Abstract
Since few data are available about factors affecting renal maturation especially in the lower gestational ages (G.A.), the aim of this work was to study postnatal renal function in a representative population sample of preterm newborns (G.A. ≤36 weeks), admitted to the neonatal intensive care units of seven Italian hospitals, in order to investigate a possible role of drugs, therapeutic interventions and diseases. Data were collected through detailed questionnaires including maternal and neonatal information. To test renal function, serum creatinine and urine output were regularly recorded every 3 days throughout the 1st month of life. A total of 246 subjects were enrolled in the study and divided into four groups according to G.A.: group A, 22–25 weeks; group B, 26–28 weeks; group C, 29–32 weeks; group D, 33–36 weeks. Serum creatinine concentrations at birth were similar in all four groups, while significant differences were evident from the 3rd to the 21st day of life. Within each group, two subpopulations were identified taking into account creatinine values. In subjects with serum creatinine concentrations within the normal range, a physiological decline in creatinine values was observed with increasing postnatal age, and an inverse correlation between creatinine and G.A. was evident from the 3rd day of life to the end of the study period. In neonates with impaired renal function, a marked increase in creatinine values was observed in all neonates from the 3rd day of life, with significant differences among groups on days 7 and 10. Whereas many risk factors were correlated (univariate analysis) with impaired renal function, the multivariate analysis identified only five factors as independent: maternal consumption of nonsteroidal anti-inflammatory drugs (NSAIDs) during pregnancy [odds ratio (OR): 7.38, 95% confidence interval (CI) 3.26–16.7] and intubation at birth (OR: 4.39, 95% CI: 1.2–16.3) were the main risk factors. Respiratory distress syndrome, a low Apgar score and ibuprofen treatment of the neonate were identified as additional risk factors. Our data confirm a multifactorial origin of acute renal impairment in newborns. It is of note that pharmacological treatment with NSAIDs during pregnancy may negatively influence neonatal renal function.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Under normal conditions, the early neonatal period is characterized by a rapid maturation of kidney function, brought about mainly by haemodynamic factors such as cardiac output, vascular resistance and mean arterial blood pressure. In preterm newborns, the anatomical and functional immaturity is even more important, especially in neonates with low gestational age (G.A.) and birth weight (B.W.), where glomerular filtration and renal plasma flow values are related, in terms of the nephrogenesis process, in a directly proportional manner to G.A. [1].
In the phase of adaptation to extrauterine life, the homeostatic regulation of the organism is transferred from placenta to kidney, which particularly in preterm newborns shows a reduced functionality due to either low levels of glomerular filtrate or tubular immaturity [2]. The newborn kidney’s main physiologic limitation is its very low glomerular filtration rate (GFR), maintained by a delicate balance between vasoconstrictor and vasodilatory renal forces. The low GFR of the newborn kidney, sufficient for growth and development under normal conditions, limits the postnatal renal functional adaptation to endogenous and exogenous stress. This adaptation becomes even more problematic in preterm infants of lower G.A., where multiple factors affecting renal function occur in combination [3]. So, the kidney is at risk of imbalance under all non-physiological conditions leading to hypoxia, hypotension and hypovolaemia which may be responsible for the initial phase of renal impairment mainly mediated by haemodynamic factors [1]. Moreover, a variety of therapeutic interventions and the administration of vasoactive or nephrotoxic drugs may have harmful renal consequences [2]. Iatrogenic complications include a reduction of renal perfusion (prerenal failure) or damage to renal parenchyma (intrinsic renal failure), frequently reversible if diagnosed early.
The particular vulnerability of the neonatal kidney to drugs is ascribed mainly to its specific anatomic-functional characteristics, its excretory and detoxifying role, its high blood flow, the high degree of specialization of the tubular cells and its extensive capillary surface area [2]. On the one hand, drug-induced renal toxicity seems less common and severe in the newborn: the reasons could be multiple, including less sensitivity to toxic agents, less uptake of drugs by the proximal tubule because of incomplete maturation and greater “renal volume to body volume” ratio [4]. However, this issue is controversial and, on the other hand, neonatal status may be considered itself a risk factor for drug-induced nephrotoxicity, since newborns, particularly prematures, receive a number of drugs in the first days of life that might have short-term effects on renal structure and function. This result is particularly important as regards very low birth weight (VLBW) infants, whose percentage of survival has increased in recent years, contributing to a rise in the number of subjects experiencing renal impairment, mainly acute renal failure (ARF) [5].
Briefly, in this work we report data referring to a representative population of preterm newborns in the attempt to study their postnatal renal function in the 1st month of life in relation to the influence that could be exerted by some diseases, drug treatments and other therapeutic interventions.
Methods
Study population
The study population included all hospitalized preterm newborns with a G.A. ≤36 weeks receiving care at the neonatal intensive care units (NICUs) of seven Italian hospitals after the approval of the Ethic Committees during a 3-year period (March 2000-March 2003). Neonates were enrolled after written informed consent was obtained from their parents. Neonates with evidence of congenital structural renal diseases or other major anomalies (e.g. congenital heart diseases) were excluded. Other criteria for exclusion were impossibility to obtain information about mothers or to collect urine samples throughout the study period.
Data collection
Data were collected through a detailed 74-item questionnaire especially designed for this study, comprising various information about newborns and mothers, and entered into a computerized relational database (Microsoft Access). For each newborn demographic characteristics (B.W., G.A., sex, Apgar scores), biologic data (blood pressure, respiratory status, routine laboratory assays, radiologic examinations), clinical outcomes diagnosed or suspected (anoxia, respiratory distress syndrome, patent ductus arteriosus, bronchopulmonary dysplasia, intraventricular haemorrhage, necrotizing enterocolitis, sepsis) and all therapeutic interventions (catheters, intubation, phototherapy) were recorded. Moreover, any information about drugs administered was collected (dose, intervals, route of administration, duration of treatment).
Mothers were interviewed by a trained physician within a few days after the delivery. Women were asked a number of questions related to previous obstetric history (contraception, fertility treatments, antenatal care), to their pregnancy (smoking, caffeine and alcohol consumption, medical complications) and to intrapartum risk factors (fever, premature rupture of membranes, type of delivery), with particular attention given to drugs taken during pregnancy and delivery. Information was also collected about sociodemographic variables (age, number of children, employment) and any family history of acute and chronic diseases, in particular those related to renal function.
Renal function
To test renal function during the observational period, serum creatinine levels (Crs) and urine output were measured and regularly recorded every 3 days throughout the 1st month of life in order to obtain information about renal postnatal maturation or development of pathological problems.
Crs concentrations were analyzed on the basis of a modified kinetic Jaffe reaction method validated previously as having minimal interference from noncreatinine chromogens such as bilirubin (Synchron LX Systems, Beckman Coulter, Fullerton, CA, USA). Daily urine collections were made via a bladder catheter, if positioned, or through an external collecting device: urine loss was controlled by weighing diapers.
Moreover, newborns underwent postnatal renal sonography examinations to evaluate the size, structure and echogenicity of the kidneys.
Statistical analysis
Statistical analysis was performed using the Statistical Package for Social Sciences for Windows (SPSS Inc., Chicago, IL, USA). Univariate analysis was performed to identify differences among the four groups of neonates and, within each group, between subjects with normal or pathological Crs values: the analysis of variance (ANOVA) test (continuous data) or the Pearson χ2 test (categorical variables) was used as appropriate and statistical significance required a p value ≤0.05. Odds ratio (OR) and 95% confidence interval (CI) were calculated. Variables that the univariate analysis showed to be significant were entered into a stepwise logistic regression model.
Results
Study population
During the study period, 281 preterm neonates (G.A. ≤36 weeks) admitted to our NICUs were involved in the research: six subjects were excluded due to the impossibility to collect information about mothers, five because of major anomalies and the parents of four newborns refused participation. Another 20 preterm infants were excluded: they were transferred elsewhere or urine samples were not obtained as required. So, 246 subjects were enrolled in the study and divided into four groups according to G.A.: group A, 22–25 weeks; group B, 26–28 weeks; group C, 29–32 weeks, group D, 33–36 weeks.
The main characteristics of preterm infants (demographic data, pathologies and therapeutic interventions influencing renal function) are summarized in Table 1. All the diseases diagnosed and the therapeutic interventions applied to our preterm infants were inversely correlated with the gestational age of the subjects (p<0.001 for all examined parameters, except as regards NEC: p=0.019).
Drugs administered to our neonates are shown in Table 2: according to different G.A., doses and intervals followed international guidelines and were standardized in NICUs participating in this research. Instead, differences were evident among the four groups as regards the percentage of drugs administered. Compared to the other three groups, neonates of group D received a lower percentage of antibiotics such as aminoglycosides and penicillins, ibuprofen, furosemide, dopamine and steroids and these differences were all highly statistically significant (p<0.001) except as regards cephalosporins (p=0.053).
Maternal information
The average age of the mothers was 32.02±3.62 years. Maternal pathologies included premature rupture of membranes (PROM) (59/246, 23.98%), pre-eclampsia (31/246, 12.79%) and fever (27/246, 10.98%). The incidence of caesarean section was 62.6% (154/246) and a statistically significant difference was evident among groups, with a higher incidence in mothers of VLBW infants (χ2=15.35, p=0.002); 17 of 246 mothers (6.91%) had acute or chronic renal pathologies.
Therapies during pregnancy included tocolytics (43/246, 17.48%), antibiotics (35/246, 14.23%), NSAIDs (47/246, 19.11%) and antenatal steroids (44/246, 17.89%). Some statistically significant differences were found among the four groups. Mothers of groups A and B neonates had a higher percentage of PROM and fever during pregnancy (χ2=15.11, p=0.002 and χ2=19.72, p<0.001, respectively). Moreover, more antibiotics and tocolytics were taken during pregnancy (χ2=14.71, p=0.003 and χ2=15.25, p=0.002, respectively). As regards drugs administered to the mothers during the delivery, the only significant difference regarded antibiotics given in a greater amount to mothers of groups A and B neonates (χ2=14.58, p=0.003).
Renal function
As reported in Table 3, no differences at birth were observed among our four groups as regards Crs values, while significant differences were evident from the 3rd to the 21st day of life. A peak in Crs values was reached at the 3rd day in groups A, B and C: the rise was greatest in the more premature neonates (mean Crs in group A: 115.8 μmol/l). In Group D concentrations progressively decreased from birth to the end of the study period. Kidney sizes were within normal range for size and shape. A greater percentage of oliguria, even if not significant, was observed in group A (8 vs 4, 3 and 1%, respectively, in the other three groups) together with significant differences in relation to medullary hyperechogenicity observed with postnatal ultrasonography (24 vs 13, 11 and 7%, p=0.044). A mild urinary tract dilatation (pyelectasis) was evident in 11 newborns distributed among the four groups.
By a careful analysis of Crs data, within each group we identified two subpopulations of neonates: subjects with Crs concentrations within the normal range and subjects with pathological values. In these newborns a diagnosis of ARF was made on the following basis: Crs concentrations at the 60th h of life or later ≥114.9 μmol/l or ≥88.4 μmol/l, respectively, in subjects with a G.A. < or ≥33 weeks and/or presence of oliguria (urine output <1 ml/kg per h) [1, 6].
As shown in Fig. 1, in neonates with normal renal function, with increasing postnatal age a physiological decline in Crs values was observed that extended over 2–3 weeks in our preterm infants, with an inverse correlation between Crs and G.A. (r=−0.317, p<0.001) and with significant differences among groups observed from the 3rd day of life to the end of the study period (p<0.001 for each examined day), where a value of 38.9 μmol/l was reached in neonates of group D. In neonates with a lower G.A. (group A) after an initial increase in Crs concentrations, the values decreased much slower and remained higher at the 28th day (56.6 μmol/l). In neonates with impaired renal function, a marked increase in Crs values was observed in all groups from the 3rd to the 10th day of life, with significant differences among groups on day 7 (p=0.030) and day 10 (p=0.006). Then, values decreased but remained higher, compared to subjects with normal renal function, in all neonates at the 28th day of life.
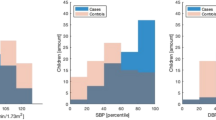
Finally, a relationship is evident between G.A. and the percentage of neonates with impaired renal function (χ2=25.71, p<0.001): 56% of neonates in group A had impaired renal function, while in group D only 15% had Crs values considered pathological (Fig. 2).
Statistical analysis
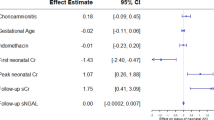
From the analysis of all maternal and neonatal factors that could have influenced renal function in the first days of life, some interesting and significant differences were evident in groups A and D. As regards preterm newborns with the lower G.A., we found significant differences in neonates with impaired renal function, compared to those with normal function, in relation to phototherapy (95 vs 63%, χ2=6.42, p=0.011) and ibuprofen treatment (78 vs 45%, χ2=4.51, p=0.034). If we compare neonates with normal and impaired renal function of group D, maternal NSAID consumption during pregnancy (46 vs 7%, χ2=12.39, p<0.001), intubation at birth (62 vs 8%, χ2=19.91, p<0.001), umbilical artery catheterization (54 vs 15%, χ2=7.58, p=0.006), Apgar score <7 at 5 min (38 vs 5%, χ2=9.88, p=0.002) and RDS (85 vs 24%, χ2=15.78, p<0.001) were significantly different. Moreover, drugs were administered in a greater amount to neonates with impaired renal function: statistically significant differences were evident as regards antibiotics (85 vs 35%, χ2=9.39, p=0.002), in particular aminoglycosides (62 vs 23%, χ2=6.43, p=0.011). Taking into account G.A. as controlling factor, the results of the univariate analysis with the relative OR and 95% CI are shown in Table 4. The multivariate logistic regression analysis included all variables with a significance of p<0.05 for univariate analysis (intubation at birth, umbilical artery catheterization, mechanical ventilation, low Apgar score, RDS, maternal NSAIDs and ibuprofen given to newborns). Maternal NSAIDs (OR: 7.38, 95% CI: 3.26–16.7) and intubation at birth (OR: 4.39, 95% CI: 1.2–16.3) were associated with the greatest risk for impaired renal function, whereas three other variables (low Apgar score, RDS and ibuprofen given to newborns) were identified as lower independent risk factors (Table 5).
Discussion
Based on this work, we would underline the role played by some drugs, therapeutic interventions and diseases in postnatal renal function of neonates with nephrogenesis mostly completed, while this analysis is difficult in the presence of a high-grade prematurity. More importantly, the multivariate analysis underlines the role of NSAIDs taken by mothers during pregnancy or administered to newborns in ARF development, confirming our previous data related to a lower number of preterm newborns [6].
These results derive from an accurate analysis of four groups of preterm newborns with different G.A. in the 1st month of life, taking into account all information obtained by a detailed questionnaire developed in an attempt to understand some aspects not clearly elucidated by other authors. In fact, in the literature relatively few data exist about renal function maturation, particularly in preterm infants and in any case no study examines all the factors potentially affecting kidney function. Some papers report data on renal function in wide G.A. categories [7]; others are confined to the first days of life [8–10] or related to longer periods but at intervals of 2 or more weeks [7, 11, 12]. Only a few studies report data comparable with ours. A study by Aperia et al. [13] showed that preterm infants born before 34 weeks of gestation had significantly lower GFRs than full-term infants and that this difference persisted for up to 3–5 weeks postnatally. Bueva et al. [14] reported creatinine levels in 28 healthy full-term infants and three groups of 38 premature infants from birth until 3 weeks of life: on day 1.5, Crs concentrations were significantly higher in preterm compared to term infants, correlated positively with G.A. and persisted higher during the 2nd week of life. More recently, Gallini et al. [15] measured Crs, creatinine clearance (CrCl) and fractional excretion of sodium (FeNa) until the 5th week of life in 83 preterm neonates under 32 weeks divided into four groups according to G.A. Glomerular function showed a progression directly correlated to G.A. and postnatal age, while tubular function correlated inversely to the same parameters.
From our data, no differences at birth were observed in Crs values among the four groups: this is not surprising, since Crs at birth reflects maternal plasma concentrations and therefore it is not a reliable index of renal function [8, 16]. During the following days, our results are compatible with those of other authors [10, 17] and clearly demonstrate that Crs in preterm infants does not fall steadily from birth, but rises in the first days of life, reaching a peak and then falling to equilibrium levels. This trend of the fall was slower compared to a 72-h period observed by other authors in term neonates [18]. In the neonates with lower G.A. (group A), after the more marked initial increase in Crs concentrations, the decrease was much slower, perhaps reflecting a retarded progression in glomerular function [7] and/or a greater creatinine backflow across the immature tubular structures [17]. Another possible explanation could be the greater amount of drugs given to neonates with a lower G.A. that could have affected, even under normal conditions, renal function.
If we examine separately, within each group, Crs data under both normal and pathological conditions, on the one hand in cases of normal renal function the initial rise in Crs values was evident only in neonates of group A and the physiological decline was more pronounced in neonates of group D, leading to a Crs value at the 28th day of life close to 35.4 μmol/l, which is considered a terminal value after complete adaptation of glomerular function [8]. These data agree well with the fact that in neonates of group D (G.A. 33–36 weeks) nephrogenesis could have been completed [16]. On the other hand, in neonates with impaired renal function, the marked increase in Crs values in all groups is evident, persisting at least until the 10th day and after. This situation of compromised function seems to be a transient condition since Crs values tended toward a progressive decrease after about 14 days of life, persisting at pathological levels only in 8% of neonates of group A, 3% of group B and 2% of group C at the end of the study period.
Our data seem to confirm the prerenal origin of ARF [2] related to drugs, complications or therapeutic interventions that cause hypoperfusion of the kidneys. This agrees well with the higher percentage of hyperechogenicity observed in VLBW of group A: the medullary region is especially sensitive to hypoxaemic damage [19] and these neonates were affected concomitantly by different pathological conditions and received multiple treatments.
In order to quantify all risk factors involved in kidney impairment, first of all we compared carefully the two subpopulations of neonates within the four groups and we found some significant differences. In neonates of group A, the differences were mainly related to the treatment of two pathological conditions, hyperbilirubinaemia and PDA, which affect particularly VLBW infants and seem to predispose to renal problems [2, 20–23]. In neonates of group D, the role played by a greater number of factors, as specified in the “Results” section, is more evident. The univariate analysis of all these factors confirmed a role in renal impairment for maternal NSAIDs [24–28], intubation at birth [2], catheterization [15, 22], mechanical ventilation [6], a low Apgar score at 5 min [6, 29, 30], RDS [31, 32] and ibuprofen given to the newborns [22].
The multivariate analysis, which takes into account the interdependency of different factors in ARF development, demonstrated that only five of these variables are independent predictors of renal impairment: maternal NSAIDs, a low Apgar score at 5 min, intubation at birth, RDS and ibuprofen given to the newborns. This confirmed the important role played by drugs such as NSAIDs and by respiratory problems, all contributing to a decrease in renal perfusion.
In fact, administration of NSAIDs results in decreased renal perfusion and urine output due to their mechanism of action, implying the inhibition of vasodilatory prostaglandins [21]. A clear relationship between renal problems and anoxia has been reported by some authors [6, 29, 30]. Moreover, RDS is considered one of the main causes of prerenal failure by reducing GFR and renal plasma flow [31, 32], particularly if the severity of the disease implies treatments such as mechanical ventilation and surfactant [6]. Finally, the concomitant presence of all these factors in a same subject could amplify the single effects on renal function.
This probably justifies why in preterm newborns of group A (G.A. 22–25 weeks) more than 50% of subjects present a transient alteration of renal function; thus, it is not easy to differentiate the effect on renal function of a high-grade prematurity, concomitant multiple diseases and pharmacological treatments. Instead, in neonates of group D where nephrogenesis is mostly completed (G.A. ≥33 weeks) the percentage of subjects with renal impairment is considerably lower (15%) but among these neonates the role played by some drugs, therapeutic interventions and diseases is evident.
In conclusion, from our data a multifactorial origin of ARF in the newborns seems to be confirmed. In this context, the influence that pharmacological treatment with NSAIDs during pregnancy could have on the foetus or newborn has to be underlined overall. Several cases of severe and sometimes irreversible renal insufficiency have been described in neonates after prenatal exposure to NSAIDs [24–28], so this iatrogenic effect derived from maternal drug consumption should be avoided. Particular attention has to be paid to the bulk of premature newborns who experience a slight increase in Crs by careful monitoring, since the line between normality and renal impairment is very thin in the first days of life and iatrogenic effects due to drug treatments could be avoided [6].
References
Fanos V, Khoory BJ, Cataldi L (1996) Postischaemic acute renal failure in newborns. Physiopathological aspects and early diagnosis. In: Cataldi L, Fanos V, Simeoni U (eds) Neonatal nephrology in progress. Agorà, Lecce, pp 237–249
Toth-Heyn P, Drukker A, Guignard JP (2000) The stressed neonatal kidney: from pathophysiology to clinical management of neonatal vasomotor nephropathy. Pediatr Nephrol 14:227–239
Drukker A, Guignard JP (2002) Renal aspects of the term and preterm infant: a selective update. Curr Opin Pediatr 14:175–182
Fanos V, Cataldi L (1999) Antibacterial-induced nephrotoxicity in the newborn. Drug Saf 20:245–267
Tommiska V, Heinonen K, Ikonen S, Kero P, Pokela ML, Renlund M, Virtanen M, Fellman V (2001) A national short-term follow-up study of extremely low birth weight infants born in Finland in 1996–1997. Pediatrics 107:e2
Cataldi L, Leone R, Moretti U, De Mitri B, Fanos V, Ruggeri L, Sabatino G, Torcasio F, Zanardo V, Attardo G, Riccobene F, Martano C, Benini D, Cuzzolin L (2005) Potential risk factors for the development of acute renal failure in preterm newborn infants: a case-control study. Arch Dis Child Fetal Neonatal Ed 90:514–519
Sonntag J, Prankel B, Waltz S (1996) Serum creatinine concentration, urinary creatinine excretion and creatinine clearance during the first 9 weeks in preterm infants with a birth weight below 1,500 g. Eur J Pediatr 155:815–819
Gordjani N, Burghard R, Leititis JU, Brandis M (1988) Serum creatinine and creatinine clearance in healthy neonates and prematures during the first 10 days of life. Eur J Pediatr 148:143–145
Siegel SR, Oh W (1976) Renal function as a marker of human fetal maturation. Acta Paediatr Scand 65:481–485
Miall LS, Henderson MJ, Turner AJ, Brownlee KG, Brocklebank JT, Newell SJ, Allgar VL (1999) Plasma creatinine rises dramatically in the first 48 hours of life in preterm infants. Pediatrics 104:e76
Brion L, Fleischman A, McCarton C, Schwartz G (1986) A simple estimate of glomerular filtration rate in low birth weight infants during the first year of life: non-invasive assessment of body composition and growth. J Pediatr 109:698–707
Ross B, Cowett R, Oh W (1977) Renal function of low birth weight infants during the first two months of life. Pediatr Res 11:1162–1164
Aperia A, Broberger O, Elinder G, Herin P, Zetterstrom R (1981) Postnatal development of renal function in preterm and full-term infants. Acta Paediatr Scand 70:183–187
Bueva A, Guignard JP (1994) Renal function in preterm neonates. Pediatr Res 36:572–577
Gallini F, Maggio L, Romagnoli C, Marrocco G, Tortorolo G (2000) Progression of renal function in preterm neonates with gestational age < 32 or = weeks. Pediatr Nephrol 15:119–124
Wilkins BH (1992) Renal function in sick very low birth weight infants: 1. Glomerular filtration rate. Arch Dis Child 67:1140–1145
Guignard JP, Drukker A (1999) Why do newborn infants have a high plasma creatinine? Pediatrics 103:e49
Manzar S, Al-Umran K, Al-Awary BH, Al-Faraidy A (2001) Changes in plasma creatinine in the first 72 hours of life. Arch Dis Child 85:F146–F147
Brezis M, Epstein FH (1993) Cellular mechanisms of the acute ischemic injury in the kidney. Annu Rev Med 44:27–37
Dennery PA, Seidman DS, Stevenson DK (2001) Neonatal hyperbilirubinemia. N Engl J Med 344:581–590
Schlondorff D (1993) Renal complications of nonsteroidal drugs. Kidney Int 44:643–653
Ojala R, Ala-Houhala M, Ahonen S, Harmoinen A, Turjanmaa V, Ikonen S, Tammela O (2001) Renal follow-up of premature infants with and without perinatal indomethacin exposure. Arch Dis Child 84:F28–F33
Martin SJ, Danziger LH (1994) Continuous infusion of loop diuretics in the critically ill: a review of the literature. Crit Care Med 22:1323–1329
Peruzzi L, Gianoglio B, Porcellini MG, Coppo R (1999) Neonatal end-stage renal failure associated with maternal ingestion of cyclo-oxygenase-type-1 selective inhibitor nimesulide as tocolytic. Lancet 354:1615
Balasubramaniam J (2000) Nimesulide and neonatal renal failure. Lancet 355:575
Holmes RP, Stone PR (2000) Severe oligohydramnios induced by cyclooxygenase-2 inhibitor nimesulide. Obstet Gynecol 96:810–811
Cuzzolin L, Dal Cerè M, Fanos V (2001) NSAID-induced nephrotoxicity from the fetus to the child. Drug Saf 24:9–18
Benini D, Fanos V, Cuzzolin L, Tatò L (2003) In utero exposure to nonsteroidal anti-inflammatory drugs: neonatal renal failure. Pediatr Nephrol 19:232–234
Karlowicz MG, Adelman RD (1992) Acute renal failure in the neonate. Clin Perinatol 19:139–158
Gouyon JB, Guignard JP (2000) Management of acute renal failure in newborns. Pediatr Nephrol 14:1037–1044
Hentschel R, Lödige B, Bulla M (1996) Renal insufficiency in the neonatal period. Clin Nephrol 46:54–58
Guignard JP, John EG (1986) Renal function in the tiny, premature infant. Clin Perinatol 13:377–399
Acknowledgements
Special thanks to B. De Mitri, L. Ruggeri, G. Sabatino, E. Barbante, F. Torcasio, V. Zanardo, G. Attardo, F. Riccobene, S. Borgione, C. Martano, D. Benini (Neonatal Nephrology Study Group of the Italian Society of Neonatology) so helpful in collecting the data. We also thank U. Moretti (University of Verona) for the statistical support. This study was partly funded by MIUR 60% grants (University of Sacred Heart, Rome). Some of the data were presented in the poster session at the 46th Meeting of the European Society of Pediatric Research, 31 August–3 September, 2005, Siena (Italy).
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Cuzzolin, L., Fanos, V., Pinna, B. et al. Postnatal renal function in preterm newborns: a role of diseases, drugs and therapeutic interventions. Pediatr Nephrol 21, 931–938 (2006). https://doi.org/10.1007/s00467-006-0118-2
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00467-006-0118-2