Abstract
Hypertension is frequent in pediatric patients receiving dialysis, with an especially high rate reported in children on hemodialysis (HD). We performed the present study to assess blood pressure (BP) status and identify risk factors for poor BP control in children on maintenance HD. One month’s dialysis records were collected from 71 subjects receiving HD in ten dialysis units participating in the Midwest Pediatric Nephrology Consortium (MWPNC). For each HD session, data on pre- and posttreatment weights and BPs were recorded. Hypertension, defined as mean BP ≥ 95th percentile, was found in 42 (59%) subjects. Eleven subjects (15.5%) had prehypertension, defined as mean BP between the 90th and 95th percentiles, while 18 subjects (25.3%) had normal BP (<90th percentile). BP significantly decreased at the end of a dialysis session; however, only 15 of 42 hypertensive subjects (35%) normalized their BP. Hypertensive subjects were younger (p = 0.03), had higher serum phosphorus (p = 0.01), and had more elevated posttreatment weight above estimated dry weight (p = 0.02). Logistic regression showed that younger age (p = 0.02) and higher serum phosphorus (p = 0.02) independently predicted hypertensive status. In conclusion, this study emphasizes the difficulty of BP control in pediatric HD patients. Especially poor BP control was found in younger children; those patients who do not reach their posttreatment weight goals, perhaps reflecting their hypervolemic state; and those who have higher serum phosphorus levels.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Hypertension is a frequent complication in adults on maintenance hemodialysis (HD), with a prevalence of 55–75% [1–3]. In these patients, hypertension is a leading risk factor for cardiovascular disease and has been shown to be independently associated with morbidity and mortality [4]. As in adults, pediatric patients on maintenance dialysis have a high prevalence of hypertension [5, 6]. A recent analysis of data from the North American Pediatric Renal Transplant Cooperative Study (NAPRTCS) determined that a majority of patients on maintenance dialysis required antihypertensive medications, yet 51% of patients still had hypertension after 1 year of dialysis therapy [6]. Associated risk factors for hypertension included young age, acquired etiology of kidney failure, and African American race. This study also determined that children on HD were more likely to have hypertension than children on peritoneal dialysis. The reason for higher hypertension prevalence in children on HD is unclear. Unfortunately, the NAPRTCS database does not collect information on HD adequacy or overall volume status, nor does it include information on nephrectomy status, classes of antihypertensive medications, or standard monthly laboratory monitoring data.
Therefore, we performed the present study to determine the prevalence of hypertension in children on maintenance HD, to assess the adequacy of treatment of these hypertensive patients, and to identify the risk factors for poor blood pressure (BP) control in this population.
Materials and methods
Subjects
This is a retrospective cross-sectional analysis of data collected from pediatric patients receiving maintenance HD. Ten pediatric dialysis units from the Midwest Pediatric Nephrology Consortium (MWPNC) participated in the study. The Institutional Review Board of each participating center approved the study. All children and adolescents receiving maintenance HD for a minimum of 4 weeks prior to study initiation were eligible to participate. Exclusion criteria included patients older than 21 years and patients receiving less than thrice weekly (12 sessions in 1 month) HD. Eligibility was determined by the coinvestigator at each participating institution.
Charts were reviewed for baseline patient demographic information, which included gender, race, height, age at initiation of dialysis, age at current treatment, history of prior kidney transplant, and etiology of kidney failure. Congenital etiologies included obstructive uropathies, renal dysplasia, cystic diseases, reflux nephropathy, and congenital nephrotic syndrome. Acquired causes included focal sclerosis, systemic lupus, other glomerulonephritides, vasculitides, and typical hemolytic uremic syndrome (HUS). Additionally, history of prior nephrectomy and number and type of antihypertensive medications prescribed at the time of data collection were documented.
Monthly laboratory data collected included hematocrit, serum calcium and phosphorus, parathyroid hormone, bicarbonate, and albumin levels. In the event of multiple laboratory values during the month of interest, e.g., weekly hematocrit in patients on noninvasive volume monitoring (NIVM), the laboratory value on the day that complete laboratory values were obtained was used in our analysis. All hematocrits were determined from laboratory evaluation of drawn blood and were not estimated from NIVM. Dialysis adequacy and its method of determination, as calculated by the individual institutions, were also collected with the monthly data.
HD treatments
One month’s dialysis records were collected for each patient. For most participating institutions, data were collected for the month of September 2004; however, institutions with delay in local institutional study approval collected data from the most current complete month following approval. For each of 12 consecutive HD sessions, data collected included pre- and posttreatment systolic (SBP) and diastolic (DBP) BPs, pre- and posttreatment weight, estimated dry weight (EDW), and use of NIVM. For the first HD session, prior posttreatment weight was also collected. EDW was determined by the individual nephrologist managing HD. The main criteria used to estimate dry weight were absence of symptoms of excess fluid removal, such as cramping and hypotension, in combination with postdialysis BP readings and nutritional assessment. NIVM was used only for secondary confirmation of excess dry weight at all but one participating center. Subjects were considered to have regular NIVM if 50% or more of their dialysis sessions were performed using the monitor.
Mean values for each of the pre- and posttreatment BPs and weights were calculated. For sessions in which there were missing data points, mean values of those variables were calculated over the remaining sessions. In the event that EDW was changed during the month, mean EDW was calculated for values over the entire month. Average interdialytic weight gain (IWG) was calculated from the difference between mean pretreatment weight and mean posttreatment weight from the prior HD session. Average ultrafiltrate (UF) was calculated from the difference between mean pretreatment weight and mean posttreatment weight. Average excess weight was calculated from the difference between mean posttreatment weight and mean EDW.
Normalized values for IWG, UF, and excess weight were also calculated for each subject by dividing their mean values by the subject’s EDW and then multiplying by 100. To further evaluate whether any differences in these values could be attributed to the longer interdialytic period associated with weekends, comparisons were also made of these values at the first treatment of the week and the midweek treatment. The midweek treatment was defined as the very next treatment following the first treatment of the week.
BP calculations and categorization
Measurement of BP was performed by the standard routine used by each dialysis center. All participating centers obtained BP via the automated cuff on the dialysis machine. Predialysis BP was obtained while the subject was seated prior to the initiation of HD. Half of the participating centers obtained the postdialysis BP during the blood rinse phase near the conclusion of dialysis while the remaining centers obtained readings approximately 10 min after the conclusion of the treatment, including completion of rinse back and decannulation. BP status was defined based on the Fourth Report on the Diagnosis, Evaluation and Treatment of High Blood Pressure in Children and Adolescents [7]. In order to directly compare BP readings across all subjects, BP was adjusted for body size. The calculated mean BP values were divided by the age, gender, and height-specific 95th percentiles for both SBP and DBP to give the SBP and DBP index for each subject. Hypertension was defined as mean BP ≥95th percentile or SBP or DBP index greater than or equal to 1. Patients were classified as nonhypertensive if their BP indices were less than 1. Nonhypertensive subjects were further subdivided as having normotension, defined as mean BP <90th percentile, and prehypertension, defined as mean BP between the 90th and 95th percentile. As with the HD parameters, the BP parameters were also compared for the first of the week and midweek treatments.
Statistical methods
Analysis of differences between pre- and posttreatment BP indices was performed using paired t testing. To analyze the difference between hypertensive and nonhypertensive subjects (predialysis BP values only), t test and Mann–Whitney rank sum test were used for continuous variables, and the chi-square test was used for categorical variables. P values less than 0.05 were considered statistically significant. Multivariable logistic regression was performed to determine the independent predictors for hypertension, which was the dichotomous dependent variable. Independent variables with p values less than 0.2 from the univariate analyses were entered into the logistic regression. SigmaStat software, version 3.1, was used to perform the analysis.
Results
Study population
Data were obtained on 71 subjects from the ten pediatric dialysis centers. Number of subjects from each individual center ranged from three to 15. Demographic characteristics of the overall group are shown in Table 1. A majority of subjects were male (54%), African American (54%), and had an acquired etiology of their kidney failure (55%). Age at time of study ranged from 26 to 242 (mean 161) months, and time on dialysis ranged from 1 to 160 (mean 27) months. Twenty-two subjects (31%) had a previous kidney transplant, with three of these subjects having repeated transplants. Seventeen subjects (24%) had a prior nephrectomy.
Hypertension control
Fifty-one of 71 subjects (72%) were prescribed antihypertensive medications. Despite the use of medications, hypertension was still present in 42 subjects (59%). Isolated systolic hypertension was prevalent in 13 of these 42 subjects, and isolated diastolic hypertension was prevalent in just one subject. The majority of hypertensive subjects had both SBP and DBP elevation. Nine of the 42 hypertensive subjects were prescribed no antihypertensive medications whereas 33 subjects remained hypertensive despite having a prescribed antihypertensive regimen. Prehypertension was present in 11 subjects (16%), with 6 of these subjects having been prescribed antihypertensive medications. Eighteen subjects (25%) were normotensive, with 12 of these subjects having been prescribed antihypertensives; and only 6 subjects had normal BP without requiring antihypertensives.
Both SBP and DBP significantly decreased following dialysis sessions (Table 2). Only 15 of the 42 hypertensive subjects improved posttreatment so that they were no longer considered hypertensive: nine of those 15 patients were normotensive (BP < 90th percentile), and six remained prehypertensive following dialysis. Three patients who were normotensive before treatments became hypertensive. Hypertensive subjects had a significant difference in change in BP following treatments when compared with nonhypertensive patients: mean change in SBP was 12.6 ± 10.2 mmHg in hypertensive subjects vs. 2.3 ± 10.3 mmHg in nonhypertensive subjects (p < 0.001) whereas the mean change in DBP was 8.5 ± 9.0 mmHg vs. 0.6 ± 7.6 mmHg (p < 0.001).
Comparisons were also made between first of the week and midweek treatments (Table 2). There were no significant differences between first of the week and midweek BP indices either pre- or postdialysis (all p values >0.1). The prevalence rate of hypertension was also similar when comparing values from the first of the week versus midweek. These rates were slightly higher, but not statistically different, than the overall prevalence rates.
The use of BP medications in hypertensive and nonhypertensive subjects was compared (Table 3). Hypertensive subjects on medications were prescribed an average of 2.30 antihypertensives whereas nonhypertensive subjects were prescribed 1.39 medications. The most commonly used antihypertensives in both groups were calcium channel blockers, angiotensin-converting enzyme inhibitors, and angiotensin receptor blockers.
Risk factors for hypertension
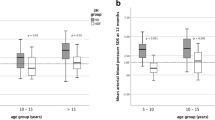
Comparisons of the demographic, laboratory, and clinical parameters between hypertensive and nonhypertensive groups are shown in Tables 4, 5, and 6. Hypertensive subjects were younger at the time of the study (p = 0.025);however, they were not younger at the time of initiation of dialysis (Table 4). There were no significant differences between groups by race, gender, time on dialysis, etiology of kidney failure, transplant, or nephrectomy status. Hypertensive subjects had significantly higher serum phosphorus levels (p = 0.014), but there were no differences in other monthly laboratory values (Table 5). Hypertensive subjects also had significantly higher average excess weight postdialysis (p = 0.022), which became more significant when normalized to EDW (p = 0.008). There was a trend toward an increased normalized IWG in hypertensive patients, but it only reached statistical significance for the midweek normalized IWG (p = 0.03). There were no differences between groups in UF or dialysis adequacy (Table 6).
Multivariate logistic regression analysis showed that younger age (β = −0.013, p = 0.015) and higher serum phosphorus level (β = 0.32, p = 0.016) independently predicted hypertensive status. The odds ratio for age in months was 0.987 (confidence interval 0.976–0.997) and for serum phosphorus 1.377 (1.062–1.786).
Discussion
The results of this multicenter study show that children on maintenance HD have poorly controlled BP. Recent Kidney/Dialysis Outcomes Quality Initiative (K/DOQI) Clinical Practice Guidelines on Hypertension and Antihypertensive Agents in Chronic Kidney Disease recommend target BP in children to be lower than the 90th percentile for normal values adjusted for age, gender, and height [8]. In our study, the prevalence of hypertension was nearly 60%. Of patients prescribed antihypertensive medications, only one third had BP below the 95th percentile, and a mere 12 patients (23.5%) achieved adequate BP control goals below the 90th percentile as defined by the K/DOQI guidelines. These data are consistent with the findings from the NAPRTCS study, in which only 33% of patients on antihypertensive medications were able to achieve BP below the 95th percentile [6]. However, data from that study were collected from 1992 to 2004. Our study shows that since the time period of the NAPRTCS data collection, starting one decade ago, the rates of hypertension have not changed, and the vast majority of pediatric patients on maintenance HD are not achieving recommended target BP levels.
The use of mean values for BP for determination of hypertension is potentially susceptible to influence by extreme values and, therefore, may be a less robust method for determining hypertension. Some of the potential influence of single abnormal BP readings should be offset by the use of 1 month’s BP readings, as 1 month of BP readings have been compared with ambulatory BP monitoring in terms of accuracy of hypertension diagnosis [9]. Analysis of our hypertensive and nonhypertensive groups in terms of overall frequency of elevated BP readings showed that hypertensive subjects had a substantially greater number of hypertensive readings predialysis for SBP (median 10 vs. 2, p <0.001) and DBP (8.5 vs. 1, p <0.001). There were similar differences in frequencies of postdialysis SBP and DBP elevations (7.5 vs. 2 and 4.5 vs. 0, p <0.001, respectively). Therefore, the differences seen in mean BP between the two groups in this study cannot be attributed to a single extreme BP value.
Improvements in BP readings postdialysis were generally seen in our subjects, with significant decrease in both SBP and DBP. However, two thirds (27 of 42) of hypertensive subjects continued to have elevated BP following dialysis. This percentage is significantly higher than the European data reported more than a decade ago by Loirat et al. [10] in which only 15% of pediatric HD patients remained hypertensive immediately following treatment. The authors concluded that volume overload was the main cause of hypertension in their population. Our results would concur with that assertion.
Although we found no significant differences in UF between groups, there was a trend toward differences in IWG between hypertensive and nonhypertensive patients, especially during the midweek treatment. Consequently, hypertensive patients had a significantly higher excess weight (above EDW) following HD compared with nonhypertensive patients (0.57 kg vs. 0.21 kg, p = 0.022). These findings become even more significant when looking at normalized excess weight (p < 0.01), and they held consistent both for treatments at the beginning of the week and at midweek. This difference in excess volume is noteworthy, as adult studies have shown that hypertensive patients have increased volume sensitivity when compared with their normotensive counterparts [11]. Our findings would indicate that chronic fluid overload might be the significant cause of poor BP control in pediatric HD patients and that circumspect achievement of dry weight may be the most important factor in controlling hypertension.
One established method for better estimation of dry weight is the use of noninvasive hematocrit monitoring (NIVM) [12]. We found wide variation in its use among centers. Therefore, no meaningful conclusions could be reached in our attempt to analyze the associations between use of NIVM and BP control.
Our study also showed that hypertension was more prevalent in younger patients. This is consistent with previous NAPRTCS data [6]. One explanation has been decreased rates of prescribing antihypertensive medications in younger children. Our results showed that 65% of hypertensive subjects <12 years of age were on antihypertensive medications whereas 88% of hypertensive subjects >12 years of age were being treated, but this difference was not significant (p = 0.16). Another possible explanation is that in younger children, with continued growth, it is more difficult to estimate true dry weight and to actually reach EDW. In our study, percent excess weight above EDW in younger patients was twice that in older patients (2.7% vs. 1.7%), though this difference was not statistically significant. Multivariate logistic regression showed that younger age was an independent predictor of hypertensive status. So, whereas excess weight gain may be a contributing factor, it may not be the sole cause of increased risk of hypertension in younger patients.
Lastly, our study results showed a significantly higher serum phosphorus level among hypertensive subjects. This difference in serum phosphate levels was not secondary to the younger age of our hypertensive subjects, as the difference persisted if serum phosphate was normalized to age-based standard values (p = 0.04, data not shown). This finding is consistent with other studies, which have shown higher BP associated with hyperphosphatemia [13]. Etiologic theories have mainly centered on hyperphosphatemia contributing to secondary hyperparathyroidism and increased calcium entry to vascular-wall smooth-muscle cells [14]. In vitro studies have found increased calcification with dose-dependent phosphate levels [15]. We, however, found no association between hypertension and serum calcium or parathyroid hormone levels in our subjects. Therefore, the association between hyperphosphatemia and hypertension also exists in pediatric HD patients, just as it does in adult patients; however, further research is needed to find the causative link between these two conditions.
There are limitations to this multicenter study. With ten different participating institutions, standardization of measures across all subjects was not attempted, as it was an observational study analyzed retrospectively. Variation in methods for BP measurements and determination of EDW could have significant influence on the results. The analysis of oscillometric BP readings, even though hypertension was defined by standards for auscultatory BP measures, is a potential limitation, as oscillometric BP readings tend to be higher when compared with auscultated readings. However, many multicenter studies of chronic HD patients have shown the association between predialysis BP and cardiovascular morbidity using either oscillometric measures or the routine measures, likely oscillometric, of the participating individual dialysis centers [3, 16–18]. Likewise, automated oscillometric sphygmomanometers have been shown to correlate with auscultatory-determined SBP, with a correlation coefficient (r value) of 0.98 [19].
The difference in timing for obtaining postdialysis BP likely affects the prevalence of postdialysis hypertension. BPs obtained later after dialysis would allow for repletion of the intravascular volume and are less likely to be elevated from renin mediation. Therefore, dialysis centers that measured postdialysis BPs 10 min after completion of all treatment may have lower rates of postdialysis hypertension. However, as our primary outcome of hypertension was defined by predialysis BP, this difference in timing does not affect our overall hypertension prevalence but may influence our estimates of how well BP is lowered by HD treatment.
Another limitation of this nonstandardization is different times of the week when hematocrits were checked in this study. Four participating centers, accounting for 23 of the total 71 subjects, obtained their monthly laboratory values on the first day of dialysis each week. Hence, the hematocrit could be falsely lowered in these subjects than what would be measured if checked later in the week, as excess fluid may decrease these measures. A comparison of hematocrit values between those checked at the beginning of the week versus those checked midweek showed no difference (34.4 ± 4.8 vs. 35.5 ± 4.7 gm/dl, p = 0.37), and these 23 subjects were distributed between the hypertensive (15 of 23 subjects, 65%) and nonhypertensive (35%) group, much like the overall study population.
Although the number of subjects in this study is relatively large for a pediatric HD population, we were unable to assess the efficacy of individual antihypertensive medication classes on controlling hypertension because of a significant variability in their use. A recent European study analyzed the antihypertensive dosing in 130 pediatric dialysis patients [17]. The range of weight-based dosing of different antihypertensives was reported for their overall group; however, no comparison of these values was made between hypertensive and nonhypertensive subjects. It is likely that the study’s reported variation in antihypertensive class use did not allow for sufficiently powered analysis, as well. Nonadherence with BP medications was not evaluated in this study, which could have significant impact on the prevalence of hypertension.
Our study has some common pitfalls that are found in many observational multicenter studies, primarily that of nonstandardization of techniques at all centers. However, because this study did not attempt to alter the routines of each center, it might be a better reflection of the true clinical practices taking place.
References
Mittal SK, Kowalski E, Trenkle J, McDonough B, Halinski D, Devlin K, Boylan E, Flaster E, Maesaka JK (1999) Prevalence of hypertension in a hemodialysis population. Clin Nephrol 51:77–82
Cheigh JS, Milite C, Sullivan JF, Rubin AL, Stenzel KH (1992) Hypertension is not adequately controlled in hemodialysis patients. Am J Kidney Dis 19:453–459
Salem MM (1995) Hypertension in the hemodialysis population: a survey of 649 patients. Am J Kidney Dis 26:461–468
Tomita J, Kimura G, Inoue T, Inenaga T, Sanai T, KawanoY, Nakamura S, Baba S, Matsuoka H, Omae T (1995) Role of systolic blood pressure in determining prognosis of hemodialyzed patients. Am J Kidney Dis 25:405–412
Lerner GR, Warady BA, Sullivan EK, Alexander SR (1999) Chronic dialysis in children and adolescents. The 1996 annual report of the North American Pediatric Renal Transplant Cooperative Study. Pediatr Nephrol 13:404–417
Mitsnefes M, Stablein D (2005) Hypertension in pediatric patients on long-term dialysis: a report of the North American Pediatric Renal Transplant Cooperative Study (NAPRTCS). Am J Kidney Dis 45:309–315
(2004) The fourth report on the diagnosis, evaluation, and treatment of high blood pressure in children and adolescents. Pediatrics 114:555–576
National Kidney Foundation (2004) K/DOQI clinical practice guidelines on hypertension and antihypertensive agents in chronic kidney disease. Am J Kidney Dis 43:S1–S290
Zoccali C, Mallamaci F, Tripepi G, Benedetto FA, Cottini E, Giacone G, Malatino L (1999) Prediction of left ventricular geometry by clinic, predialysis and 24-h ambulatory BP monitoring in hemodialysis patients: CREED investigators. J Hypertens 17:1751–1758
Loirat C, Ehrich JH, Geerlings W, Jones EH, Landais P, Mallick NP, Margreiter R, Raine AE, Salmela K, Selwood NH, Tufveson G, Valderrabano F (1994) Report on management of renal failure in children in Europe, XXIII, 1992. Nephrol Dial Transplant 9(Suppl 1):26–40
Ventura JE, Sposito M (1997) Volume sensitivity of blood pressure in end-stage renal disease. Nephrol Dial Transplant 12:485–491
Michael M, Brewer ED, Goldstein SL (2004) Blood volume monitoring to achieve target weight in pediatric hemodialysis patients. Pediatr Nephrol 19:432–437
Marchais SJ, Metivier F, Guerin AP, London GM (1999) Association of hyperphosphataemia with haemodynamic disturbances in end-stage renal disease. Nephrol Dial Transplant 14:2178–2183
Horl MP, Horl WH (2002) Hemodialysis-associated hypertension: pathophysiology and therapy. Am J Kidney Dis 39:227–244
Jono S, McKee MD, Murry CE, Shioi A, Nishizawa Y, Mori K, Morii H, Giachelli CM (2000) Phosphate regulation of vascular smooth muscle cell calcification. Circ Res 87:E10–E17
Rahman M, Fu P, Sehgal AR, Smith MC (2000) Interdialytic weight gain, compliance with dialysis regimen, and age are independent predictors of blood pressure in hemodialysis patients. Am J Kidney Dis 35:257–265
Tkaczyk M, Nowicki M, Balasz-Chmielewska I, Boguszewska-Baczkowska H, Drozdz D, Kollataj B, Jarmolinski T, Jobs K, Kilis-Pstrusinska K, Leszczynska B, Makulska I, Runowski D, Stankiewicz R, Szczepanska M, Wiercinski R, Grenda R, Kanik A, Pietrzyk JA, Roszkowska-Blaim M, Szprynger K, Zachwieja J, Zajaczkowska MM, Zoch-Zwierz W, Zwolinska D, Zurowska A (2006) Hypertension in dialysed children: the prevalence and therapeutic approach in Poland-a nationwide survey. Nephrol Dial Transplant 21:736–742
Lopez-Gomez JM, Villaverde M, Jofre R, Rodriguez-Benitez P, Perez-Garcia R (2005) Interdialytic weight gain as a marker of blood pressure, nutrition, and survival in hemodialysis patients. Kidney Int Suppl S63–S68
Cavalcanti S, Marchesi G, Ghidin C (2000) Validation of automated oscillometric sphygmomanometer (HDBPM) for arterial pressure measurement during haemodialysis. Med Biol Eng Comput 38:98–101
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
VanDeVoorde, R.G., Barletta, G.M., Chand, D.H. et al. Blood pressure control in pediatric hemodialysis: the Midwest Pediatric Nephrology Consortium Study. Pediatr Nephrol 22, 547–553 (2007). https://doi.org/10.1007/s00467-006-0341-x
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00467-006-0341-x