Abstract
Background and Objective
Gentamicin is commonly used in neonates, and it requires drug concentration monitoring. The objective of this study was to determine the extent of high trough (≥ 2 mg/l) and therapeutic peak serum gentamicin concentrations (5–12 mg/l) using our current gentamicin regimen and to adjust the dosing regimen accordingly and reassess.
Methods
This was a prospective cohort study of neonates, with normal renal function, who were prescribed gentamicin. Group 1: March 2014–July 2017—gentamicin intravenous (IV) 2.5 mg/kg given every 36 h if < 30 weeks gestational age (GA) and every 24 h if ≥ 30 weeks GA; Group 2: August 2019–February 2020—gentamicin IV 3.5 mg/kg given every 36 h if < 30 weeks GA and every 24 h if ≥ 30 weeks GA. We assessed the number of neonates with aberrant trough and peak serum gentamicin concentrations.
Results
Forty-eight neonates < 30 weeks GA and 34 ≥ 30 weeks GA were given 2.5 mg/kg gentamicin. Eleven (23%) neonates < 30 weeks GA and four (13%) ≥ 30 weeks GA had subtherapeutic peak concentrations (< 5 mg/l); none had supratherapeutic (> 12 mg/l) or toxic trough concentrations (≥ 2 mg/l). Forty-four neonates < 30 weeks GA and 54 ≥ 30 weeks GA were given 3.5 mg/kg gentamicin. Eighty-four (86%) had non-toxic trough concentrations (< 2 mg/l). One (1%) < 30 weeks GA neonate had subtherapeutic (< 5 mg/l) and one (1%) neonate ≥ 30 weeks GA had supratherapeutic (> 12 mg/l) peak concentrations.
Conclusions
Gentamicin regimen of 2.5 mg/kg given every 36 h for neonates < 30 weeks GA and every 24 h for neonates ≥ 30 weeks GA was suboptimal at achieving therapeutic gentamicin peak. Increasing the dosage to 3.5 mg/kg achieved therapeutic peak concentrations in 98% and non-toxic trough concentrations in 86% of all neonates (prior to dose interval adjustment).
Similar content being viewed by others
Avoid common mistakes on your manuscript.
In neonates given gentamicin at a dose of 2.5 mg/kg (given every 36 h if < 30 weeks GA and every 24 h if ≥ 30 weeks GA), none had toxic trough concentrations but 19% had peak concentrations that were sub-therapeutic |
Changing the routine gentamicin dosing regimen to 3.5 mg/kg (given every 36 h if < 30 weeks GA and every 24 h if ≥ 30 weeks GA) resulted in 98% of neonates achieving therapeutic peak gentamicin concentrations, with only a slight increase in toxic trough concentrations (prior to dose interval adjustment) |
1 Introduction
Gentamicin is one of the most commonly used antibiotics for treatment of neonates at risk of infection and for those with suspected or documented neonatal sepsis. It provides synergistic coverage for common neonatal pathogens [1]. There are many different neonatal gentamicin dosing regimens. These range from conventional multiple-dose/day regimens (low dose, short interval) to extended interval dosing (high dose, long interval) with doses ranging from 2.5 to 5 mg/kg given every 12 h in traditional multiple dose regimens to doses given every 24–48 h in extended interval regimens [1,2,3,4,5]. These extended interval regimens have largely been adopted, not because there is evidence that they are better, but because their use has been extrapolated from regimens used in adults and children. Some dosing regimens also account for gestational age (GA) [6].
The way gentamicin is used has changed. Traditionally, the aim was to achieve steady-state pharmacokinetics: adequate peak gentamicin serum concentrations and non-toxic trough concentrations [7, 8]. In the last 2 decades some have aimed for higher peak concentrations and very low trough concentrations so that these high-dose, long-interval regimens can take advantage of the post-antibiotic effect and decrease post-exposure resistance [7, 8]. Evidence for these extended-interval regimens over traditional steady-state regimens is insufficient. The latest Cochrane review [9] was unable to conclude whether once daily dosing versus multiple daily dosing is superior in the treatment of proven neonatal sepsis.
For traditional dosing regimens, acceptable trough concentrations are < 2 mg/l while peak serum gentamicin range is 5–12 mg/l [9,10,11,12,13,14,15]. The targets are based on the pharmacokinetic principles of achieving early and high peak gentamicin plasma concentrations, such that the target ratio of peak concentration (Cmax) to minimum inhibitory concentrations (MIC) for target organisms—Cmax:MIC—is 8–10 [16]. Sustained and elevated peaks > 12 mg/l, or troughs > 2 mg/l, can increase the risk of toxicity including ototoxicity and nephrotoxicity [16, 17], although much of the evidence is extrapolated from adults and animal studies [18]. Recent evidence suggests ototoxicity, although a possibility, is rare and is more likely with prolonged courses of aminoglycosides especially if given concomitantly with loop diuretics [19].
Our dosing regimen aimed for traditional steady-state pharmacokinetics, using a dose of 2.5 mg/kg of gentamicin, every 36 h for < 30 weeks GA and 24 h for ≥ 30 weeks GA. These dosage intervals were based on a retrospective audit showing that dosing intervals of 24 h in neonates < 30 weeks GA and 12 h in term neonates led to a significant number of toxic trough concentrations [8, 20]. The aim of this study was to determine the gentamicin concentrations that result from this gentamicin dosage regimen to consider the number of neonates with toxic trough concentrations and subtherapeutic and toxic peak concentrations and adjust the dosing regimen accordingly.
2 Methods
This study received ethical approval from the hospital ethics committee.
2.1 Participants
Neonates born between March 2014 and July 2017 within the first 2 days of life prescribed gentamicin as part of their usual care were considered for inclusion. Informed parental/carer consent was obtained by a member of the medical team. Each infant was only enrolled once in the study for one course of gentamicin.
A follow-up study was undertaken between August 2019 and February 2020 after adjustment of the gentamicin dosing regimen was made.
Inclusion Criteria
-
All neonates prescribed intravenous gentamicin as part of their usual care and management.
-
Neonates who received three or more doses of gentamicin.
Exclusion Criteria
-
Neonates with pre-existing renal or cardiac dysfunction.
-
Neonates for whom there were concerns regarding renal function:
-
for infants who received renal function testing, impaired renal function was defined as having a serum creatinine level > 0.09 mmol/l [21];
-
for those without renal function testing, renal function was deemed impaired if there was poor urine output - less than 1 mL/kg/h if measured, or less than four wet nappies in the 24 h preceding the gentamicin concentration.
-
The data collected included: infant’s birth weight; GA at birth; dose and dosage interval of gentamicin; the reason for gentamicin treatment and the weight of the infant at commencement of gentamicin.
The original dosage regimen in neonates was 2.5 mg/kg of gentamicin given every 36 h for neonates < 30 weeks GA and every 24 h for neonates ≥ 30 weeks GA. Gentamicin was undiluted from a 10 mg in a 1-ml vial and was given intravenously via either peripheral intravenous cannula or umbilical venous catheter as a push followed by a 0.9% sodium chloride flush.
2.2 Blood Samples
A blood sample for a trough serum concentration of gentamicin was taken 30 min prior to the third dose of gentamicin (usual practice). A blood sample for a peak serum concentration of gentamicin (not routinely monitored) was taken 1 h after the end of the third gentamicin injection. Only two blood samples were taken from each infant: one trough and one peak concentration. For each sample, 0.5 ml of blood was collected into a gel (clotted, serum) tube and sent immediately to the laboratory for analysis.
Analysis of gentamicin concentrations was conducted at the hospital Pathology Unit as per usual practice. A trough concentration of ≥ 2 mg/l was considered to indicate a significant risk of toxic gentamicin accumulation. A peak concentration of > 12 mg/l was considered a risk for toxicity. A peak concentration of < 5 mg/l was considered subtherapeutic.
2.3 Follow-up Study
The follow-up study was conducted in neonates born between August 2019 and February 2020.
The theoretical optimum dose of gentamicin to minimise non-therapeutic peak concentrations was determined by extrapolation of the original data based on the following two assumptions: (1) the peak concentration will be proportional to the dose given (the principle of first order kinetics: serum concentration is directly proportional to dose if the volume of distribution is unchanged [22]) and (2) the variation in the calculated mean (i.e., the SD) is the same as that for a 2.5 mg/kg dose and resultant frequency distribution is normal (as is the frequency distribution of our data tested with Kolmogorov-Smirnov normality test). Based on these distributions we then calculated the z-scores for cutoff concentrations of 5 and 12 mg/l and the resultant proportions above and below these z-scores. The new regimen was 3.5 mg/kg of gentamicin given every 36 h for neonates < 30 weeks GA and every 24 h for neonates ≥ 30 weeks GA. Inclusion and exclusion parameters remained the same. Sampling times and analysis remained the same.
2.4 Bioanalytical Assay
Analysis of gentamicin concentrations was conducted at the hospital Pathology Unit with a Beckman DXC800 analyser (Beckman Coulter Australia Pty Ltd, Sydney, Australia) using a particle enhanced turbidimetric inhibition immunoassay, as per usual practice for samples sent from our nursery [23].
2.5 Statistical Analyses
Associations between GA groups or gentamicin doses and categorical variables were examined using χ2 test or Fisher’s exact test. Associations between GA groups or gentamicin doses and continuous variables were examined using a two-sample t-test or the Wilcoxan rank-sum test. Categorical variables were summarised by frequency and percentage and continuous variables were summarised by mean and standard deviation (SD) or median and (IQR—interquartile range). Statistical analyses were performed in Stata version 15 (StataCorp, College Station, TX, USA).
The original sample size aimed to recruit 200 infants based on admission rates; however, due to extremely poor recruitment and slowing with no reasonable prospect of achieving the original intended number, it was thought reasonable to analyse the existing data to prevent any further delay in obtaining the data required to inform clinical practice.
3 Results
3.1 Original Study: Gentamicin Regimen 2.5 mg/kg Given Every 36 h for Neonates < 30 Weeks GA and Every 24 h for Neonates ≥ 30 Weeks GA
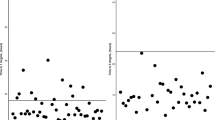
Eighty neonates were included in the initial study: group 1, from < 30 weeks GA (n = 47), and group 2, ≥ 30 weeks GA (n = 33). Table 1 shows the birth weights, GAs and reason for gentamicin treatment. Table 2 presents the gentamicin concentrations for the whole cohort and both groups. A total of 79 neonates had peak concentrations included (one excluded for peak concentration taken at incorrect time). All 80 neonates had trough concentration < 2 mg/l. No infant had supratherapeutic peak serum gentamicin concentrations. Overall, 19% of peak concentrations were sub-therapeutic. Eleven (23%) of the < 30 weeks GA neonates had subtherapeutic peak concentrations (< 5 mg/l). Four (12%) of the ≥ 30 GA neonates received had subtherapeutic peak concentrations.
There was no evidence of an association between GA groups and peak gentamicin concentrations (p = 0.23). No neonates were found to have toxic trough concentrations at the 2.5 mg/kg dose. There was no evidence of a difference in trough concentrations between GA groups (p = 0.12), nor was there evidence of a difference in the peak concentrations between GA groups (p = 0.10).
Following the results of the 2.5 mg/kg data, extrapolation analysis indicated 3.5 mg/kg was an optimal gentamicin dose to achieve the required therapeutic concentrations.
3.2 Follow-up Study: Gentamicin Regimen 3.5 mg/kg Given Every 36 h for Neonates < 30 Weeks GA and Every 24 h for Neonates ≥ 30 Weeks GA
Ninety-eight infants were included following the gentamicin dose increase, 44 infants < 30 weeks GA and 54 infants ≥ 30 weeks GA. All received gentamicin on the first day of life. Table 3 shows the birth weights, GAs and reason for gentamicin treatment. Table 4 presents the overall gentamicin concentrations and those compared between the two groups.
Of the 44 neonates in the < 30 weeks GA group, none had supratherapeutic peak concentrations. Of the 54 neonates in the ≥ 30 weeks GA group, none had subtherapeutic peak concentrations.
Overall 84 (86%) infants had trough concentrations < 2 mg/l. Three (6.8%) neonates < 30 weeks GA and 11 (20%) ≥ 30weeks GA had trough concentrations ≥ 2 mg/l; all had their dosage intervals extended as a result.
There was no significant association between the frequency of trough concentrations ≥ 2 mg/l and GA groups (p = 0.057). The ≥ 30 weeks GA group had significantly higher trough concentrations (1.5 mg/l vs. 0.8 mg/l, p < 0.001) and peak concentrations (9.2 mg/l vs. 8.3 mg/l, p < 0.006). There was only one (1.2%) neonate in the < 30 weeks group with a sub-therapeutic peak gentamicin concentration and one (1.2%) in the ≥ 30 weeks group with a supratherapeutic peak.
Table 5 presents the gentamicin concentrations for each of the GA groups compared between the 2.5 and 3.5 mg/kg gentamicin dose regimens. There was evidence of an association between GA and sub- and supra-therapeutic peak gentamicin concentrations and dose regimen (p < 0.005, < 30 weeks GA and p < 0.027, ≥ 30 weeks GA). No evidence of an association in trough toxicity between dose regimens in the < 30 weeks GA groups was found (p = 0.069), while there was strong evidence of an association with trough toxicity and dose regimens in the ≥ 30 weeks GA group (p = 0.006), with trough toxicity (i.e., a trough concentration of ≥ 2 mg/l) only exhibited in 11 neonates administered the 3.5 mg/kg dose.
4 Discussion
Gentamicin, like all other aminoglycosides, has a narrow therapeutic window [5], and its bactericidal effect depends on the plasma concentration; higher peak concentration enhances the therapeutic response [24]. However, getting the balance between dosing regimens which achieve maximal bactericidal effect (high peak concentrations), non-toxic trough concentrations that minimise the risk of ototoxicity and nephrotoxicity [5, 23] and potentially low enough trough concentrations (post-antibiotic effect and preventing adaptive microbial resistance) remains an issue [7, 25, 26]. Also, both GA and birth weight remain significant factors affecting gentamicin elimination [2, 16]. There have been limited studies on gentamicin dosing and drug concentrations in neonates < 30 weeks GA. There are large variations in recommended dosing regimens (Table 6).
We found that using 2.5 mg/kg (every 36 h for neonates < 30 weeks GA and every 24 h for neonates ≥ 30 weeks GA) was safe, with no toxic troughs or supra-therapeutic peak concentrations. Our results were comparable with Hansen et al. [15], who studied neonates < 35 weeks GA and ≥ 35 weeks GA, using extrapolated data to ascertain that gentamicin given every 36 h in neonates < 35 weeks GA yields non-toxic trough concentrations in 100% of patients. These data support the physiological effect prematurity has on extending the gentamicin elimination half-life, with kidney function proportional to GA [5]. Preterm neonates having fewer glomeruli, reducing glomerular filtration rate and overall diminished kidney function [6, 27], increasing their susceptibility to toxicity.
Unfortunately, the dose of 2.5 mg/kg resulted in suboptimal peak concentrations of gentamicin in 19% of all neonates, 23% of < 30 weeks GA and 13% of ≥ 30 weeks GA. This significant proportion of neonates with peak gentamicin concentrations that do not lie in the target range is clear evidence that the dose of 2.5 mg/kg is simply too low. Similar results were found by Gooding et al. [28], with 81% of < 28 weeks GA neonates not achieving therapeutic peaks with 2.5 mg/kg 24 hourly dosing. Hansen et al. [15] found neonates < 35 weeks GA dosed at 3 mg/kg 24 hourly resulted in 21% subtherapeutic peak concentrations.
Following this interim analysis, the dosing regimen was increased to 3.5 mg/kg/dose at the same dosing interval for GAs. This revealed a significant improvement compared to 2.5 mg/kg (p < 0.005) at effectively achieving therapeutic gentamicin concentrations in 98% of neonates and non-toxic trough concentrations in 86% of neonates. Our results of median trough and mean peak concentrations were comparable to Hoff et al.'s [16] dosing of 4 mg/kg every 48 h if birth weight was < 1250 g and 4 mg/kg every 24 h if birth weight was ≥ 1250 g.
There was an increase in the number of high trough concentrations in the ≥ 30 week GA group, with 11 neonates having trough concentrations 2–2.2 mg/l (all within a 30–31.8-week GA range). This accounted for 41% (11/27) of the neonates within this specific GA range, all of which had normal renal function (none had proven sepsis). All of these neonates had the dosing frequency reduced to 36 hourly with good effect. A similar result was found by Fullas et al. [10], with dosing of neonates within the 30–34-week GA group at 3.5 mg/kg every 36 h resulting in only 56% of infants having trough concentrations within the targeted ranges. This does highlight the potential for this gestation age range, 30–32 weeks, being more at risk of poor gentamicin clearance and subsequent high trough concentrations, despite normal renal function, and reinforces the need for ongoing trough monitoring in all babies if requiring three or more doses of gentamicin. To avoid toxic drug accumulation, it would be prudent not to use too high a dose of gentamicin and to monitor trough concentrations of gentamicin. If this is done early, the dose interval can be adjusted by day 3 of life, thus preventing a prolonged period of time with high trough levels and drug accumulation, especially in the neonates born from 30 to 32 weeks GA.
One of this study’s strengths is the fact that neonates were studied in two different GA groups, specifically those < 30 weeks GA, accounting for 58% of all neonates included in the study. These results are particularly important as this GA group is vulnerable to the effects of medications in general and this population has not been well studied. The limitations to the study include: (1) the proposed number of the patients recruited for the study was not met because of extremely poor recruitment and slowing with no reasonable prospect of achieving the original intended number. (2) The use of a convenience sample of neonates (rather than all neonates or a random sample) may produce a non-representative sample. (3) Very few neonates within the study had actual infection (the effect of dosing of neonates when critically unwell cannot be extrapolated from this data). (4) Only the gentamicin concentrations were studied, not the neonatal response to therapy (i.e., effective resolution of infection or recurrence of infection could not be assessed).
5 Conclusions
The original gentamicin regimen of 2.5 mg/kg given every 36 h for neonates <3 0 weeks GA, and every 24 h for neonates ≥ 30 weeks GA, carried little risk of gentamicin toxicity. However, approximately one in four peak concentrations did not achieve a therapeutic range for neonates < 30 weeks GA. Changing the routine gentamicin dosing regimen for neonates to 3.5 mg/kg given every 36 h if < 30 weeks GA and every 24 h if ≥ 30 weeks GA resulted in 98% of neonates achieving therapeutic peak gentamicin concentrations, with a slight increase in toxic trough concentrations (prior to dose interval adjustment).
The new dosing regimen has been shown to be reliable in preterm and term neonates with normal renal function and will be included in the revised Queensland Neonatal Clinical Guideline for Early Onset Group B Streptococcal disease 2021. Further research is required to evaluate gentamicin regimens in neonates with evidence of impaired renal function.
References
Hagen I, Oymar K. Pharmacological differences between once daily and twice daily gentamicin dosage in newborns with suspected sepsis. Pharm World Sci. 2009;31:18–23.
Low YS, Tan SL, Wan AS. Extended-interval gentamicin dosing in achieving therapeutic concentrations in Malaysian Neonates. J Pediatr Pharmacol Ther. 2015;20:119–25.
Hitron AE, Yao S, Scarpace SB. Accuracy of empiric gentamicin dosing guidelines in neonates. J Pediatr Pharmacol Ther. 2010;15:264–73.
Lannigian R, Thomson A. Evaluation of 22 neonatal gentamicin dosage protocols using Bayesian approach. Paediatr Perinat Drug Ther. 2001;4:92–100.
Skopnik H, Wallraf R, Nies B, Troster K, Heimann G. Pharmacokinetics and antibacterial activity of daily gentamicin. Arch Dis Childhood. 1992;67:57–61.
Kadambari S, Heath PT, Sharland M, Lewis S, Nichols A, Turner MA. Variation in gentamicin and vancomycin dosage and monitoring in UK neonatal units. J Antimicrob Chemother. 2011;66:2647–50.
Davies MW. Gentamicin dosage in neonates. Infect Med. 2000;17:634.
Davies MW, Cartwright DW. Gentamicin dosage intervals. J Paediatr Child Health. 1999;35:412.
Rao SC, Ahmed M, Hagan R. One dose per day compared to multiple doses per day of gentamicin for treatment of suspected or proven sepsis in neonates. Cochrane Database Syst Rev. 2006;25:CD005091.
Fullas F, Padomek MT, Thieman CJ, Van Gorp AE. Comparative evaluation of six extended-interval gentamicin dosing regimens in preterm and full-term neonates. Am J Health-Syst Pharm. 2011;68:52–6.
Langlass TM, Mickle TR. Standard gentamicin dosage regimen in neonates. Am J Health-Syst Pharm. 1999;56:440–3.
Murphy JE, Austin ML, Frye RF. Evaluation of gentamicin pharmacokinetics and dosing protocols in 195 neonates. Am J Health-Syst Pharm. 1998;55:2280–8.
DiCenzo R, Forrest A, Slish JC, et al. A gentamicin pharmacokinetic population model and once-daily dosing algorithm for neonates. Pharmcotherapy. 2003;23:585–91.
Bauer LA. Aminoglycoside antibiotics. In: Bauer LA, editor. Clinical pharmacokinetics handbook. New York: The McGraw-Hill Companies; 2005. p. 55–7.
Hansen A, Forbes P, Arnold A, O’Rouke E. Once-daily gentamicin dosing for the preterm and term newborn: Proposal for a simple regimen that achieves target levels. J Perinat Med. 2003;23:635–9.
Hoff DS, Wilcox RA, Tollefson LM, Lipnik PG, Commers AR, Liu M. Pharmacokinetic outcomes of a simplified, weight-based, extended-interval gentamicin dosing protocol in critically ill neonates. Pharmacotherapy. 2009;29:1297–305.
Touw DJ, Westerman EM, Sprij AJ. Therapeutic drug monitoring of aminoglycosides in neonates. Clin Pharmacokinet. 2009;48(2):71–88.
Musiime GM, Seale AC, Moxon SG, Lawn JE. Risk of gentamicin toxicity in neonates treated for possible severe bacterial infection in low- and middle-income countries: systematic review. Trop Med Int Health. 2015;20(12):1593–606.
Kent A, Turner MA, Sharland M, Heath PT. Aminoglycoside toxicity in neonates: something to worry about? Expert Rev Anti Infect Ther. 2014;12(3):319–31.
Davies MW, Cartwright DW. Gentamicin dosage intervals in neonates: longer dosage interval—less toxicity. J Paediatr Child Health. 1998;34:577–80.
Feldman H, Guignard J-P. Plasma creatinine in the first month of life. Arch Dis Child. 1982;57:123–6.
Ahmed TA. Pharmacokinetics of drugs following IV bolus, IV infusion, and oral administration [Internet]. Intechopen; 2015 [cited 2019 Jul 9]. https://www.intechopen.com/books/basic-pharmacokinetic-concepts-and-some-clinical-applications/pharmacokinetics-of-drugs-following-iv-bolus-iv-infusion-and-oral-administration, https://doi.org/10.5772/61573
Beckman Coulter Inc. Chemistry Information Sheet 0151Gentamicin. https://www.beckmancoulter.com/wsrportal/techdocs?docname=/cis/A18492/%25%25/EN_GEN.pdf. Accessed 6 July 2021.
Moore RD, Lietman PS, Smith CR. Clinical response to aminoglycoside therapy: importance of the ratio of peak concentration to minimal inhibitory concentration. J Infect Dis. 1987;155:93–9.
Nestaas E, Bangstad HJ, Sandvik L, Wathe KO. Aminoglycoside extended interval dosing in neonates is safe and effective: a meta-analysis. Arch Dis Child Fetal Neonatal Ed. 2005;90:294–300.
Barclay ML, Begg EJ. Aminoglycoside adaptive resistance: importance for effective dosage regimens. Drugs. 2001;61:713–21.
Koren G. Therapeutic drug monitoring principles in the neonate. Clin Chem. 1997;43:222–7.
Gooding N, Elias-Jones A, Shenoy M. Gentamicin dosing in neonatal patients. Pharm World Sci. 2001;23:179–80.
Low YS, Tan SL, Wan ASL. Extended-interval gentamicin dosing in achieving therapeutic concentrations in Malaysian neonates. J Pediatric Pharmacol Ther. 2015;20(2):119–27.
García B, Barcia E, Pérez F, Molina IT. Population pharmacokinetics of gentamicin in preterm newborns. J Antimicrob Chemother. 2006;58(2):372–9.
Stolk LML, Degraeuwe PLJ, Nieman FHM, De Wolf MC, Boer AD. Population pharmacokinetics and relationship between demographic and clinical variables and pharmacokinetics of gentamicin in neonates. Ther Drug Monit. 2002;24:527–31.
Acknowledgements
Queensland Health Pathology Services and Ms Anje Van Aswegen and Ms Acacia Fairweather for assistance with data collection.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Funding
No source of funding.
Conflict of interest
No conflicts of interest.
Ethics approval
This study received ethical approval from the Royal Brisbane and Women’s Hospital Human Research Ethics Committee (reference no. HREC/13/QRBW/12), and all procedures in this study were in accordance with the 1964 Helsinki Declaration (and its amendments).
Consent to participate
The parent or carer of each infant gave written informed consent for their infant to participate in the study.
Consent for publication
Not applicable.
Code availability
Not applicable.
Author contributions
MD, KW and DC contributed to the conception and design of this study; KOC and KW performed the statistical analysis and drafted the manuscript; PK, MD and DC critically reviewed the manuscript; MD and KW supervised the whole study process. All authors read and approved the final manuscript.
Rights and permissions
About this article
Cite this article
O’Connor, K., Davies, M.W., Koorts, P. et al. Gentamicin Dosing in Neonates with Normal Renal Function: Trough and Peak Levels. Eur J Drug Metab Pharmacokinet 46, 677–684 (2021). https://doi.org/10.1007/s13318-021-00708-x
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s13318-021-00708-x