Abstract
Objective
To identify the prevalence of renal insufficiency (RI) in children with a history of prematurity and acute kidney injury (AKI).
Study design
This prospective cohort study evaluated renal function in children born preterm at 5–9 years of age. Univariable analyses compared perinatal and follow-up data from subjects with and without AKI history, and with and without current RI. Regression analyses were attempted to model RI as a function of AKI and other clinical risk factors.
Results
Fifteen of 43 (35%) participants had previously undiagnosed RI. Only children with no AKI history or neonatal stage 1 AKI presented for follow-up. Children born preterm with a history of stage 1 AKI had higher serum creatinine (sCr) at follow-up, but were not more likely to have RI compared to children without stage 1 AKI history (RI prevalence 30% and 36% in AKI and non-AKI group, respectively).
Conclusion
The high prevalence of RI in this preterm cohort at middle childhood follow-up highlights the need for routine kidney health assessments in this population. Large multicenter studies are needed to further characterize the impact of premature birth and mild AKI on renal function throughout childhood.
Similar content being viewed by others
Introduction
Premature infants are at increased risk for chronic kidney disease (CKD) even in the absence of known nephrotoxic exposures or acute kidney injury (AKI) in the neonatal period [1,2,3,4,5]. Since the majority of nephrogenesis occurs in the third trimester, premature infants have lower nephron mass at birth when compared with term infants [6,7,8], and early arrest of nephrogenesis [8, 9]. Relative oligonephronia and premature arrest of branching nephrogenesis may result in compensatory hyperfiltration of individual nephrons [10]. While this hyperfiltration translates to an increased glomerular filtration rate (GFR) acutely, consequent development of glomerular hypertension and fibrosis ultimately results in further nephron loss and decreased GFR [10,11,12,13,14]. Prospective studies of former preterm, very low- (VLBW) and extremely low- (ELBW) birthweight (BW) infants suggest that signs of aberrant renal development and/or dysfunction, including small kidney volume on imaging, hypertension, lower estimated GFR (eGFR), and microalbuminuria, may be evident in early childhood [15,16,17,18].
AKI in the neonatal period may increase the risk for progression to CKD, particularly in children with a history of prematurity [3, 4, 19, 20]. Comparisons across studies of neonatal AKI progression to childhood CKD are complicated by differing definitions of AKI, differing equations for determination of eGFR and variable eGFR thresholds for defining CKD and/or renal dysfunction [3, 4, 19,20,21]. Despite apparent complete recovery, children born prematurely with neonatal AKI of any severity constitute a particularly high-risk population, due to a lack of standardized algorithms for surveillance of renal health following NICU hospitalization, either with the general pediatrician or a nephrologist.
We previously reported the incidence of AKI in preterm infants <30 weeks gestation in our NICU at 30% [22], which is in the reported range of similar studies of AKI in preterm, ELBW, and/or VLBW infants [23,24,25,26,27,28]. The majority of our patients had the mildest form of AKI (Stage 1 by the modified Acute Kidney Injury Network (AKIN) criteria) [23] and had a normal serum creatinine (sCr) documented prior to hospital discharge [22]. We now report on a subgroup of that initial cohort who presented for renal health assessments at 5–9 years of age. We hypothesized that prior history of AKI, including mild AKI, is an independent risk factor for evolving CKD manifesting as one or more signs of renal insufficiency (RI) in childhood.
Materials/subjects and methods
Subjects
This study was approved by the Program for the Protection of Human Subjects at The Icahn School of Medicine at Mount Sinai. The electronic medical record (EMR) was used to identify all preterm infants born at The Mount Sinai Hospital at <30 weeks gestation from 2007 to 2013. sCr values from the birth hospitalization were reviewed through the EMR to identify former preterm infants with and without a history of neonatal AKI. AKI was defined by sCr values using the modified AKIN staging criteria described by Koralkar et al. [23]. Urine output criteria were not used as this retrospective determination of AKI precluded our ability to employ quality control measures for accurate urine output assessment and recording. Subjects with major congenital malformations, including congenital anomalies of the kidneys or urinary tract but not isolated hydronephrosis, were excluded. Subjects were also excluded in the setting of maternal renal failure, death before discharge, or lack of documented creatinine (Cr) measurements.
Power calculation
Based on our previous retrospective analysis of neonatal AKI in our NICU population, we anticipated the prevalence of prior AKI exposure to be 30% [22]. Therefore, in our power calculation, we chose to have a ratio of 1:2 of patients with a history of any stage of neonatal AKI to those with no history of neonatal AKI. Based on the reported prevalence of renal dysfunction following preterm birth at a median age of 5 years in a similar VLBW cohort (65% with neonatal AKI, 14% without AKI) [3], we estimated that a study sample of 12 patients with a history of neonatal AKI and 24 patients with no history of neonatal AKI (total sample size 36) was needed to reject the null hypothesis that the prevalence of RI in the groups is equal with power of 0.8 and a type 1 error probability of 0.05. To compensate for any error in the estimate of AKI prevalence in our population, we recruited an additional 20% for a total sample size of 43 participants.
Study visit
Parents of potential subjects were first approached by mail. Those who expressed interest in study participation were then contacted by phone to schedule a single study visit at the Clinical Research Unit at the Icahn School of Medicine at Mount Sinai. Informed consent was obtained by a member of the study team at the time of the study visit. In addition, assent was obtained from all children ages 7 and above. At the study visit, height, weight, and manual blood pressure were measured. Serum was collected for blood urea nitrogen (BUN), Cr, cystatin C, and neutrophil gelatinase-associated lipocalin (NGAL). Urine specimen cups mailed in advance of the study visit enabled collection of first morning urine samples, which were then analyzed for protein, Cr, beta-2-microglobulin (B2M), and NGAL. Serum BUN, Cr, and cystatin C, and urine Cr, protein, and B2M levels were measured by the Mount Sinai Clinical Laboratories. sCr was determined using the enzymatic method. Cystatin C was determined by immunonephelometric assay. Serum and urine NGAL were measured in the Mount Sinai Human Immune Monitoring Core Facility using the Quantikine Human Lipocalin-2 Immunoassay (R&D Systems, Inc, Minneapolis, MN).
Data analysis
eGFR was calculated using both the full Chronic Kidney Disease in Children (CKiDfull) [29] and the bedside Schwartz (CKiDbed) [30] equations as follows: CKiDfull = 39.8 × (height[m]/sCr [mg/dL]0.456 × (1.8/cystatin C [mg/L])0.418 × (30/BUN [mg/dL])0.079 × 1.076 (if male) × (height [m]/1.4)0.179 CKiDbed = 41.3 × (height [m]/sCr [mg/dL] RI was defined by eGFR < 90 mL/min/1.73 m2 (by either calculation) and/or urine protein:creatinine ratio (UPC) > 0.2 mg/mg and/or systolic blood pressure (SBP) or diastolic blood pressure ≥95th percentile (for age, sex and height) [31]. Children with eGFR 90–99 mL/min/1.73 m2 and/or UPC = 0.2 mg/mg were considered at risk for RI. The trigger for nephrology consultation was “any RI,” or the primary composite outcome of children with current RI and those at risk for RI, as even borderline RI in this population was considered to be clinically significant and potentially a manifestion of evolving CKD. Retrospective perinatal data and current clinical study data from subjects with and without history of neonatal AKI, and with and without any RI were compared using Fisher’s exact or independent t-tests as appropriate. All variables with significant univariate analysis were included in general linear models of AKI status and RI status, respectively. All data were analyzed using SAS Studio 3.8 (Cary, NC) [32] and RStudio Version 1.1.463 (Boston, MA) [33].
Results
Forty-three children (13 with a history of stage 1 AKI and 30 with no history of neonatal AKI) from the original study cohort [22] participated in the current study. Despite recruitment efforts being inclusive of all stages of AKI, there were no children with stage 2 or 3 neonatal AKI history who responded for follow-up. The median age of participants was 8 years (IQR 6–9) at the time of the study visit. Fifteen of 43 (35%) participants presented with previously undiagnosed RI, including 4 of 13 (30%) children with a history of stage 1 AKI, and 11 of 30 (36%) children without neonatal AKI history. Ten of these children (23%) met criteria for current RI and were referred for immediate nephrology evaluation; the other five children were at risk for RI and were referred for nephrology evaluation in 1 year. Of the ten children who were referred for immediate nephrology follow-up, three (30%) had a history of stage 1 AKI. Of the 5 children at risk for RI, one (20%) had a history of stage 1 AKI.
There were five children born to mothers with hypertensive disease during pregnancy who presented for follow-up. While none of these children had AKI during their NICU stay, three (60%) had signs of current RI. Of those, one child had elevated BP at follow-up in addition to low eGFR.
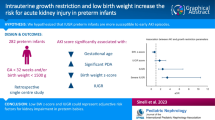
Table 1 presents univariable analyses of maternal/perinatal, neonatal, and clinical factors at the study visit in children with and without stage 1 AKI during the NICU hospitalization. Children with a history of stage 1 AKI were significantly more likely to have a mother with chorioamnionitis at the time of their birth, to be born at a younger gestational age (GA), to have a lower BW, and to have a higher Clinical Risk Index for Babies II score [34] than children without neonatal AKI. Children with a history of neonatal stage 1 AKI were also more likely to have received indomethacin for treatment of a patent ductus arteriosus. While the peak sCr during the NICU hospitalization was higher in children with a history of stage 1 AKI, the first measured sCr was actually lower in these children. At the follow-up visit, children with a history of stage 1 AKI had significantly higher sCr and higher serum NGAL (sNGAL). Approximately one-third of children with stage 1 AKI history had signs of RI at follow-up, but this was not significantly different from the prevalence of RI observed in children without neonatal AKI. Using linear regression modeling that included all factors significant in univariable analyses (maternal chorioamnionitis; GA; neonatal administration of indomethacin; first and peak neonatal sCr; sCr and sNGAL at follow-up), only initial neonatal sCr, peak neonatal sCr, and current sCr remained significantly associated with stage 1 AKI history in the multivariable model (Fig. 1).
Table 2 presents univariable analyses of maternal/perinatal, neonatal, and clinical factors at the study visit in children with and without any RI. The maternal sCr immediately prior to delivery was significantly higher in children with any RI. There were no differences in GA or BW between the two groups of children. Children with any signs of RI at follow-up were more likely to be female and small for gestational age (SGA) at birth, and less likely to have received ampicillin during their NICU hospitalization than children with normal renal function at follow-up. Urinary NGAL (uNGAL) at the time of the study visit was significantly higher in children with any RI. A multivariable model for RI was attempted but did not converge due to the limited sample size.
Figure 2 shows the full range of eGFRs at follow-up calculated using the CKiDbed and CKiDfull equations. In Fig. 3, eGFR values derived from each equation are compared between children with and without neonatal stage I AKI history. The eGFR calculated using CKiDbed was significantly higher than the eGFR calculated using CKiDfull for children with (CKiDbed 114 vs. CKiDfull 103, p < 0.05) and without (CKiDbed 125 vs. CKiDfull 104, p < 0.000) neonatal AKI history.
In addition to urine and sNGAL, other biomarkers measured at the study visit included serum cystatin C and urinary B2M. Mean cystatin C was 0.73 ± 0.08, with no significant difference between children with and without any RI. Mean urinary B2M in all children at follow-up was 124.8 ± 103 μg/L, with no significant difference between children with and without signs of RI.
Discussion
In this small single-center cohort study, approximately one-third of children born at <30 weeks gestation with a history of stage 1 neonatal AKI had signs of RI at age 5–9 years. However, this was not higher than the observed prevalence of any RI in children born preterm with no AKI history. This contrasts with the findings of a recent study by Harer et al. in which neonatal AKI history carried a 4.5-fold risk of renal dysfunction at follow-up when compared with preterm birth without AKI [3]. While they also evaluated a VLBW cohort, the children were significantly younger at the time of follow-up evaluation and the majority of the AKI group had more severe stage 2 or 3 neonatal AKI history. In another prospective study of former ELBW infants with and without neonatal AKI, AKI was not associated with higher risk of CKD in childhood; however, the sole criteria for defining CKD in this study was eGFR < 90 mL/min/1.73 m2 and the eGFR calculation used is not clear [26]. Methodological differences and representation of more severe AKI in these studies unfortunately preclude meaningful comparison with our results. In our study, 15 children (35%) had signs of RI concerning for evolving CKD. These findings are consistent with other follow-up studies of preterm and LBW cohorts that report CKD prevalence at 23–45% [3,4,5, 19]. Both SGA and female sex have previously been identified as risk factors for CKD [2, 16, 33]. While SGA has been examined as an independent risk factor for CKD in the preterm population [2, 16], the risk of CKD progression associated with female sex has not been described in survivors of prematurity. In another high-risk pediatric population (heart transplant recipients), however, females were significantly more likely to have CKD at a mean age of 9.9 years at follow-up [35]. It should be noted that the CKiDfull equation utilizes a correction factor for male sex resulting in a higher eGFR than would be determined for a female with otherwise equal height and laboratory values; this may explain the sex differences noted between groups with and without RI in our study. Further studies are needed to determine if female sex independently increases the risk for progression to CKD in children with a history of preterm birth.
Early identification of CKD is necessary to inform dosing for renally cleared medications; enhance screening and early intervention for comorbid cardiovascular disease, anemia, renal osteodystrophy, neurocognitive deficits, and growth impairment; and increase attention to other modifiable risk factors including obesity, hypertension, hyperlipidemia, and diabetes. This requires vigilant screening of high-risk populations, guidelines for preferred testing and frequency of kidney health evaluations, and clearly defined thresholds for subspecialty referral. The 2012 Kidney Disease Improving Global Outcomes (KDIGO) Work Group defines CKD as either eGFR < 60 ml/min/1.73 m2 for >3 months or eGFR ≥ 60 ml/min/1.73 m2, with additional signs of renal dysfunction (albuminuria, imaging or histologic abnormalities, urinary sediment or other evidence of tubular dysfunction) [36]. The guidelines also suggest staging CKD by cause, degree of albuminuria and GFR—relevant to this discussion is the classification of GFR ≥ 90 ml/min/1.73 m2 as normal and GFR 60–89 ml/min/1.73 m2 as mildly decreased, or stage 2 CKD when in the setting of other renal dysfunction. Both the longitudinal CKiD study and several smaller prospective analyses of children at risk for CKD utilize the cutoff of 90 ml/min/1.73 m2 in definitions of CKD and/or RI [3,4,5, 26, 35, 37, 38]. In this study, we utilized the threshold of 90 ml/min/1.73 m2 rather than 60 ml/min/1.73 m2 because our goal was not to diagnose and stage CKD, but to identify any signs of RI ideally well before kidney function has declined to the levels consistent with the KDIGO definition of CKD. While GFR ≥ 90 ml/min/1.73 m2 is technically classified as normal, the higher baseline risk of our population prompted the decision to recommend children with borderline values (90–99 ml/min/1.73 m2) for repeat kidney health evaluation with nephrology in 1 year, to ensure follow-up for study subjects with “normal” but potentially declining renal function that could not be determined within this cross-sectional analysis. Further complicating characterization of CKD progression in children is the challenge of measuring GFR. While renal inulin clearance is still the gold standard for measured GFR, it is technically challenging in children and moderately invasive, requiring an IV infusion and often a urinary catheter. More ideal for routine screening of high-risk populations is the use of eGFR, for which multiple estimating equations have been developed and studied in children. While many eGFR equations have shown significant correlation with measured GFR in large studies of children with CKD [29, 30], few have been validated in children with normal renal function [39,40,41,42]. In our study, the multivariate CKiDfull equation incorporating both sCr and cystatin C identified 11 children (26% of the study population) with decreased eGFR, whereas the CKiDbed only identified 2 children (5% of the study population) with decreased eGFR. Pediatric populations with increased risk for CKD (ie. history of preterm birth, SGA, LBW, and AKI history) should be screened for RI using multiple measures of renal function, as it remains unclear which eGFR equation is most reliable in this setting. An eGFR <90 ml/min/1.73 m2 in known high-risk populations should prompt further workup, consideration for nephrology referral and measures to mitigate risk for progression to CKD whenever possible.
Comprehensive longitudinal screening of high-risk children should assess for other signs of renal dysfunction, including hypertension and proteinuria. Hypertension has been independently associated with CKD progression in children with both glomerular and non-glomerular disease [43, 44]. In studies of children born preterm, rates of hypertension vary widely depending on definitions used and age at follow-up [3, 4, 15, 18]. Early recognition of hypertension is important not only for identifying children with RI and predicting CKD progression, but also because it represents a potentially modifiable risk factor for comorbid cardiovascular disease [45]. In our study, none of the children presented with isolated hypertension. Proteinuria, albuminuria, and/or hypoalbuminemia are also important indices of renal function. Elevated UPC ratio and hypoalbuminemia are both associated with a significant decrease in time to need for renal replacement therapy or 50% reduction in GFR in children with both glomerular and non-glomerular disease [41]. Baseline proteinuria is independently associated with CKD progression in children with non-glomerular CKD [44]. In our cohort, all children referred to nephrology for proteinuria presented with elevated UPC as their sole index of renal dysfunction, which underscores the importance of urine screening in high-risk populations during childhood.
We previously reported on the lower incidence of AKI in neonates born to mothers with pre-eclampsia and/or mothers who received intrapartum magnesium [22]. In our small cohort, several children born to mothers with hypertensive disease of pregnancy presented with evidence of RI at follow-up. Despite the seemingly protective effects against neonatal AKI acutely, it is unclear whether that translates to better long-term renal outcomes.
In our study, we assessed markers of tubular function including urinary B2M, and urine and sNGAL. Urinary B2M excretion was similar in children with and without any current RI. While a reference range for serum B2M exists for healthy children, there are no normative values for urinary B2M to enable comparison of our data with low-risk children with normal renal function [46]. Median sNGAL at follow-up for all children in our study was similar to that of healthy children [47]. Despite evidence of acute sNGAL elevations following AKI [48], it has not been previously evaluated as a biomarker for remote AKI history. In our study population, while sNGAL was significantly higher in the AKI group in univariable analysis, there was no significant relationship between neonatal AKI and current sNGAL in multivariable analysis. Furthermore, all sNGAL values in children with AKI history fell within normal reference ranges and therefore, clinical significance of any difference between groups remains unclear. Bennet et al. described a significant difference in uNGAL excretion between healthy males and females across all age groups, with median uNGAL excretion in the 5–9 age group 2.6× higher in females [49]. In our subjects, uNGAL at follow-up was significantly higher in children with RI in univariable analysis—this may be due to the female predominance of the RI group.
Our study is limited by a small sample size and single-center study population. Furthermore, we only enrolled children with stage 1 AKI history and thus may be inadequately powered to detect a true difference in RI between AKI and non-AKI groups. Although we targeted children with a history of any stage AKI, we were only contacted by participants with a history of no AKI or stage 1 disease. It may be that children with a history of more severe neonatal AKI had already been evaluated for kidney disease based on history, and therefore did not respond to study outreach. Alternatively, children with a history of more severe neonatal AKI may have more significant generalized morbidity related to prematurity and thus a lower response rate. In fact, in-hospital mortality of our original cohort with stage 2–3 AKI was 41%. As our power calculation was based on a study with a more heterogenous AKI group predominantly comprised of subjects with history of more severe stage 2–3 injury [3], our study may be underpowered to detect an association between stage 1 AKI and CKD in childhood. As long-term follow-up studies of kidney function in children born preterm are scarce, it is difficult to determine what sample size is necessary to enable characterization of the independent effect of mild neonatal AKI on renal function of former preterm infants in early childhood, if any exists. Another limitation is the lack of gold standard GFR measurements for validation of eGFRs calculated by either the bedside or CKiDfull equations, as well as the lack of a control group of age-matched healthy term children. Last, only a single BP measurement was obtained, whereas ambulatory blood pressure monitoring may be more appropriate for this high-risk population [45].
Conclusion
This study of children born before 30 weeks gestation identified a high prevalence of RI at a median of 8 years of age. While one-third of children with neonatal stage 1 AKI history had signs of RI at follow-up, this was not significantly different from children with no AKI history. Larger prospective studies are needed to investigate the impact of mild neonatal AKI on long-term renal outcomes in the ex-preterm population, determine the optimal timing and frequency of screening for CKD, and define thresholds for nephrology referral and/or intervention. Screening of high-risk populations should incorporate multiple markers of renal function including blood pressure, urine protein excretion, and eGFR. Further studies are needed to establish normal pediatric reference ranges for urinary biomarkers and their role in identifying children with RI.
References
Crump C, Sundquist J, Winkleby MA, Sundquist K. Preterm birth and risk of chronic kidney disease from childhood into mid-adulthood: national cohort study. BMJ. 2019;365:l1346.
Gjerde A, Lillås BS, Marti H-P, Reisæter AV, Vikse BE. Intrauterine growth restriction, preterm birth and risk of end-stage renal disease during the first 50 years of life. Nephrol Dial Transpl. 2020;35:1157–63.
Harer MW, Pope CF, Conaway MR, Charlton JR. Follow-up of acute kidney injury in neonates during childhood years (FANCY): a prospective cohort study. Pediatr Nephrol. 2017;32:1067–76.
Bruel A, Rozé J-C, Quere M-P, Flamant C, Boivin M, Roussey-Kesler G, et al. Renal outcome in children born preterm with neonatal acute renal failure: IRENEO-a prospective controlled study. Pediatr Nephrol. 2016;31:2365–73.
Nishizaki N, Hirano D, Nishizaki Y, Fujinaga S, Nagata S, Ohtomo Y, et al. Increased urinary angiotensinogen is an effective marker of chronic renal impairment in very low birth weight children. Clin Exp Nephrol. 2014;18:642–8.
Abitbol CL, Rodriguez MM. The long-term renal and cardiovascular consequences of prematurity. Nat Rev Nephrol. 2012;8:265–74.
Faa G, Gerosa C, Fanni D, Nemolato S, Locci A, Cabras T, et al. Marked interindividual variability in renal maturation of preterm infants: lessons from autopsy. J Matern Fetal Neonatal Med. 2010;23:129–33.
Bonsib SM. Renal hypoplasia, from grossly insufficient to not quite enough: consideration for expanded concepts based upon the author’s perspective with historical review. Adv Anat Pathol. 2020;27:311–30.
Rodríguez MM, Gómez AH, Abitbol CL, Chandar JJ, Duara S, Zilleruelo GE. Histomorphometric analysis of postnatal glomerulogenesis in extremely preterm infants. Pediatr Dev Pathol. 2004;7:17–25.
Brenner BM, Lawler EV, Mackenzie HS. The hyperfiltration theory: a paradigm shift in nephrology. Kidney Int. 1996;49:1774–7.
Mañalich R, Reyes L, Herrera M, Melendi C, Fundora I. Relationship between weight at birth and the number and size of renal glomeruli in humans: a histomorphometric study. Kidney Int. 2000;58:770–3.
Koike K, Ikezumi Y, Tsuboi N, Kanzaki G, Haruhara K, Okabayashi Y, et al. Glomerular density and volume in renal biopsy specimens of children with proteinuria relative to preterm birth and gestational age. CJASN. 2017;12:585–90.
Hodgin JB, Rasoulpour M, Markowitz GS, D’Agati VD. Very low birth weight is a risk factor for secondary focal segmental glomerulosclerosis. CJASN. 2009;4:71–6.
Carmody JB, Charlton JR. Short-term gestation, long-term risk: prematurity and chronic kidney disease. Pediatrics. 2013;131:1168–79.
Vashishta N, Surapaneni V, Chawla S, Kapur G, Natarajan G. Association among prematurity (<30 weeks’ gestational age), blood pressure, urinary albumin, calcium, and phosphate in early childhood. Pediatr Nephrol. 2017;32:1243–50.
Vollsæter M, Halvorsen T, Markestad T, Øymar K, Ueland PM, Meyer K, et al. Renal function and blood pressure in 11 year old children born extremely preterm or small for gestational age. PloS ONE. 2018;13:e0205558.
Rakow A, Laestadius Å, Liliemark U, Backheden M, Legnevall L, Kaiser S, et al. Kidney volume, kidney function, and ambulatory blood pressure in children born extremely preterm with and without nephrocalcinosis. Pediatr Nephrol. 2019;34:1765–76.
Sanderson KR, Chang E, Bjornstad E, Hogan SL, Hu Y, Askenazi D, et al. Albuminuria, hypertension, and reduced kidney volumes in adolescents born extremely premature. Front Pediatr. 2020;8:230.
Abitbol CL, Bauer CR, Montané B, Chandar J, Duara S, Zilleruelo G. Long-term follow-up of extremely low birth weight infants with neonatal renal failure. Pediatr Nephrol. 2003;18:887–93.
Chaturvedi S, Ng KH, Mammen C. The path to chronic kidney disease following acute kidney injury: a neonatal perspective. Pediatr Nephrol. 2017;32:227–41.
Mammen C, Al Abbas A, Skippen P, Nadel H, Levine D, Collet JP, et al. Long-term risk of CKD in children surviving episodes of acute kidney injury in the intensive care unit: a prospective cohort study. Am J Kidney Dis. 2012;59:523–30.
Weintraub AS, Connors J, Carey A, Blanco V, Green RS. The spectrum of onset of acute kidney injury in premature infants less than 30 weeks gestation. J Perinatol. 2016;36:474–80.
Koralkar R, Ambalavanan N, Levitan EB, McGwin G, Goldstein S, Askenazi D. Acute kidney injury reduces survival in very low birth weight infants. Pediatr Res. 2011;69:354–8.
Viswanathan S, Manyam B, Azhibekov T, Mhanna MJ. Risk factors associated with acute kidney injury in extremely low birth weight (ELBW) infants. Pediatr Nephrol. 2012;27:303–11.
Jetton JG, Boohaker LJ, Sethi SK, Wazir S, Rohatgi S, Soranno DE, et al. Incidence and outcomes of neonatal acute kidney injury (AWAKEN): a multicentre, multinational, observational cohort study. Lancet Child Adolesc Health. 2017;1:184–94.
Maqsood S, Fung N, Chowdhary V, Raina R, Mhanna MJ. Outcome of extremely low birth weight infants with a history of neonatal acute kidney injury. Pediatr Nephrol. 2017;32:1035–43.
Lee CC, Chan OW, Lai MY, Hsu KH, Wu TW, Lim WH, et al. Incidence and outcomes of acute kidney injury in extremely-low-birth-weight infants. PLoS ONE. 2017;12:e0187764.
Shalaby MA, Sawan ZA, Nawawi E, Alsaedi S, Al-Wassia H, Kari JA. Incidence, risk factors, and outcome of neonatal acute kidney injury: a prospective cohort study. Pediatr Nephrol. 2018;33:1617–24.
Schwartz GJ, Schneider MF, Maier PS, Moxey-Mims M, Dharnidharka VR, Warady BA, et al. Improved equations estimating GFR in children with chronic kidney disease using an immunonephelometric determination of cystatin C. Kidney Int. 2012;82:445–53.
Schwartz GJ, Work DF. Measurement and estimation of GFR in children and adolescents. CJASN. 2009;4:1832–43.
Flynn JT, Kaelber DC, Baker-Smith CM, Blowey D, Carrol AE, Daniels SR, et al. Clinical practice guideline for screening and management of high blood pressure in children and adolescents. Pediatrics. 2017;140:e20171904.
SAS Institute Inc. SAS® Studio 3.8: user’s guide [software]. Cary, NC: SAS Institute Inc.; 2018. Copyright©
RStudio Team. RStudio: integrated development for R [software], Version 1.1.463. Boston, MA: RStudio, Inc; 2020. http://www.rstudio.com/.
Parry G, Tucker J, Tarnow-Mordi W. CRIB II: an update of the clinical risk index for babies score. Lancet. 2003;361:1789–91.
Abraham BP, Frazier EA, Morrow WR, Blaszak RT, Devarajan P, Mitsnefes M, et al. Cystatin C and neutrophil gelatinase-associated lipocalin as markers of renal function in pediatric heart transplant recipients. Pediatr Transpl. 2011;15:564–9.
Kidney Disease: Improving Global Outcomes (KDIGO) CKD Work Group. KDIGO 2012 clinical practice guideline for the evaluation and management of chronic kidney disease. Kidney Int Suppl. 2013;3:1–150.
Mitsnefes MM, Kathman TS, Mishra J, Kartal J, Khoury PR, Nickolas TL, et al. Serum neutrophil gelatinase-associated lipocalin as a marker of renal function in children with chronic kidney disease. Pediatr Nephrol. 2007;22:101–8.
Wong CJ, Moxey-Mims M, Jerry-Fluker J, Warady BA, Furth SL. CKiD (CKD in Children) Prospective Cohort Study: a review of current findings. Am J Kidney Dis. 2012;60:1002–11.
Zachwieja K, Korohoda P, Kwinta-Rybicka J, Miklaszewska M, Moczulska A, Bugasjka J. et al. Modification of the Schwartz equations for children increases their accuracy at eGFR > 60 mL/min/1.73. Ren Fail. 2016;38:787–98.
Fadrowski JJ, Neu AM, Schwartz GJ, Furth SL. Pediatric GFR estimating equations applied to adolescents in the general population. CJASN. 2011;6:1427–35.
Staples A, LeBlond R, Watkins S, Wong C, Brandt J. Validation of the revised Schwartz estimating equation in a predominantly non-CKD population. Pediatr Nephrol. 2010;25:2321–6.
Bacchetta J, Cochat P, Rognant N, Ranchin B, Hadj-Aissa A, Dubourg L. Which Creatinine and Cystatin C equations can be reliably used in children? CJASN. 2011;6:552–60.
Warady BA, Abraham AG, Schwartz GJ, Wong CS, Muñoz A, Betoko A, et al. Predictors of rapid progression of glomerular and non-glomerular kidney disease in children: the CKiD Cohort. Am J Kidney Dis. 2015;65:878–88.
Fathallah-Shaykh SA, Flynn JT, Pierce CB, Abraham AG, Blydt-Hansen TD, Massengill SF, et al. Progression of pediatric CKD of nonglomerular origin in the CKiD Cohort. CJASN. 2015;10:571–7.
Mitsnefes M, Flynn J, Cohn S, Samuels J, Blydt-Hansen T, Saland J, et al. Masked hypertension associates with left ventricular hypertrophy in children with CKD. JASN. 2010;21:137–44.
Kelly J, Raizman JE, Bevilacqua V, Chan MK, Chen Y, Quinn F, et al. Complex reference value distributions and partitioned reference intervals across the pediatric age range for 14 specialized biochemical markers in the CALIPER cohort of healthy community children and adolescents. Clin Chim Acta. 2015;450:196–202.
Wheeler DS, Devarajan P, Ma Q, Harmon K, Monaco M, Cvijanovich N, et al. Serum neutrophil gelatinase-associated lipocalin (NGAL) as a marker of acute kidney injury in critically Ill children with septic shock. Crit Care Med. 2008;36:1297–303.
Mishra J, Dent C, Tarabishi R, Mitsnefes MM, Ma Q, Kelly C, et al. Neutrophil gelatinase-associated lipocalin (NGAL) as a biomarker for acute renal injury after cardiac surgery. Lancet. 2005;365:1231–8.
Bennett MR, Nehus E, Haffner C, Ma Q, Devarajan P. Pediatric reference ranges for acute kidney injury biomarkers. Pediatr Nephrol. 2015;30:677–85.
Acknowledgements
The authors would like to acknowledge The Mount Sinai Clinical Research Unit for their assistance with all aspects of the study visits and specimen processing, and The Mount Sinai Human Immune Monitoring Core Facility for their performance of the NGAL assays.
Funding
This work was supported by a grant from The Icahn School of Medicine at Mount Sinai Pediatric Scholars Program.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Pulju, M., Pruitt, C., Reid-Adam, J. et al. Renal insufficiency in children born preterm: examining the role of neonatal acute kidney injury. J Perinatol 41, 1432–1440 (2021). https://doi.org/10.1038/s41372-021-01097-4
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41372-021-01097-4
- Springer Nature America, Inc.