Abstract
The standard renoprotection is based on the inhibition of the renin-angiotensin system (RAS) by angiotensin convertase inhibitors (ACEi) or angiotensin II receptor 1 blockers (AT1B). The aim of our study was to analyze the effects of the addition of AT1B to ACEi-based renoprotection in children with chronic kidney disease. We examined 11 children with a mean age of 10.5 years (range, 0.5–18 years) with a mean glomerular filtration rate (GFR) of 61±61 ml/min/1.73 m2. In four patients, the primary renal disease was hemolytic uremic syndrome, in three congenital nephrotic syndrome (CNS), in two reflux nephropathy, prune-belly syndrome in one and acute cortical necrosis in one. All patients were treated with complex hypotensive ACEi-based therapy. AT1B losartan was added in a mean dose of 0.9 mg/kg/day. The change in GFR, proteinuria and blood pressure at two 12-month intervals before and after adding AT1B was compared. The results showed that during the 12 months preceding AT1B therapy, there was no change in blood pressure and proteinuria, but the GFR declined in 7 of 11 patients. After the 12th month of add-on therapy with AT1B, there was a significant decrease in both absolute and indexed blood pressure values. Proteinuria decreased in eight patients, did not change in one and increased in two, including one with CNS. The GFR stabilized or increased in eight patients and decreased in three patients with CNS. In 7 of 11 patients, there was a significant, but not threatening increase in serum potassium. In conclusion, add-on renoprotection with AT1B added to ACEi is safe and significantly improves the renoprotective effects of ACEi treatment in children with progressive nephropathies, including patients with advanced CKD.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The standard hypotensive and renoprotective therapy is based on the inhibition of the renin-angiotensin system (RAS) by angiotensin convertase inhibitors (ACEi) or angiotensin II receptor 1 blockers (AT1B) [1]. Although hypotensive effects of ACEi in children with chronic kidney disease (CKD) are well described, there are only a few reports describing the renoprotective effects of ACEi in children [2, 3]. Classically, the use of ACEi and AT1B together is avoided, as their undesired common side effects, such as hyperkalemia and a further decrease of the glomerular filtration rate, are regarded as important contraindications to combined therapy. However, both drugs have been successfully combined together in adults with arterial hypertension and normal renal function, and recently as renoprotective drugs in adults with non-diabetic CKD [4–6]. The rationale for a double blockade of RAS with ACEi and AT1B is a demand for better blood pressure control and avoidance of the so-called “escape phenomenon” observed in patients in whom ACEis are used as the exclusive renoprotecive drugs [7]. Combining drugs was reported to be more effective than increasing the dose of ACEi [8]. Both kinds of drugs can be used in combination either from the start of renoprotective therapy or as sequential therapy when the second drug is added, while the effect of ongoing monotherapy is unsatisfactory.
Below we describe our preliminary experience with the addition of AT1B to hypotensive and renoprotective ACEi-based treatment in 11 children and adolescents with CKD.
Patients
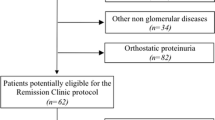
Eleven patients, 5 girls and 6 boys with a mean age of 10.5 years (range, 0.5–18 years) with CKD in stages 5 to 1, were included in the study. The causes of CKD were hemolytic uremic syndrome (HUS) in four cases, congenital nephrotic syndrome (CNS) in three, reflux nephropathy (RN) in two, prune-belly syndrome in one and acute cortical necrosis in one case. All patients were under our care since the diagnosis of the disease and were treated with on average 2.4 (1–5) hypotensive drugs, including ACEi, calcium channel blockers, beta-blockers and diuretics (Table 1). All but one patient had proteinuria despite treatment with ACEi. Despite full doses of hypotensives, blood pressure values were above the 50th percentile for age and sex, and proteinuria tended to increase. The mean glomerular filtration rate (GFR) measured as creatinine clearance was 61±61 ml/min/1.73m2 and ranged from 14 (patient 4) to 156 ml/min/1.73m2 in the case of 4-year-old girl with CNS (patient 7). The mean 24-h proteinuria was 1.2 (0–4) g/day and was the greatest in two siblings with CNS (patients 6 and 7).
Because of insufficient blood pressure control and/or proteinuria, the AT1B losartan (Xartan, Adamed) was given in one daily dose of 0.9 (0.5–2) mg/kg as an additional hypotensive and renoprotective drug. The clinical and laboratory data of the patients are shown in Table 1.
Methods
The glomerular filtration rate (GFR) was estimated from the creatinine clearance calculated from 24-h urine collection using Jaffe reaction. Proteinuria was also estimated as 24-h urine excretion, and urinary protein was determined using the Exton method. In the youngest children (patients 8 and 11), 24-h urine collection was made using a special bag.
Blood pressure was measured with the oscillometric method using a calibrated oscillometric Dinamap device during 2-month ambulatory visits. The average value from three measurements was noted. Blood pressure was expressed as absolute values of systolic (SBP) and diastolic (DBP) blood pressure and as the blood pressure index (SBPi and DBPi, respectively).The reference normative blood pressure values were those published in the Fourth Task Force Report in 2004 [9].
Patients were followed at 2-month intervals for 2 years. Laboratory data obtained during the ambulatory visits or hospital stays at the 12th month before the start of AT1B (−12), at the start of AT1B (0) and after 12 months of therapy with AT1B (+12) were analyzed. The rate of GFR decline was calculated as the difference between the GFR value obtained at two 12-month intervals, i.e., 12 months before introducing AT1B (−12 visit) and the GFR value at the start of AT1B therapy (0 visit) and between the GFR value at the 12th month (+12) and at the start of the losartan therapy (0). The same was calculated for the change in proteinuria. There were no changes in the drug therapy other than the hypotensive agents.
Statistical analysis
Analyzed variables were the GFR, proteinuria, absolute and indexed blood pressure values, serum potassium levels and change in GFR, proteinuria and blood pressure expressed as the difference between two values obtained at 12-month intervals. The Wilcoxon paired t-test was used, and a P value less than 0.05 was regarded as significant.
Results
Blood pressure values and the results of renal function tests noted before (−12), at the start (0) and after 12 months (+12) of AT1B treatment are shown in Tables 1 and 2. In 7 of 11 patients, the GFR declined during the 12 months preceding the introduction of losartan, in three patients GFR was stable, and in one it increased by 1 ml/min/1.73m2. The mean decline in GFR during the preceding 12 months was –4.8±4.9 ml/min/1.73m2.
On average, the indexed values of SBP and DBP at –12 and 0 points were 1.01±0.12 vs. 1.01±0.11 (n.s.) and 0.90±0.20 vs. 0.95±0.20 (n.s.). The mean change in daily proteinuria was 0.35 (range: −0.5−2.4) g/day and was not significant. Proteinuria increased in five patients, decreased in two and remained stable in four patients. The serum potassium concentration did not change significantly.
At the 12th month after the introduction of AT1B treatment, the mean number of hypotensives prescribed was significantly greater at 3.3 (1–6) vs. 2.4 (1–5) (P=0.001). In all patients, there was a significant decrease of blood pressure expressed both as absolute SBP (124±16 vs. 115±15 mmHg; P=0.006), indexed SBP (1.01±0.11 vs. 0.94±0.10; P=0.004), absolute DBP (73±15 vs. 60±18 mmHg; P=0.01) and indexed DBP (0.95±0.20 vs. 0.76±0.23; P=0.012) (Figs. 1 and 2).
In eight patients, the GFR increased or stabilized. The GFR lowered only in three patients with CNS (patients 6, 7 and 11) (Table 2, Fig. 3). On average, there was no change in the comparison of mean GFR values (56±46 vs. 49±28 ml/min/1.73 m2, n.s.) and in ΔGFR at two 12-month study periods (−4.8±4.9 vs. −7.4±21 ml/min/1.73 m2, n.s.). When three patients with CNS were excluded from the analysis, there was a significant difference in the comparison of the mean GFR values before and after the addition of losartan (40±22 vs. 42±20 ml/min/1.73 m2, P=0.02) and significant slowing of the rate of CKD progression expressed as ΔGFR before (−4.6±5.0 ml/min/1.73 m2) and after 12 months of treatment with losartan (2.8±2.7 ml/min/1.73 m2) (P=0.02).
Proteinuria decreased in 8 of 11 patients, did not change in 1 and increased in 2, including 1 patient with CNS (Fig. 4). On average, there was no change in daily proteinuria (1.6 range: 0–4 vs. 1.16 range: 0–6.3 g/day, n.s.). However, when the change in proteinuria during the preceding 12 months was compared, there was a significant difference between the two study periods (0.35, range: −0.5–2.4 vs. −044, range: −2.2−2.3, g/day, P=0.02). There was no correlation between the change in blood pressure and proteinuria and between the change in blood pressure and the change in GFR.
In 7 of 11 patients there was a significant increase in serum potassium concentrations after the introduction of AT1B treatment, and on average serum potassium rose from 4.3±0.3 at the 0 to 5.0±0.7 at the +12 visit (P=0.03).
There were no adverse events noted such as cough, edema or a rash during the entire observation period.
Seven patients were observed longer than 12 months after the introduction of losartan. In two patients with CNS, there was fast progression towards renal failure. In the other five patients, including patients with HUS, reflux nephropathy and acute cortical necrosis, the course of CKD was stable during at least the next 12 months of observation (Table 2).
Discussion
The main result of our study is the observation that a dual blockade of the RAS system with ACEi and AT1B in children with CKD, even in an advanced stage, is safe, causes a significant decrease in blood pressure and proteinuria and slows the GFR decline. The main weak point of our study is the low number of patients included. Therefore, these results must be regarded so far as a preliminary observation. Secondly, the observed group was heterogenous in terms of the stage of CKD, as two patients had GFR above 100 ml/min/1.73 m2, as well as of the primary cause of CKD.
Renoprotective therapy has a well-documented place in the complex conservative treatment of patients with CKD. However, the published data on the effects of renoprotection were based on the results of trials involving adult patients. The main differences between adults and children include the etiology of CKD and influence of physiological development and puberty. There are only a few studies of the renoprotective effects of a RAS blockade in children [2, 10–12]. Data published by Lama et al. on the beneficial effects of ACEi in children with reflux nephropathy strongly indicate that renoprotection is effective in children [2]. However, it seems that in congenital degenerative nephropathies such as Alport syndrome the effects of RAS inhibition are negligible in terms of slowing the GFR decline [13]. In others, such as Finnish-type congenital nephritic syndrome, the antiproteinuric effect seems to depend on the type of mutation and concomitant therapy with indomethacin and unilateral nephrectomy [13–15]. However, the real renoprotective effect of a RAS blockade on slowing the GFR decline in CNS patients is unknown.
In practice, renoprotection is based on ACEi and AT1B alone or in combination with other hypotensive drugs. There are some reports on the antiproteinuric and hypotensive effect of AT1B in children with CKD and good renal function (stage 1) [16] and in children with more advanced CKD (stages 2–3) [17]. The efficacy of a dual blockade of RAS in adult patients with CKD was documented in the COOPERATE study [5, 6]. The renoprotective and hypotensive effects of a dual RAS blockade in children were reported in children with IgA nephropathy and relatively good renal function [18, 19]. Potential further deterioration of the GFR and hyperkalemia may be of concern in the cases of patients with CKD who have low or normal blood pressure and low GFR. In our patients, blood pressure values were above the 50th percentile, and in five of them well above the 95th percentile. In five patients, the main indication to add the AT1B was uncontrolled blood pressure, and consequently the patients with high blood pressure benefited most from this treatment, both in terms of the hypotensive effect and renoprotection. It seems interesting that we observed a beneficial effect of the dual blockade in patients who because of low GFR values might be disqualified from most trials with classic renoprotective therapy (patients 2, 3 and 4). However, there are some reports that both enalapril and benazepril used in adults with non-diabetic CKD in stage 4 and GFR below 30 ml/min/1.73 m2 exerted significant antiproteinuric and renoprotective effects [20, 21].
As expected, we have observed a significant rise in the serum potassium concentration despite concomitant diuretic use; however, except in one patient, this was not in a too seriously threatening range. This adverse side effect may be of real concern, especially in patients with the lowest GFR values and in the youngest children. It underlines the necessity for close monitoring of patients treated with combined renoprotective therapy.
The other issue is the problem of the dosing of AT1B in children with CKD. We used the dose extrapolated from those used in adult patients, and it was on average 1 mg/kg/day. In the study by Ellis et al., the authors suggested the use of losartan in a dose of 0.8 mg/kg/day, which was extrapolated from those used in adults [16]. The dose used by us was also in the range suggested by others as effective and safe in the treatment of hypertensive children [22]. However, recently there were some reports on the beneficial effects of super high doses of AT1B in adult patients with diabetic nephropathy and preserved GFR [23].
The relatively short time of our observation and small number of patients make it difficult to draw firm conclusions on the long-term efficacy of the renoprotective effect of the dual blockade of RAS. Besides three patients with CNS, the addition of AT1B led not only to a significant decrease of blood pressure, but it also decreased proteinuria and at least stabilized GFR. The long-term effects of the achieved decrease in proteinuria are uncertain. Preliminary results of the ESCAPE study indicate that ACEi treatment efficiently lowers blood pressure in children with CKD [10], but after 3 years in some patients, there is an increase in protein excretion despite good blood pressure control (F. Schaefer, personal communication). This observation indicates that the hypotensive effect of RAS blockers can be dissociated from the renoprotective effect and is similar to that described in previously published conclusions [5, 6]. Our results suggest that the addition of AT1B may be beneficial in cases of escape phenomenon from the renoprotective effect of ACEi.
In conclusion, the presented clinical observation suggests that in children with CKD aready treated with ACEi and who are still hypertensive or proteinuric, the addition of AT1B leads to a significant improvement in blood pressure control, stabilizes or decreases proteinuria and can arrest CKD progression. The best results were seen in patients who were severely hypertensive. The other conclusion that seems important from the practical point of view is that such treatment was safe and efficacious even in patients with advanced CKD (stage 4).
References
Del Vecchio L, Locatelli F (2001) The renoprotective effect of combined antihypertensive drugs. J Nephrol 14:7–14
Lama G, Salsano ME, Pedulla’ M, Grassia C, Ruocco G (1997) Angiotensin converting enzyme inhibitors and reflux nephropathy: a 2-year follow-up. Pediatr Nephrol 11:714–718
Trachtman H, Gauthier B (1988) Effect of angiotensin-converting enzyme inhibitor therapy on proteinuria in children with renal disease. J Pediatr 112:295–298
Ruilope LM, Aldigier JC, Ponticelli C, Oddou-Stock P, Botteri F, Mann JF (2000) Safety of the combination of valsartan and benazepril in patients with chronic renal disease. European Group for the Investigation of Valsartan in Chronic Renal Disease. J Hypertens 18:89–95
Nakao N, Seno H, Kasuga H, Toriyama T, Kawahara H, Fukagawa M (2004) Effects of combination treatment with losartan and trandolapril on office and ambulatory blood pressures in non-diabetic renal disease: a COOPERATE-ABP substudy. Am J Nephrol 24:543–548
Nakao N, Yoshimura A, Morita H, Takada M, Kayano T, Ideura T (2003) Combination treatment of angiotensin-II receptor blocker and angiotensin-converting-enzyme inhibitor in non-diabetic renal disease (COOPERATE): a randomised controlled trial. Lancet 361:117–124
Shiigai T, Schichiri M (2001) Late escape from the antiproteinuric effect of ACE inhibitors in nondiabetic renal disease. Am J Kid Dis 37:477–483
Kincaid-Smith P, Fairley KF, Packham D (2004) Dual blockade of the renin-angiotensin system compared with a 50% increase in the dose of angiotensin-converting enzyme inhibitor: effects on proteinuria and blood pressure. Nephrol Dial Transplant 19:2272–2274
National High Blood Pressure Education Program Working Group on High Blood Pressure in Children and Adolescents (2004) The fourth report on the diagnosis, evaluation and treatment of high blood pressure in children and adolescents. Pediatrics 114:555–576
Wuhl E, Mehls O, Schaefer F; ESCAPE Trial Group (2004) Antihypertensive and antiproteinuric efficacy of ramipril in children with chronic renal failure. Kidney Int 66:768–776
Van Dyck M, Proesmans W (2004) Renoprotection by ACE inhibitors after severe hemolytic uremic syndrome. Pediatr Nephrol 19:688–690
Litwin M (2004) Risk factors for renal failure in children with non-glomerular nephropathies. Pediatr Nephrol 19:178–186
Adler L, Mathew R, Futterweit S, Frank R, Gauthier BG, Kashtan CE, Trachtman H (2002) Angiotensin converting enzyme inhibitor therapy in children with Alport syndrome: effect on urinary albumin, TGF-beta and nitrite excretion. BMC Nephrol 3:2
Holmberg C, Trygvasson K, Kestila MK, Jalanko HJ (2004) Congenital nephrotic syndrome. In: Avner ED, Harmon WE, Niaudet P (eds) Pediatric nephrology, 5th edn. Lippincot Wiliams & Wilkins, pp 503–516
Hamed RM, Shomaf M (2002) Congenital nephritic syndrome: a clinico-pathological study of 30 children. J Nephrol 14:104–109
Ellis D, Moritz ML, Vats A, Janosky JE (2004) Antihypertensive and renoprotective efficacy and safety of losartan. A long-term study in children with renal disorders. Am J Hypertens 17:928–935
Gartenmann AC, Fossali E, von Vigier RO, Simonetti GD, Schmidtko J, Edefonti A, Bianchetti MG (2003) Better renoprotective effect of angiotensin II antagonist compared to dihydropyridine calcium channel blocker in childhood. Kidney Int 64:1450–1454
Tanaka H, Suzuki K, Nakahata T, Tsugawa K, Konno Y, Tsuruga K, Ito E, Waga S (2004) Combined therapy of enalapril and losartan attenuates histologic progression in immunoglobulin A nephropathy. Pediatr Int 46:576–579
Yang Y, Ohta K, Shimizu M, Nakai A, Kasahara Y, Yachie A, Koizumi S (2005) Treatment with low-dose angiotensin-converting enzyme inhibitor (ACEI) plus angiotensin II receptor blocker (ARB) in pediatric patients with IgA nephropathy. Clin Nephrol 64:35–40
Ihle BU, Whitwirth JA, Shahinfar S, Cnaan A, Kincaid-Smith PS, Becker GJ (1996) Angiotensin-converting enzyme inhibition in non-diabetic progressive renal insufficiency: a controlled double-blind trial. Am J Kidney Dis 27:489–495
Hou FF, Zhang X, Zhang GH, Xie D, Chen PY, Zhang WR, Jiang JP, Liang M, Wang GB, Liu ZR, Gang RW (2006) Efficacy and safety of benazepril for advanced chronic renal insufficiency. N Eng J Med 354:131–140
Shahinfar S, Cano F, Sofffer BA, Ahmed T, Santoro EP, Zhang Z, Gleim G, Miller K, Vogt B, Blumer J, Biezogounov J (2005) A double-blind, dose-response study of losartan in hypertensive children. Am J Hypertens 18:183–190
Rossing K, Schjoedt KJ, Jensen BR, Boomsma F, Parving HH (2005) Enhanced renoprotective effects of ultrahigh doses of irbesartan in patients with type 2 diabetes and microalbuminuria. Kidney Int 68:1190–1198
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Litwin, M., Grenda, R., Śladowska, J. et al. Add-on therapy with angiotensin II receptor 1 blocker in children with chronic kidney disease already treated with angiotensin-converting enzyme inhibitors. Pediatr Nephrol 21, 1716–1722 (2006). https://doi.org/10.1007/s00467-006-0223-2
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00467-006-0223-2