Abstract
Cardiac hypertrophy is frequently encountered in patients with renal failure and represents an independent risk factor for cardiovascular morbidity and mortality. The pathogenesis of cardiac hypertrophy is related to multiple factors, including excess adrenergic activity. This study investigated how renal injury in the early stages of life affects the adrenergic system and thereby potentially influences cardiac growth. Biomarkers of cardiac hypertrophy were used to assess adrenergic function. Newborn male Sprague-Dawley rats were allocated to three groups of five rats each: 5/6 nephrectomy (Nx), pair-fed controls (PF), and sham-operated (SH). Nx animals had significantly higher plasma urea nitrogen, serum creatinine, and mean arterial blood pressure. The heart-weight/body-weight ratio of the Nx cohort was higher than SH and PF (p < 0.001) groups. Plasma norepinephrine (NE) of Nx animals was almost twofold higher than SH and PF (p < 0.01) animals. Compared with SH and PF, Nx animals had higher α1A-receptor protein expression, lower cardiac β1- and β2-receptor protein expression (p < 0.05), but higher G-protein-coupled receptor kinase-2 (GRK2) expression (p < 0.05). Norepinephrine transporter protein (NET) and renalase protein expression in cardiac tissue from Nx pups were significantly lower than SH and PF. Our data suggest that early age Nx animals have increased circulating catecholamines due to decreased NE metabolism. Enhancement of cardiac GRK2 and NE can contribute to cardiac hypertrophy seen in Nx animals. Furthermore, AKT (activated via α1A receptors), as well as increased α1A receptors and their agonist NE, might contribute to the observed hypertrophy.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Cardiovascular (CV) complications of renal failure are not infrequent in pediatric patients with end-stage renal disease (ESRD) [1, 2]. It has been reported that left ventricular hypertrophy arises and progresses in children during early stages of CKD [3]. Sympathetic tone is consistently raised in patients with ESRD, and CV mortality of these patients is dependent on the level of sympathetic nerve system (SNS) overactivity [4]. Studies in adult uremic rats have revealed that increased SNS activity can either decrease or have no effect on adrenergic receptors [5–7]. In the adult, β-adrenergic receptor blockade or the destruction of neuronal inputs to β-adrenergic receptors results in compensatory suprasensitivity of receptor signaling and eventually to upregulation of cell-surface receptors [8]. When these events are triggered in the developing organism, however, there is little or no increase in sensitivity or receptor numbers [9, 10]. Therefore, compared with augmented sympathetic activity in adults, increased sympathetic activity in postnatal organisms can produce markedly different qualitative and quantitative response. Furthermore, during the fetal and early postnatal periods, cardiomyocytes are actively proliferative. In rats, cardiomyocytes exit the cell cycle after the fourth to fifth day of life. The growth of cardiomyocytes then shifts from a predominant pattern of hyperplasia to one of hypertrophy [11]. However, sympathetic cardiac innervation becomes tonically active and responsive to reflex sympathetic stimulation during the second postnatal week [12]. The maturation of cardiac innervation plays several roles in the development of the heart. First, the final adjustments of β-receptor sensitivity are linked to the onset of tonic neuronal input [13]. Second, ontogeny of the myocardium itself is subject to autonomic influence [13]. Therefore, although myocyte proliferation ceases after a week, the autonomic influence on the heart continues for 2–3 weeks after birth. The proliferation of adult cardiomyocytes is limited and has only been reported in diseased hearts and under pathological conditions [14]. These facts underscore the observation that the mechanism(s) of adult cardiac hypertrophy versus those of the developing organism might be different but also that adrenergic receptor signaling may be altered (due to pathologic situations such as renal injury in early life), and this can affect cardiac growth. Most studies investigating the role of uremia on the adrenergic nervous system and cardiac hypertrophy have been conducted in adult rats [5, 6]. There is very little information exploring neonatal kidney injury and its effect on SNS and cardiac hypertrophy. Recognizing the pattern of these mechanistic changes will allow for better comprehension of the pathology and possibly treatment of cardiac hypertrophy in childhood uremia.
Cardiac hypertrophy is an adaptive condition frequently associated with contractility impairment, often leading to heart failure (HF) [15]. An increase in plasma catecholamines due to disturbances in biosynthesis or metabolism has been observed in uremic patients and animals [16], and sympathomimetics and norepinephrine (NE) infusion have been shown to cause cardiac hypertrophy [16, 17]. The mutation of norepinephrine transporter protein (NET) in humans is known to increase arterial NE concentrations as a function of decreased catecholamine clearance [18]. Catecholamines acting on α1-adrenergic receptors activate G alpha q (Gaq) signaling, promoting calcium (Ca2+) entry into intracellular compartments with cardiac hypertrophy and an increase in the levels of α1-adrenergic receptors during HF [19]. Elevated catecholamines cause cardiac hypertrophy via the β-adrenergic receptor signaling. However, sustained stimulation of β-adrenergic receptors leads to reduced cardiac function and development of HF [20]. In addition, catecholamine-induced cardiac hypertrophy is associated with reduced contractile responses to adrenergic agonists, an effect attributed to downregulation of myocardial β adrenoreceptors and desensitization by G-protein-coupled receptor kinase-2 (GRK2) [21, 22]. GRK2 is a member of the serine/threonine kinase family that phosphorylates β1- and β2-adrenergic receptor. GRK2 increase is associated with pressure-overload cardiac hypertrophy [23]. Moreover, GRK2 may be a key factor in the transition from hypertension-induced compensatory cardiac hypertrophy to HF [22]. Catecholamines are strong stimuli to activate GRK2 [24], and increased plasma NE seen in uremic patients and animals can promote GRK2 activity [5]. Finally, regulation of myocyte cell growth by G-protein-coupled receptors such as α- and β-receptor agonists involves a complex network of interacting pathways that activates key effector molecules found in the mitogen-activated protein (MAP) kinase pathway, phosphatidylinositol-3-OH kinase (PI3 kinase/AKT pathway)-dependent, protein kinase C (PKC)-dependant, protein kinase A (PKA)-dependent, and calcineurin-dependent pathways. Cardiac growth or hypertrophy can be physiological (as seen in athletes) or pathological as is seen disease state. In mice expressing dominant-negative PI3-kinase (PI-3 kinase/ AKT pathway) in the heart [25], exercise-induced (physiological) but not overload-induced (pathological) hypertrophy was impaired, suggesting that latter is mediated by other pathways such as extracellular signal-regulated kinase (ERK) [26].
We hypothesized that renal injury in early life can lead to high BP and elevated circulating catecholamines. Increased levels of catecholamines, such as NE, can act on cardiac adrenergic receptors to cause cardiac hypertrophy which may lead to HF. To investigate this matter we looked at biomarkers (NET and renalase) responsible for regulating the plasma concentration of catecholamines by affecting its metabolism. We also looked at the changes in adrenergic receptors (α and β) and GRK2 which not only can modulate β-adrenergic receptors but by itself can affect hypertrophy. Finally, we measured signaling markers AKT, implicated in physiologic cardiac growth and ERK, implicated in pathologic cardiac growth.
Materials and methods
Antirenalase polyclonal sera were generated by Proteintech Group, Inc. All other antibodies were obtained from Santa Cruz Biotechnology (Santa Cruz, CA, USA.).
Animals
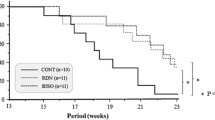
All animal procedures were approved by the Institutional Animal Care and Use committees of Virginia Commonwealth University. Rat pups were produced by timed-pregnancy mother rats acquired from Hilltop Laboratories (Scottdale, PA, USA). After birth, the pups from same mother were divided into three groups, with five animals in each group. The sham-surgery group (SH) was fed ad libitum. The nephrectomized (Nx) group was also fed as much food as they could consume. The amount of food consumed by each animal in these groups was quantitated daily. The pair-fed (PF) group received only as much food as its paired Nx rat consumed [1]. SH animals were subjected to sham operation and after weaning were given food and water ad libitum. After weaning PF animals were given the same amount of food as the Nx animals. The Nx animals underwent surgery, as described below.
Surgery
Chronic renal insufficiency was induced in rats by the method published previously by Krieg et al., with slight modification for neonatal animals [27]. Five-sixths (5/6) nephrectomy of neonatal rats was performed on rat pups 24–48 h old. Using sterile techniques, a left flank incision was made and the left kidney exposed. The upper and lower thirds of the kidney were ligated and excised so that one third of the mass of the left kidney remained. The muscle and skin incisions were sutured with 6–0 polypropylene suture. One week later, a right flank incision was made, and the right kidney was excised. Colodian was applied to the incisions, and the pups were placed on a heated pad to recover. Colodian is a colloidal substance that covers the incision site and surrounding area and protects it from being detected as a wound by the mother rat. This is necessary to protect the neonates from being rejected or destroyed by the mother rat. At 21 days of age, all pups were weaned and maintained for up to 9 weeks of age. At 8 weeks of age, the BP of the animals was recorded, and on the ninth week, the animals were sacrificed. Blood and tissue were collected for analysis of biomarkers.
Blood pressure
BP was measured by CODA 2 system (Kent Scientific Corporation, Torrington, CT, USA). CODA 2 utilizes volume pressure recording sensor technology to measure the rat tail BP. This is a computerized, noninvasive tail-cuff acquisition system that can simultaneously measure systolic, diastolic, and mean arterial BP without operator intervention. Animals were trained for 3 days and were kept in a restraining holder for 5–10 min. During this period, 25 sequential readings were obtained. Readings between 10 mmHg range were averaged. In this study, we report the mean arterial pressure of each group.
Immunoblotting
The heart was cut transversely and immediately frozen. The frozen heart was ground to a powder and then mixed in ice-cold phosphate-buffered saline (PBS) (pH 7.4) containing protease inhibitors and homogenized with a polytron homogenizer at 4°C. As low-speed spin employed in partial purification of receptors can lead to loss of receptors [28], we used total homogenates for receptor immunoanalysis. Cardiac homogenates (50–100 μg total protein) were separated on a 4–20% sodium dodecyl sulfate polyacrylamide gel electrophoresis (SDS-PAGE) gel, and proteins were transferred to a polyvinylidene difluoride (PVDF) membrane as described previously [29]. After being briefly washed in PBS containing 1% Tween-20 (PBS-T) and blocked in 5% nonfat dry milk, blots were incubated with appropriate antibodies in 5% nonfat dry milk overnight at 4°C. After being washed three to five times in PBS-T, blots were subsequently incubated with secondary antibody appropriately diluted in 5% nonfat dry milk for 1 h at room temperature. After being washed three to five times in Tris-buffered saline (TBS), blots were developed using Lightning Chemiluminescence Reagent Plus and exposed to X-ray film.
Quantitative real-time reverse transcriptase polymerase chain reaction (RT-PCR) analysis
Powdered heart was used to isolate the total ribonucleic acid (RNA), as described previously [30], except Trizol was used instead of guanidine isothiocyanate. Two micrograms of total RNA were reverse transcribed with a high-capacity complementary deoxyribonucleic acid (cDNA) reverse transcription kit (Applied Biosystems Inc., Foster City, CA, USA), and first-strand cDNA was used to perform real-time polymerase chain reaction (PCR) using Stratagene Mx3000p real-time PCR using TaqMan® universal PCR master mix, according to the manufacturer’s specifications (Applied Biosystems). The TaqMan probes and primers for β1-adrenergic receptor (assay identification number Rn00824536_s1), β2-adrenergic receptor (assay identification number Rn00560650_s1), α receptor 1A (assay identification number Rn 00567876_m1), α receptor 1B (assay identification number Rn01471343_m1), α receptor 1D (assay identification number Rn00577931_m1), GRK2 (assay identification number Rn00562822_m1), and β-actin (assay identification number Rn00667869_m1) were assay-on-demand gene-expression products (Applied Biosystems). The amount of messenger RNA (mRNA) was calculated by ΔΔCT method and normalized to β-actin.
Plasma catecholamines
At the time of death, trunk blood was obtained from the aorta and placed in prechilled tubes containing 10 mmol/L disodium ethylenediaminetetraacetic acid (EDTA). Plasma was processed for radioimmunoassay according to the published procedure of American Laboratory Products Company (ALPCO). In brief, the samples were extracted on a phenylsilylsilica column with methanol, and the eluant was dried and processed for radioimmunoassay using a specific antibody to NE and epinephrine (ALPCO).
Plasma urea nitrogen (PUN) and creatinine
Creatinine was measured by a NOVA16 autoanalyzer (NOVA Biomedical, Waltham, MA, USA). Plasma urea nitrogen (PUN) was determined using the enzymatic colorimetric method (Stanbio Lab, Boerne, TX, USA).
Statistical analysis
Statistical comparisons among groups were performed using analysis of variance (ANOVA) followed by Tukey’s multiple comparison test. Groups were considered to be significantly different with a p value ≤0.05.
Results
General characteristics, heart weight, blood pressure, and biochemical parameters
Table 1 describes general characteristics of BP and biochemical changes. The body weight of the SH group was significantly higher than the PF (p < 0.05) and Nx (p < 0.01) group. PF animals weighed significantly more than the Nx cohort (p < 0.01). The average total wet heart weight in rats from the SH, PF, and Nx groups are shown in Table 1. The heart weight of the PF animals was significantly lower than the SH (p < 0.01) and Nx (p < 0.05) animals. Total heart-weight to body-weight ratio was used as a marker for relative cardiac hypertrophy, and when the heart weight was corrected for the body weight, the heart-weight/body-weight ratio of the Nx cohort was 30% and 34% higher than the SH and PF (p < 0.001) groups, respectively, suggesting that Nx animals had hypertrophied hearts.
The mean arterial BP of the SH and PF groups was not significantly different, but the Nx animals had significantly higher BP (p < 0.001). Data in Table 1 shows that the Nx animals were uremic. PUN of Nx animals was more than tenfold higher than in SH and PF animals (p < 0.005), and plasma creatinine of the Nx group was four times higher than in SH and PF (p < 0.005) animals. Plasma NE concentrations of the Nx group were twofold higher than in the SH (p < 0.001) and PF (p < 0.01) groups, whereas cardiac NE was significantly lower than in the PF and SH (p < 0.05) groups. We did not observe any significant change in plasma epinephrine, but cardiac epinephrine concentrations in the Nx group were significantly lower than in the SH and PF (p < 0.05) groups.
Cardiac β-adrenergic receptors
Increased heart weight and increased plasma NE and BP seen in Nx rats are known to affect adrenergic receptors. In this study, we found that cardiac β1- and β2-adrenergic receptor mRNA did not significantly differ between SH, PF, and Nx rats (data not shown). However, as shown in the immunoblot analysis (Fig. 1a), β1-adrenergic receptors of Nx animals were 33% lower than in SH (p < 0.01) and 23% lower than in PF (p < 0.05) animals. Figure 1b shows that compared with the SH and PF groups, cardiac β2-adrenergic receptor protein expression of the Nx group was decreased by 25% and 22%, respectively (p < 0.05).
Relative levels of immunodetectable β1-receptor (a) and β2-receptor (b) protein from rat heart are compared in sham-operated (SH) animals (open bar), pair-fed (PF) animals (solid bar), and 5/6 nephrectomized (Nx) animals (hatched bar). β receptor protein expressions are expressed in arbitrary units. The upper panel shows the representative Western blot of β1 and β2 receptors normalized to GAPDH. The significant difference between Nx and the other two groups are depicted in the figure. SH and PF were not significantly different. Values are means ± SEM of 5 animals in each group
G-protein-coupled receptor kinase 2 (GRK2)
Therefore we investigated the effect of nephrectomy on GRK2 expression in the heart. As depicted in Fig. 2a, the GRK2 mRNA of SH and PF were not significantly different. The mRNA of the Nx group was more than 2 fold higher (p < 0.001) than SH and PF cohort. GRK2 protein expression of Nx group (Fig. 2b) was almost 2 fold higher than SH (p < 0.01) and 1.6 fold higher than PF (P < 0.05). The average GRK2 protein expression of PF was not significantly different than SH.
Levels of GRK2 mRNA (a) and immuno-detectable GRK2 (b) protein from rat heart are compared in sham-operated (SH) animals (open bar), pair fed (PF) animals (solid bar), and 5/6 nephrectomized (Nx) animals (hatched bar). GRK2 mRNA levels of PF and Nx group were compared relative to SH (100%). As shown in a, Nx animals had significantly higher mRNA compared with PF and SH groups. GRK2 of PF and SH were not significantly different. The upper panel of b shows the representative Western blot of GRK2 protein normalized to glyceraldehyde-3-phosphate dehydrogenase (GAPDH). The significant difference between Nx and the other two groups is depicted. SH and PF were not significantly different. Values are means ± standard error of mean (SEM) of five animals in each group
Cardiac α-adrenergic receptors
Compared with SH animals, Nx animals had fourfold higher α1A- and α1B-adrenergic receptor mRNA (p < 0.001, Fig. 3a,b). α-1A mRNA of Nx animals was threefold higher than in PF (p < 0.01) animals. The average of α1A and α1B mRNA of the PF group was not significantly different from the SH cohort (Fig. 3a,b). Immunoblot analysis of α receptor protein expression (Fig. 4a) showed that the Nx animals had a small (17%) but significantly higher (p < 0.05) expression of α1A-receptor protein. However, α1B-receptor protein expression was not significantly different between the groups. Cardiac α1D mRNA and protein expression of SH, PF, and Nx animals were not significantly different (data not shown).
Comparison of α1A-receptor messenger ribonucleic acid (mRNA) (a) and α1B-receptor mRNA (b) from rat heart in sham-operated (SH) (open bar), pair-fed (PF) (solid bar), and 5/6 nephrectomized (Nx) (hatched bar) animals. α-1A and 1B-receptor messenger ribonucleic acid (mRNA) levels of the PF and Nx groups were compared relative to the SH group (100%). As shown α1A- and α1B-receptor mRNA of the SH and PF groups were not significantly different, but mRNA of Nx animals was significantly higher than the PF and SH animals. Values are means ± standard error of mean (SEM) of five animals in each group
Relative levels of immunodetectable α1A-receptor (a) and α1B-receptor (b) protein from rat hearts are compared in sham-operated (SH) (open bar), pair-fed (PF) (solid bar), and 5/6 nephrectomized (Nx) (hatched bar) animals. α-1A and 1B-receptor protein expressions are expressed in arbitrary units. The upper panel shows the representative Western blot of α1A and α1B-receptors normalized to glyceraldehyde-3-phosphate dehydrogenase (GAPDH). Nx animals (a) had significantly higher α1A protein expression compared with SH and PF animals; however, α1B protein expression of Nx, PF, and SH animals (b) were not significantly different. Values are means ± standard error of mean (SEM) of five animals in each group
Norepinephrine transporter protein (NET) and renalase
NET plays a pivotal role in catecholamine clearance. As shown in Fig. 5a, the Nx group had a 22% and 19% lower NET protein expression than the SH and PF (p < 0.05) groups, respectively, although NET mRNA did not significantly differ between groups. Renalase is a recently discovered enzyme shown to metabolize catecholamine [31]. Renalase protein expression in the Nx group (Fig. 5b) was almost 37% and 39% lower than in the SH (p < 0.01) and PF (p < 0.01) groups, respectively, and renalase mRNA of the Nx group was 25% and 21% lower than in the SH and PF groups, respectively. The renalase protein expression and mRNA of the SH and PF groups was not significantly different.
Immuno-detectable norepinephrine transporter protein (NET) (a) and renalase (b) from rat heart were measured by Western blot. The upper panels of a and b show the representative Western blot of NET and renalase, respectively. Compared with sham-operated (SH) and pair-fed (PF) animals, the nephrectomized (Nx) cohort had significantly lower NET and renalase. Values are means ± standard error of mean (SEM) of five animals in each group
ERK and AKT
ERK and AKT play a central role in the signaling events leading to cardiac hypertrophy. Increased phosphorylations of these proteins are observed in cardiac hypertrophy. In this study, we measured the ratio of phosphorylated ERK (pERK)/total ERK and phosphorylated AKT (pAKT)/total AKT in cardiac tissue by Western blot. We observed no significant change of ERK and phosphorylated ERK proteins between groups (Fig. 6a). Although we found no significant change in AKT between groups, we saw an increase in AKT phosphorylation in Nx animals (Fig. 6b). As shown in Fig. 6b, Nx animals had significantly higher pAKT/AKT ratio compared with SH and PF groups (p < 0.05).
Comparisons of immunodetectable phosphorylated extracellular signal-regulated kinase (ERK) (pERK)/total ERK (a) and phosphorylated AKT (pAKT)/total AKT (b) from rat heart. The upper panels of a and b show the representative Western blot, and the bar graph is the ratio of phosphorylated ERK (pERK)/total ERK and phosphorylated AKT (pAKT)/total AKT. Nephrectomized (Nx) animals had significantly higher pAKT/AKT ratio compared with sham-operated (SH) and pair-fed (PF) groups. Values are means ± standard error of mean (SEM) of five animals in each group
Discussion
This study was designed to investigate the role of the adrenergic nervous system on the heart during neonatal uremia. Plasma creatinine and PUN were very high in Nx animals, clearly demonstrating their uremic condition. The Nx animals had decreased appetite, and both Nx animals and their PF controls had significantly lower body weight than SH controls. The heart weight of rat pups undergoing nephrectomy were significantly heavier than SH and PF rats. Increase in heart-weight to body-weight ratio is one of several ways to measure cardiac hypertrophy [32, 33]. When the heart weight was corrected for body weight, the heart-weight/body-weight ratios of SH and PF animals were not significantly different. But the heart-weight/body-weight ratios of Nx animals were significantly higher than both SH and PF groups (see Table 1). This was accompanied by increased BP and plasma NE. There is accumulating evidence demonstrating that cardiac hypertrophy is promoted by excess circulating catecholamine [34]. Indeed, circulating NE levels of Nx animals were significantly higher than the SH and PF controls. However, plasma tissue epinephrine did not change. Lower tissue NE of the Nx group observed in our study was similar to the observation made by other investigators in adult Nx animals [5, 35, 36]. Plasma NE is generally taken as an indicator of sympathetic activity [37, 38], and in humans, excess arterial NE can cause an increase in left ventricular (LV) mass [34]. Chronic infusion of NE in dogs raised the plasma NE, causing hypertrophy, although the ventricular NE was significantly lower than the control. In mice chronic infusion of α1 agonist (phenylephrine) caused increase in BP and pressure overload, resulting in cardiac hypertrophy [15]. Furthermore, activation of α1-adrenergic receptor in rat cardiomyocytes results in hypertrophy [39]. These studies suggest that an increase in circulating catecholamines or sympathomimetics can induce cardiac hypertrophy, irrespective of the cardiac NE. Therefore, excess circulating NE in conjunction with increased BP and increased α1-adrenergic receptor possibly contributed to the cardiac hypertrophy in this study.
In humans there is a profound decrease in cardiac β-adrenergic responsiveness with aging. This occurs by multiple mechanisms, including downregulation and decreased agonist binding of β1 receptors [40]. However, in rats, cardiac β receptor density does not change with age [41]. We observed significant downregulation of β1-adrenergic receptor protein, but β2-adrenergic receptors did not change. The decline in β receptors can be due to many reasons but not due to reduced gene expression of the protein, because mRNA expression was not altered between the groups. Catecholamine-induced cardiac hypertrophy is associated with reduced contractile responses to adrenergic agonists, an effect attributed to downregulation of myocardial β adrenoreceptors [21]. In subtotally Nx rats and uremic patients, a marked increase in LV mass is seen very early in the course of renal failure [42]. In adult Nx rats, Leineweber et al. [5] observed downregulation of LV β receptors but not right ventricular receptors. Downregulation of β-adrenergic receptors seen in this study can partially explain the β-adrenoceptor hypo-responsiveness seen in uremic patients and rats [5, 43].
G-protein-coupled receptors such as β-adrenergic receptors are regulated to ensure that uncontrolled stimulation will not occur, and in the heart, they are controlled by GRK2 [44]. One of the strongest stimuli to activate GRK2 is increased sympathetic activity [45], and the increased GRK2 found in this study can be attributed to increased adrenergic activity. GRK2 plays an active role in the downregulation of β-adrenergic receptor sensitivity [20]. Cardiac overexpression of the inhibitor of β-adrenergic receptor kinase (β-ARKct) which results in GRK2 inhibition, prevented cardiac hypertrophy and progressive deterioration in cardiac dysfunction [46]. Furthermore, enhancement of cardiac GRK2 is known to contribute to cardiac hypertrophy [20], and hypertrophied heart seen in Nx animals might be due to increased GRK2 expression. It is worthwhile to note that GRK2 also plays an important role in hypertension. Transgenic mice overexpressing GRK2 had significantly elevated BP [47]. It might be conjectured that hypertension seen in Nx rats may be associated with the elevated GRK2.
Unlike β-adrenergic receptors, α-adrenergic receptor density in the heart declines with age [48]. Compared with the SH and PF groups, α1A- and α1B-adrenergic receptor mRNA of Nx animals went up fourfold, whereas α1A-adrenergic protein increased by only 17% (p < 0.05). However, α1B-adrenergic protein expression did not change. It is not clear why there was inconsistency between α1A- and α1B-adrenergic messages and protein expression. Chalothorn et al. [49] using real-time imaging of living cells observed differences in the agonist-mediated internalization properties of the α1-adrenergic receptors. In agreement with previous work [50, 51], they observed that the α1B-adrenergic receptors underwent rapid agonist-mediated internalization. However, internalization occurred at a slower rate α1A-adrenergic receptors. We believe that the discrepancy between mRNA and protein expression might due to different degrees of receptor internalization. Upregulation of α1-adrenergic receptors observed in our study was also surprising, as plasma NE of Nx animals was significantly higher than animals in the SH and PF groups, and agonist mediated downregulation of adrenoreceptors is a more commonly encountered situation than an upregulation [52]. In addition, Meggs et al. [7] noted downregulation of α1-adrenoreceptors in adult uremic rats. It is not clear whether the observed dissimilarity is because of the difference in age group or due to cross-talk between β- and α-adrenergic receptors [53]. Akhter et al. suggested that downregulation of β-adrenergic receptors and upregulated GRK2 expression can cause increase in α1A and α1B receptors [53]. It is possible that the increase in receptor density observed in this study is a compensatory mechanism, especially as the β receptors were downregulated. Additionally, studies with isolated myocytes and rats have shown that α1A-adrenergic receptor is responsible for cardiac hypertrophy [39], and it is possible that the increased α1A-adrenergic receptor protein expression in association with increased circulating NE and that BP contributes to the cardiac hypertrophy observed in this study.
Increased plasma NE observed in our investigation may be due to increased sympathetic nerve activity, decreased NE uptake, and decreased metabolism of NE. Under normal conditions, approximately 80% of the NE released from vesicles in the neurons is taken up by the NET, and approximately 20% percent spills over into the circulation [18]. If the sympathetic activity is high, the spillover of catecholamine will be augmented. Although we did not measure sympathetic activity, others have reported increased sympathetic nerve activity in patients with renal failure [54]. In addition, a point mutation in the NET gene resulted in 98% loss in NET function and increased arterial NE in one patient. The increase in NE in this patient was due to decreased clearance of NE [18], which also reflects that decreased NET can result in increased circulating catecholamines. Cardiac NET expression of Nx rats was significantly lower than that of SH and PF control animals, which can explain the excess NE in the plasma of Nx rats. A decrease in NET density has been observed in adult uremic rats by other investigators [5]. Besides reduced uptake, decreased metabolism might contribute to the increase in plasma NE. Therefore, we looked into the catecholamine-metabolizing enzyme, renalase. Renalase is a relatively newly described enzyme shown to metabolize catecholamines and modulate BP [31]. Cardiac renalase in SH and PF rats was significantly higher than in Nx rats. Although the reason for this decrease is not clear, it can contribute to the reduced metabolism of catecholamines, resulting in increased spillover of NE in plasma. Furthermore, decreased clearance of catecholamines due to reduced uptake can lead to excess catecholamines in the circulation [18]. This is probably due to increased spillover of NE from tissue to the circulation. However, it does not explain why plasma epinephrine concentrations (although higher than in SH and PF animals) were not significantly different.
Both AKT and ERK pathways have been shown to play a significant role in cardiac hypertrophy [55]. Xiao et al. [56] provided evidence that the MEK/ERK pathway mediates hypertrophic effects of α1-adrenergic agonists in adult cardiomyocytes. In our study, we saw no change in total or phosphorylated ERK. However, the contribution of the ERK cascade to the induction of cardiac hypertrophy remains controversial [57, 58], with one study even suggesting that ERK signaling prevents hypertrophy [59]. Numerous lines of evidence show that AKT enhances heart size [60, 61]. Furthermore, in a recent study, it was shown that AKT can be activated via α1A receptors [62]. The increased α1A receptors and NE observed in our investigation might contribute to AKT-mediated hypertrophy.
In conclusion, we found that high BP in conjunction with circulating NE acting on α1A-adrenergic receptors is the probable cause of cardiac hypertrophy following renal injury in neonatal rats. The changes in β-adrenergic receptors, NET, and GRK2 resemble the changes in adult rats, but the changes in α1 receptors, especially α1A receptors, are unique to neonatal animals. Numerous studies have shown that downregulation of β receptors and upregulation of GRK2 are harbingers of HF [20, 22]. Furthermore, recent studies have shown that α receptors, especially α1A-adrenergic receptors, protect cardiac function [39, 63]. Additionally, AKT has been shown to play a more important role in physiological rather than pathological hypertrophy [26]. However, cardiac hypertrophy may be regarded as an adaptive response to increased work-load ventricular hypertrophy, especially when accompanied by prolonged periods of hypertension is associated with an increased incidence of HF [23]. In light of these contexts, is possible that the upregulation of α1A receptors seen in neonatal uremic rats is a compensatory mechanism against declining heart function rather than pathological occurrence. Further investigation is needed to clarify this phenomenon.
References
O’Regan S (1984) Cardiovascular abnormalities in paediatric patients with ESRD. In: Fine RN, Gruskin AB (eds) End-stage renal disease in children. Saunders, Philadelphia, pp 359–374
Scharer K, Ulmer HE (1985) Cardiovascular complications of renal failure. In: Holliday MA, Barratit TM, Vernier RL (eds) Pediatric nephrology (2nd edn). Williams and Wilkins, Baltimore, pp 887–896
Mitsnefes MM, Kimball TR, Kartal J, Witt SA, Glascock BJ, Khoury PR, Daniels SR (2006) Progression of left ventricular hypertrophy in children with early chronic kidney disease: 2-year follow-up study. J Pediatr 2149:671–675
Zoccali C, Mallamaci F, Parlongo S, Cutrupi S, Benedetto FA, Tripepi G, Bonanno G, Rapisarda F, Fatuzzo P, Seminara G, Cataliotti A, Stancanelli B, Malatino LS (2002) Plasma norepinephrine predicts survival and incident cardiovascular events in patients with end-stage renal disease. Circulation 105:1354–1359
Leineweber K, Heinroth-Hoffmann I, Pönicke K, Abraham G, Osten B, Brodde OE (2002) Cardiac beta-adrenoceptor desensitization due to increased beta-adrenoceptor kinase activity in chronic uremia. J Am Soc Nephrol 13:117–124
Mann JF, Jakobs KH, Riedel J, Ritz E (1986) Reduced chronotropic responsiveness of the heart in experimental uremia. Am J Physiol 250:H846–H852
Meggs LG, Ben-Ari J, Gammon D, Choudhury M, Goodman AI (1986) Effect of chronic uremia on the cardiovascular alpha 1 receptor. Life Sci 39:169–179
Kohout TA, Lefkowitz RJ (2003) Regulation of G protein-coupled receptor kinases and arrestins during receptor desensitization. Mol Pharmacol 63:9–18
Slotkin TA, Saleh JL, Zhang J, Seidler FJ (1996) Ontogeny of adrenoceptor/adenylyl cyclase desensitization mechanisms: the role of neonatal innervation. Brain Res 742:317–328
Garofolo MC, Seidler FJ, Auman JT, Slotkin TA (2002) Adrenergic modulation of muscarinic cholinergic receptor expression and function in the developing heart. Am J Physiol 282:R1356–R1363
Li F, Wang X, Capasso JM, Gerdes AM (1996) Rapid transition of cardiomyocytes from hyperplasia to hypertrophy during postnatal development. J Mol Cell Cardiol 28:1737–1746
Slotkin TA, Smith PG, Lau C, Bareis DL (1980) Functional aspects of development of catecholamine biosynthesis and release in the sympathetic nervous system. In: Parvez H, Parvez S (eds) Biogenic amines in development. Elsevier/North-Holland, Amsterdam, pp 29–48
Deskin R, Mills E, Whitmore WL, Seidler FJ, Slotkin TA (1980) Maturation of sympathetic neurotransmission in the rat heart. VI. The effect of neonatal central catecholaminergic lesions. J Pharmacol Exp Ther 215:342–347
Beltrami AP, Urbanek K, Kajstura J, Yan SM, Finato N, Bussani R, Nadal-Ginard B, Silvestri F, Leri A, Beltrami CA, Anversa P (2001) Evidence that human cardiac myocytes divide after myocardial infarction. N Engl J Med 344:1750–1757
Iaccarino G, Dolber PC, Lefkowitz RJ, Koch WJ (1999) Beta-adrenergic receptor kinase-1 levels in catecholamine-induced myocardial hypertrophy: regulation by beta- but not alpha1-adrenergic stimulation. Hypertension 33:396–401
Dhein S, Röhnert P, Markau S, Kotchi-Kotchi E, Becker K, Poller U, Osten B, Brodde OE (2000) Cardiac beta-adrenoceptors in chronic uremia: studies in humans and rats. J Am Coll Cardiol 36:608–617
Briest W, Rassler B, Deten A, Zimmer HG (2003) Norepinephrine-induced cardiac hypertrophy and fibrosis are not due to mast cell degranulation. Mol Cell Biochem 252:229–237
Shannon JR, Flattem NL, Jordan J, Jacob G, Black BK, Biaggioni I, Blakely RD, Robertson D (2000) Orthostatic intolerance and tachycardia associated with norepinephrine-transporter deficiency. N Engl J Med 342:541–549
Perrino C, Rockman HA (2007) Reversal of cardiac remodeling by modulation of adrenergic receptors: a new frontier in heart failure. Curr Opin Cardiol 22:443–449
Lohse MJ, Engelhardt S, Eschenhagen T (2003) What is the role of beta-adrenergic signaling in heart failure? Circ Res 93:896–906
Osadchii OE (2007) Cardiac hypertrophy induced by sustained beta-adrenoreceptor activation: pathophysiological aspects. Heart Fail Rev 12:66–86
Penela P, Murga C, Ribas C, Tutor AS, Peregrín S, Mayor F (2006) Mechanisms of regulation of G protein-coupled receptor kinases (GRKs) and cardiovascular disease. Cardiovasc Res 69:46–56
Choi DJ, Koch WJ, Hunter JJ, Rockman HA (1997) Mechanism of b-adrenergic receptor desensitization in cardiac hypertrophy is increased b-adrenergic receptor kinase. J Biol Chem 272:17223–17229
Leineweber K, Rohe P, Beilfuss A, Wolf C, Sporkmann H, Bruck H, Jakob HG, Heusch G, Philipp T, Brodde OE (2005) G-protein-coupled receptor kinase activity in human heart failure: effects of beta-adrenoceptor blockade. Cardiovasc Res 66:512–519
McMullen JR, Shioi T, Zhang L, Tarnavski O, Sherwood MC, Kang PM, Izumo S (2003) Phosphoinositide 3-kinase(p110a) plays a critical role for the induction of physiological, but not pathological, cardiac hypertrophy. Proc Natl Acad Sci USA 100:12355–12360
Wakatsuki T, Schlessinger J, Elson EL (2004) The biochemical response of the heart to hypertension and exercise. Trends Biochem Sci 29:609–617
Krieg RJ, Chan W, Lin KC, Kuemmerle NB, Veldhuis JD, Chan JC (2002) Growth hormone and growth hormone-related mRNA in uremic rats: effect of a growth hormone secretagogue. Pediatr Nephrol 17:585–590
Rocha-Singh KJ, Honbo NY, Karliner JS (1991) Hypoxia and glucose independently regulate the beta-adrenergic receptor-adenylate cyclase system in cardiac myocytes. J Clin Invest 88:204–213
Ghosh SS, Gehr TW, Ghosh S, Fakhry I, Sica DA, Lyall V, Schoolwerth AC (2003) PPARgamma ligand attenuates PDGF-induced mesangial cell proliferation: role of MAP kinase. Kidney Int 64:52–62
Ghosh S, Sica D, Schoolwerth AC, Quigg RJ, Haas M, Fakhry I, Gehr TW (2002) The role of the renin-angiotensin system in cholesterol and puromycin mediated renal injury. Am J Med Sci 324:296–304
Xu J, Li G, Wang P, Velazquez H, Yao X, Li Y, Wu Y, Peixoto A, Crowley S, Desir GV (2005) Renalase is a novel, soluble monoamine oxidase that regulates cardiac function and blood pressure. J Clin Invest 115:1275–1280
Yamaguchi N, Takahashi N, Xu L, Smithies O, Meissner G (2007) Early cardiac hypertrophy in mice with impaired calmodulin regulation of cardiac muscle Ca release channel. J Clin Invest 117:1344–1353
Callanan EY, Lee EW, Tilan JU, Winaver J, Haramati A, Mulroney SE, Zukowska Z (2007) Renal and Cardiac Neuropeptide Y (NPY) and NPY Receptors in a Rat Model of Congestive Heart Failure. Am J Physiol Renal Physiol 293:1811–1817
Strand AH, Gudmundsdottir H, Os I, Smith G, Westheim AS, Bjørnerheim R, Kjeldsen SE (2006) Arterial plasma noradrenaline predicts left ventricular mass independently of blood pressure and body build in men who develop hypertension over 20 years. J Hypertens 24:905–913
Rascher W, Schömig A, Kreye VA, Ritz E (1982) Diminished vascular response to noradrenaline in experimental chronic uremia. Kidney Int 1:20–27
Amann K, Rump LC, Simonaviciene A, Oberhauser V, Wessels S, Orth SR, Gross ML, Koch A, Bielenberg GW, Van Kats JP, Ehmke H, Mall G, Ritz E (2000) Effects of low dose sympathetic inhibition on glomerulosclerosis and albuminuria in subtotally nephrectomized rats. J Am Soc Nephrol 11:1469–1478
Goldstein DS (1988) Plasma catecholamines and essential hypertension: An analytical review. Hypertension 5:86–99
Esler M, Kaye D (2000) Measurement of sympathetic nervous system activity in heart failure: the role of norepinephrine kinetics. Heart Fail Rev 5:17–25
Woodcock EA (2007) Roles of a1a- and a1b-adrenoceptors in heart: insights from studies of genetically modified mice. Clin Exp Pharmacol Physiol 34:884–888
Anderson D, Campbell AM, Feldman M, White R, Roden W, Minobe MF, Khan P, Larrabee M, Wollmering JD, Port F (1994) Age-related changes in beta-adrenergic neuroeffector systems in the human heart. Circulation 90:1225–1238
Bazan A, Van de Velde E, Fraeyman N (1994) Effect of age on beta-receptors, Gs alpha- and Gi alpha- proteins in rat heart. Biochem Pharmacol 48:479–486
Tyralla K, Amann K (2003) Morphology of the heart and arteries in renal failure. Kidney Int 84:S80–S83
Ferchland A, Rettkowski O, Pönicke K, Deuber HJ, Osten B, Brodde OE (1998) Effects of uremic plasma on alpha- and beta-adrenoceptor subtypes. Nephron 80:46–50
Koch WJ (2004) Genetic and phenotypic targeting of beta-adrenergic signaling in heart failure. Mol Cell Biochem. 263:5–9
Brodde OE, Bruck H, Leineweber K (2006) Cardiac adrenoceptors: physiological and pathophysiological relevance. J Pharmacol Sci 100:323–337
Rockman HA, Koch WJ, Lefkowitz RJ (2002) Seven-transmembrane-spanning receptors and heart function. Nature 415:206–212
Eckhart AD, Ozaki T, Tevaearai H, Rockman HA, Koch WJ (2002) Vascular-targeted overexpression of G protein-coupled receptor kinase-2 in transgenic mice attenuates beta-adrenergic receptor signaling and increases resting blood pressure. Mol Pharmacol 61:749–758
Kimball KA, Cornett LE, Seifen E, Kennedy RH (1991) Aging changes in cardiac alpha 1-adrenoceptor responsiveness and expression. Eur J Pharmacol 208:231–238
Chalothorn D, McCune DF, Edelmann SE, García-Cazarín ML, Tsujimoto G, Piascik MT (2002) Differences in the cellular localization and agonist-mediated internalization properties of the alpha(1)-adrenoceptor subtypes. Mol Pharmacol 61:1008–1016
Fonseca MI, Button DC, Brown RD (1995) Agonist regulation of _1B-adrenergic receptor subcellular distribution and function. J Biol Chem 270:8902–8909
Wang J, Zheng J, Anderson JL, Toews ML (1997) A mutation in the hamster a1B-adrenergic receptor that differentiates two steps in the pathway of receptor internalization. Mol Pharmacol 52:306–313
Mahan LC, McKernan RM, Insel PA (1987) Metabolism of alpha- and beta-adrenergic receptors in vitro and in vivo. Annu Rev Pharmacol Toxicol 27:215–235
Akhter SA, Milano CA, Shotwell KF, Cho MC, Rockman HA, Lefkowitz RJ, Koch WJ (1997) Transgenic mice with cardiac overexpression of alpha1B-adrenergic receptors. In vivo alpha1-adrenergic receptor-mediated regulation of beta-adrenergic signaling. J Biol Chem 272:21253–21259
Augustyniak RA, Tuncel M, Zhang W, Toto RD, Victor RG (2002) Sympathetic overactivity as a cause of hypertension in chronic renal failure. J Hypertens. 20:3–9
Proud CG (2004) Ras, PI3-kinase and mTOR signaling in cardiac hypertrophy. Cardiovasc Res 63:403–413
Xiao L, Pimental DR, Amin JK, Singh KSDB, Sawyer DB, Colucci WS (2001) MEK1/2–ERK1/2 mediates a1-adrenergic receptor-stimulated hypertrophy in adult rat ventricular myocytes. J Mol Cell Cardiol 33:779–787
Kodama H, Fukuda K, Pan J, Sano M, Takahashi T, Kato T, Makino S, Manabe T, Murata M, Ogawa S (2000) Significance of ERK cascade compared with JAK/STAT and PI3-K pathway in gp130-mediated cardiac hypertrophy. Am J Physiol Heart Circ Physiol 279:H1635–H1644
Thorburn J, Frost JA, Thorburn A (1994) Mitogen-activated protein kinases mediate changes in gene expression but not cytoskeletal organisation associated with cardiac muscle hypertrophy. J Cell Biol 126:1565–1572
Silberbach M, Gorenc T, Hershberger RE, Stork PJ, Steyger PS, Roberts CT (1999) Extracellular signal-regulated protein kinase activation is required for the anti-hypertrophic effect of atrial natriuretic factor in neonatal rat ventricular myocytes. J Biol Chem 274:24858–24864
Condorelli G, Drusco A, Stassi G, Bellacosa A, Roncarati R, Iaccarino G, Russo MA, Gu Y, Dalton N, Chung C (2002) Akt induces enhanced myocardial contractility and cell size in vivo in transgenic mice. Proc Natl Acad Sci USA 99:12333–12338
Matsui T, Li L, Wu JC, Cook SA, Nagoshi T, Picard MH, Liao R, Rosenzweig A (2002) Phenotypic spectrum caused by transgenic overexpression of activated Akt in the heart. J Biol Chem 277:22896–22901
Guo J, Sabri A, Elouardighi H, Rybin V, Steinberg SF (2006) Alpha1-adrenergic receptors activate AKT via a Pyk2/PDK-1 pathway that is tonically inhibited by novel protein kinase C isoforms in cardiomyocytes. Circ Res 99:1367–1375
O’Connell TD, Swigart PM, Rodrigo MC, Ishizaka S, Joho S, Turnbull L, Tecott LH, Baker AJ, Foster E, Grossman W, Simpson PC (2006) Alpha1-adrenergic receptors prevent a maladaptive cardiac response to pressure overload. J Clin Invest 116:1005–1015
Acknowledgement
This work is supported by the Jeffress Foundation.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Ghosh, S.S., Krieg, R.J., Sica, D.A. et al. Cardiac hypertrophy in neonatal nephrectomized rats: the role of the sympathetic nervous system. Pediatr Nephrol 24, 367–377 (2009). https://doi.org/10.1007/s00467-008-0978-8
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00467-008-0978-8