovitz E (2002) Neonatal candidosis: clinical picture, management controversies and consensus, and new therapeutic options. J Antimicrob Chemother 49[Suppl 1]:69–73
Auron A, Mhanna MJ (2006) Serum creatinine in very low birth weight infants during their first days of life. J Perinatol 26(12):755–760
Cattarelli D, Spandrio M, Gasparoni A, Bottino R, Offer C, Chirico G (2006) A randomised, double blind, placebo controlled trial of the effect of theophylline in prevention of vasomotor nephropathy in very preterm neonates with respiratory distress syndrome. Arch Dis Child Fetal Neonatal Ed 91(2):F80–F84
Jenik AG, Ceriani Cernadas JM, Gorenstein A, Ramirez JA, Vain N, Armadans M, Ferraris JR (2000) A randomized, double-blind, placebo-controlled trial of the effects of prophylactic theophylline on renal function in term neonates with perinatal asphyxia. Pediatrics 105(4):E45
Financial support:
None.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Auron, A., Auron-Gomez, M., Raina, R. et al. Effect of amphotericin B lipid complex (ABLC) in very low birth weight infants. Pediatr Nephrol 24, 295–299 (2009). https://doi.org/10.1007/s00467-008-1017-5
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00467-008-1017-5