Abstract
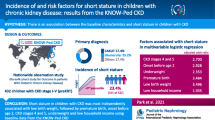
End-stage renal disease (ESRD) causes growth retardation in children, and poor growth has been linked to worse outcomes. Recombinant human growth hormone (rhGH) can increase growth velocity and final adult height in pediatric ESRD patients. We aimed to identify clinical predictors of short stature (height standard deviation score (Ht SDS) <−1.88) and rhGH use in short stature pediatric hemodialysis patients. In 2002, the Centers for Medicare & Medicaid Services (CMS) Clinical Performances Measures (CPM) ESRD Project collected demographic, clinical and laboratory data as well as rhGH use on all in-center hemodialysis patients in the US aged <18 years. The odds ratios (OR) of short stature and rhGH use for individual predictors were determined by multivariate logistic regression modeling. Six-hundred and fifty-one (92%) of 710 eligible patients were included for analysis. Of these, 266 (41%) had Ht SDS <−1.88. After adjustment, short stature was predicted by congenital / urologic causes of ESRD ((OR 5.4; 95% confidence interval [CI], 2.1–13.8; p <0.001) in patients aged 10–14 years; (OR 2.8; 95% CI, 1.5–5.4; p <0.01) in patients aged 15–18 years) and increasing years on dialysis ((OR 1.2; 95% CI, 1.1–1.4; p <0.01) in patients aged 10–14 years; (OR 1.2; 95% CI, 1.1–1.4; p <0.001) in patients aged 15–18 years). Of 266 short stature patients, 214 (80.5%) had data on rhGH use. Of these, 80 (37%) had been prescribed rhGH. After adjustment, use of rhGH in short-stature patients was predicted by white race (OR 2.1; 95% CI, 1.1–4.0; p <0.05), increasing years on dialysis (OR 1.13; 95% CI, 1.05–1.22; p <0.01) and patients with BMI <16.6 kg/m2 (OR 3.1; 95% CI, 1.2–8.4; p <0.05). Increasing age and level of intact parathyroid hormone were not associated with rhGH use among short stature patients. A significant proportion of pediatric hemodialysis patients have short stature. The majority of short-stature patients are not receiving rhGH. Patients with short stature who are white, have longer durations on dialysis and have lower BMI are more likely to receive rhGH.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Children with end-stage renal disease (ESRD) and chronic renal insufficiency often have growth retardation. The etiology of growth retardation in children with ESRD is multifactorial, with the age of onset of chronic kidney disease (CKD), the degree of acidosis, presence of anemia, renal osteodystrophy, poor caloric intake and interference with the growth hormone axis being some of the factors. Poor growth and short stature in children maintained on dialysis has been associated with an increased risk of death and increased rates of hospitalization [1]. Administration of recombinant human growth hormone (rhGH) to pediatric ESRD patients may increase growth velocity and height standard deviation scores (Ht SDS) in pediatric patients [2], and can increase their final adult height [3]. Potential increases in growth velocity from rhGH are most marked in earlier ages and early in the course of chronic kidney disease [4]. The improvement in mean growth velocity from rhGH decreases in magnitude as children age and become more skeletally mature, but still exceeds the baseline untreated growth velocity [5].
Despite the potential to attain normal adult height, many pediatric ESRD patients do not receive rhGH. Only 13% of pediatric hemodialysis (HD) patients in the North American Pediatric Renal Transplant Cooperative Study (NAPRTCS) registry in 2001 were receiving rhGH [6]. In 1999, 33.3% of pediatric ESRD patients with Ht SDS less than −1.88 were receiving rhGH 12 months after initiating dialysis [7]. Factors associated with use of rhGH in pediatric hemodialysis patients have not been extensively described. Pediatric ESRD patients in Texas, USA, were found to be more likely to receive rhGH if they were dialyzed in a pediatric facility than in an adult facility [8]. Reports of increased parathyroid hormone levels [9] and adverse musculoskeletal effects of rhGH, such as slipped capital femoral epiphysis and avascular necrosis of the femoral head [10,11], may make practitioners less likely to prescribe rhGH. The influence of other clinical and demographic factors relating to rhGH use in pediatric HD patients has not been determined. In this study, we aim to identify clinical and demographic characteristics associated with short stature, in addition to other factors associated with prescription of rhGH to pediatric hemodialysis patients with short stature.
Methods
The Centers for Medicare & Medicaid Services (CMS) ESRD Clinical Performance Measures (CPM) Project has collected data on US pediatric in-center hemodialysis patients aged 12 years up to but not including 18 years old since 2000. In 2002, the data collection effort was expanded to include all pediatric HD patients younger than 18 years of age. Also in 2002, additional information on the use of rhGH was collected via a supplemental questionnaire.
Within the 18 ESRD Networks (regional organizations contracted by CMS to perform quality oversight activities to assure the appropriateness of services and protection for dialysis patients), all in-center HD patients younger than 18 years old who were alive on December 31, 2001, were identified. In May of 2002, a 3-page data collection form and a supplemental questionnaire were sent to each facility that had at least one patient with age younger than 18 years. Demographic and clinical information were abstracted for each patient who received in-center HD between October and December 2001.
Demographic information collected included age at time of data collection, gender, race, ethnicity, age, years on dialysis and primary cause of ESRD. Clinical information collected included height, pre- and post-dialysis weight, pre- and post-dialysis blood urea nitrogen (BUN), dialysis session duration, reported single-pool Kt/V (spKt/V), hemoglobin values, serum albumin and the method used to measure the serum albumin (bromcresol purple (BCP) method or bromcresol green (BCG) method). The supplemental questionnaire collected information on whether rhGH had ever been prescribed, intact parathyroid hormone (iPTH) values and units, first monthly serum total calcium and serum phosphate and the specialty of nephrologist (pediatrician vs internist) supervising care of the patient. Completed forms were returned to the appropriate Network office where data were reviewed and entered into a computerized database (Visual FoxPro). The data were aggregated by The Renal Network, and forwarded to CMS for analysis. A subset of questionnaires was validated by Network staff. Outlying data values were also identified and verified with the submitting dialysis center.
For this report, a patient had to meet the following criteria to remain in the sample for analysis: a data collection form with at least one monthly hemoglobin value, at least one paired pre- and post-dialysis BUN value, and at least one serum albumin value over the 3-month study period. This case definition was identical to the one that has been used for the adult (≥18 years old) in-center HD sample over the course of the project period (1993–2002). For this study, additional inclusion criteria included age, sex and at least one reported height. Due to the small numbers of people ( n =78) in racial categories other than black and white, analyses by race were limited to these two racial groups. In analyses by age-stratified groups, the number of children younger than 10 years of age was too small ( n =90) to allow statistical analysis, although they were retained for analyses of the whole study population.
All available reported monthly values were utilized in calculating mean values. SpKt/V values were calculated according to the Daugirdas II formula [12]. Although reported spKt/V values were collected, spKt/V values calculated from the data collected were used for analysis. Normalized protein catabolic rate (nPCR) was calculated for each patient [13]. Body mass index (BMI, kg/m2) was calculated from reported height and mean post-dialysis weight. For analyses, BMI was stratified into quartiles (<16.6, 16.6–18.6, 18.7–21.7, and >21.7 kg/m2). Standardized height scores (Ht SDS) were calculated using the appropriate gender and age-specific mean, standard deviation and adjustment parameters for the national population derived from NHANES III study (2000) of the National Center of Health Statistics. For the purpose of the study, patients were categorized by height SDS <−1.88 vs ≥ −1.88, as the 3rd percentile for age and gender corresponds to height SDS −1.88. Patients with Ht SDS <−1.88 are hereafter referred to as having short stature.
Since the method used to measure serum albumin varied by center, mean serum albumin was stratified by level <3.5 g/dl by the BCG method and <3.2 g/dl by the BCP method. An alternate stratification by albumin <4.0 g/dl by the BCG method and <3.7 g/dl by the BCP method was also tested. Each albumin stratification method was tested independently of the other in multivariate models. Mean hemoglobin, nPCR and spKt/V were analyzed as continuous variables.
Cause of ESRD was categorized as congenital/urologic versus other identified causes combined (focal and segmental glomerulosclerosis, glomerulonephritis, systemic lupus erythematosus, hypertension or cystic disease). Sub-group analyses were based on age stratified into two groups (10 to <15 years, and 15 to <18 years). To explore the potential influence of differences in short-stature patients who did and did not have reported data on rhGH, characteristics of short-stature patients were compared by their missing data status.
Differences in clinical and demographic data were determined with two-tailed Student’s t -test of continuous data or χ2 test of proportions. Simple and multivariate logistic regression models determined odds ratios (OR). Models were constructed in a forward stepwise manner to identify those variables that were most strongly associated with the outcome. Only those variables that showed a statistically significant association with the outcome on multivariate model building were retained in the model as model building progressed. The final multivariate model is adjusted only for the included variables rather than for all variables tested.
A 95% confidence interval [95% CI] was calculated for each parameter. A p value of <0.05 was considered statistically significant. Data analyses were conducted using SAS v. 8.02 (SAS Institute, Cary, NC, USA) and SPSS for Windows, v.10.0 (Statistics, Chicago, IL, USA).
Results
Six hundred and fifty-one of 710 (92%) pediatric hemodialysis patients who were reported on dialysis as of December 31, 2001 met inclusion criteria for analysis. Thirty-six patients (5.1%) had forms submitted to CMS but were excluded because clinical information was incomplete. Twenty-three patients (3.2%) were excluded because a form was not received by CMS. The demographics and clinical parameters of included patients are listed in Table 1.
There were 266 patients (41%) with short stature. Compared with patients who had Ht SDS ≥−1.88, patients who had short stature had lower BMI (19.80 vs 21.42; p <0.01), higher spKt/V (1.61 vs 1.50; p <0.001) and higher nPCR (1.19 vs 1.06; p <0.001). Patients with short stature were more likely to be cared for by a pediatric nephrologist than by an internist (79% vs 67%; p <0.001). Patients with and without short stature did not differ in regards to mean values of hemoglobin, serum albumin, total serum calcium or serum phosphate. Short-stature patients tended to have higher mean intact PTH than patients without short stature, although the difference did not obtain statistical significance ( p =0.07).
In patients aged 10 to <15 years, variables included in a final multivariate model predicting short stature are shown in Table 2. The odds ratio of short stature was increased in patients with female gender (OR 2.9; 95% CI, 1.1–7.1; p <0.05), black race (OR 3.2; 95% CI, 1.2–9.1; p <0.05), Hispanic ethnicity (OR 4.5; 95% CI, 1.3–15.3; p <0.05), congenital or urologic causes of ESRD (OR 5.4; 95% CI, 2.1–13.8; p <0.001), each additional year on dialysis (OR 1.2; 95% CI, 1.1–1.4; p <0.01), and with each 0.1 g/kg/day increase in nPCR (OR 1.3; 95% CI, 1.1–1.5; p <0.01).
In patients aged 15 to <18 years, variables included in a final multivariate model predicting short stature are shown in Table 3. The odds of short stature were increased in patients with male gender (OR 2.6; 95% CI, 1.3–5.2; p <0.01), congenital or urologic causes of ESRD (OR 2.8; 95% CI, 1.5–5.4; p <0.01), each additional year on dialysis (OR 1.2; 95% CI, 1.1–1.4; p <0.001), each 0.1 unit increase in spKt/V (OR 1.2; 95% CI, 1.1–1.4; p <0.001), and each 1 g/dl decrease in mean hemoglobin (OR 1.3; 95% CI, 1.04–1.6; p <0.05). Mean serum albumin <3.2/3.5 g/dl (BCP/BCG) was not associated with short stature in either age group.
Of the 266 short stature patients, 214 (80.5%) had information on rhGH use. Eighty (37%) had been prescribed rhGH. Compared with short-stature patients who did not receive rhGH, those prescribed rhGH had lower BMI (18.51 vs 20.07; p <0.05). Mean Ht SDS, spKt/V, hemoglobin, serum albumin, serum total calcium, serum phosphate, intact PTH (iPTH), nPCR and specialty of nephrologist did not differ between the rhGH treated and untreated groups (Table 4).
By simple logistic regression analysis, white short-stature patients were more likely to be treated with rhGH compared with black patients with short stature (OR 1.86; 95% CI, 1.01–3.42; p <0.05). Gender, ethnicity, etiology of ESRD, mean hemoglobin, mean spKt/V, mean nPCR and mean serum albumin did not predict use of rhGH in short-stature patients. When patients were stratified by a serum albumin above and below 4.0/3.7 g/dl (BCG/BCP), patients with higher serum albumin were more likely to be treated with rhGH than those with serum albumin <4.0/3.7 g/dl (BCG/BCP) (OR 1.79; 95% CI, 1.02–3.15; p <0.05). Stratifying spKt/V using a cutoff of 1.2 did not predict use of rhGH. In short-stature patients, every year on dialysis increased the likelihood of receiving rhGH (OR 1.12, 95% CI, 1.04–1.20; p <0.01). Every 1-year increase in age decreased the odds of receiving rhGH, although it was not statistically significant (OR 0.93; 95% CI, 0.87–1.01; p =0.07).
After adjustment for age, gender, race, ethnicity, BMI quartile, etiology of ESRD, years on dialysis, specialty of supervising nephrologist, mean hemoglobin, mean spKt/V, mean nPCR, and mean serum albumin <3.5/3.2 and <4.0/3.7 g/dl (BCG/BCP), only race, BMI and years since initiating dialysis were significantly predictive of use of rhGH in short-stature patients (Table 5). Short-stature white patients were 2.1 times more likely to have used rhGH compared with black patients (OR 2.1; 95% CI, 1.1–4.0; p <0.05). For every 1 year on dialysis, the odds of receiving rhGH increased by 13% (OR 1.13; 95% CI, 1.05–1.22; p <0.01). Short-stature patients with BMI <16.6 kg/m2 were 3.1 times more likely (OR 3.1; 95% CI, 1.2–8.4; p <0.05) to have received rhGH than patients in the highest quartile of BMI (>21.7 kg/m2). Short-stature patients with BMI 16.6–18.6 kg/m2 (OR 2.3; 95% CI, 0.86–6.3; p =0.10) and 18.7–21.7 kg/m2 (OR 2.2; 95% CI, 0.79–6.2; p =0.13) also were more likely to have received rhGH than those in the highest quartile of BMI, although the results were not significant.
Missing data patterns on rhGH use in short-stature patients differed with respect to height z -score, age, BMI, etiology of ESRD and iPTH. Short-stature patients who did not have rhGH data reported ( n =52; 19.5%) were shorter than those with data reported (Ht SDS −3.89±2.07 vs −3.36±1.21; p =0.02). Short-stature patients with missing rhGH data were also older (15.2±2.5 years vs 13.6±3.7 years; p <0.01), more likely to have congenital / urologic causes of their ESRD (70% vs 47%; p =0.01) and had higher BMI (21.1±5.0 kg/m2 vs 19.5±4.6 kg/m2; p <0.05) and iPTH (831.5±703.9 pg/ml vs 505.5±524.7 pg/ml; p =0.001) compared with those with reported data.
Discussion
Optimizing growth and development is a major goal in the care of pediatric CKD and ESRD patients. The aim of the ESRD CPM Project is to assist the evaluation of care provided to ESRD patients and to focus efforts on improving that care. Growth retardation in pediatric ESRD is multifactorial, with relative growth hormone resistance one of many reasons for poor growth, in addition to poor nutrition, acidosis, anemia, osteodystrophy and inflammation. Despite the availability of rhGH, improved management of anemia, treatment of renal osteodystrophy and attention to nutritional status, 41% of pediatric patients receiving HD in the USA in the last quarter of 2001 still had short stature.
In the adolescent population, short stature was predicted by factors associated with long duration of chronic kidney disease—congenital or urologic etiologies of ESRD and increasing number of years on dialysis. With the early onset of CKD in patients with congenital or urologic etiologies of ESRD, their short stature may stem from poor growth at younger ages in the period of time before dialysis initiation.
The association of gender, ethnicity, race, mean hemoglobin, spKt/V and nPCR with short stature differed among age groups in the adolescent population. Short-stature patients had lower BMI and achieved higher spKt/V and nPCR than patients with height SDS ≥ −1.88. As spKt/V is calculated with an estimation of total body water that depends on weight, the higher spKt/V achieved in these patients may reflect their smaller body mass. The decreased odds of short stature in males aged 10–14 years and the increased odds in the 15–18 year-old males may reflect the choice of age-group stratification at a time of the normal increase in adolescent male height velocity, which may lessen the comparative impact of growth retardation in the lower age group and augment it in the older age group.
Short-stature patients were more likely to be cared for by a pediatric nephrologist than by an internist nephrologist. Internist-supervised dialysis centers may not have the equipment or staff expertise to dialyze and care for patients with smaller body size. However, when internist nephrologists do care for short-stature pediatric patients, there was no significant difference in their rhGH prescription patterns compared with their pediatric counterparts (30% vs 39%, respectively; p =0.374). In multivariate analysis, specialty of the attending nephrologist was not associated with prescription of rhGH to short-stature pediatric patients. The higher proportion of short-stature patients in pediatric practices compared with internist practices may have confounded the significant difference observed between pediatrician and internist rhGH prescribing practices in a smaller population of pediatric dialysis patients in Texas [8].
While short stature may not in and by itself account for poor clinical outcomes, it does appear to be a marker for patients at risk. Poor growth and short stature has been associated with decreased survival among pediatric dialysis and transplant patients [14], increased hospitalization rates and poor school attendance [15]. The factors associated with rhGH treatment in short-stature patients may help clinicians focus attention on other intermediate outcomes in these at-risk patients.
More than 50% of short-stature pediatric HD patients did not receive rhGH during the study period. The increased odds of being prescribed rhGH as time on dialysis increased were independent of age and suggest that patients who have been on dialysis longer have more opportunity to be considered candidates for rhGH. Patients were less likely to receive rhGH as their BMI increased, independent of age and gender. The collinearity of BMI with weight and height would suggest that clinicians are less likely to prescribe rhGH for children as their weight or the severity of their short stature increases. Since univariate analysis did not reveal a difference between the height z -scores of short-stature patients stratified by rhGH use (mean Ht SDS in rhGH prescribed vs not-prescribed group, −3.30±1.05 vs −3.40±1.30; p =0.53), the association of increased BMI and decreased odds of using rhGH in this population must be due to weight differences. As weight increases, clinicians may be falsely reassured on overall growth. This finding, along with the fact that nPCR and mean serum albumin did not predict rhGH use, argues against poor nutrition being a barrier to rhGH use.
As with other aspects of care for US pediatric CKD and ESRD patients [16,17,18], rhGH use among short-stature pediatric HD patients demonstrated racial disparities. In the US pediatric ESRD population, the proportion of short-stature white and black patients receiving rhGH at dialysis initiation was similar (10.4% vs 9.3%), but a difference developed as time since dialysis initiation progressed (23.1% vs 14.7% at 6 months; 28.1% vs 18.7% at 12 months) [7]. In this study, the racial disparity in rhGH use among short-stature HD patients was independent of other clinical factors. Other unmeasured factors, including patient and family wishes and socioeconomic barriers, should be evaluated to uncover the reason for this disparity.
Age was not found to be a significant predictor of rhGH use in short-stature patients. This result is surprising, since clinicians would seem less likely to prescribe rhGH to older patients with greater likelihood of having closed physes since the effectiveness of rhGH depends on the growth potential of the physis. The level of intact PTH also was not predictive of rhGH use in short-stature patients. The pattern of rhGH use in this study does not reflect the clinical concern about hyperparathyroidism and increased risk of rhGH-associated slipped capital femoral epiphyses and avascular necrosis of the femoral head.
There are several limitations to the data and this study. The definition of short stature was based on NHANES data and CDC growth charts that reflect the multiethnic makeup of US children in 2000. Individual ethnicities may have different height norms. The pediatric HD population in 2001 had a significantly higher percentage with Hispanic ethnicity (26%) than the US pediatric population (9%) used as the reference [19].
The 3-month data collection period may not reflect actual practice patterns regarding rhGH use. The questionnaire did not specify whether the patient was currently receiving rhGH or had ever received rhGH. Neither the standard nor supplemental questionnaire collected data on information commonly used in practice to guide prescription of rhGH. Bone age, presence of fused physes, history of avascular necrosis or slipped capital femoral epiphyses, prior adverse effects with rhGH use and patient and/or family desire were not assessed. In addition, clinicians’ thresholds for withholding rhGH based on specific levels of PTH were not assessed. These factors are presumed to be more robust predictors of the use of rhGH in clinical practice. Estimates of skeletal maturity likely confounded the relationship of age and rhGH use seen in this study.
The 20.5% of short-stature patients with missing data on rhGH is a potential source of selection bias. Bivariate analysis showed that those with missing data were not representative of the entire short-stature study population. Their exclusion from analysis could either attenuate or magnify the obtained ORs of the clinical and laboratory factors. The study also could not evaluate rhGH use among patients who had short stature before the study period but had responded to rhGH with improved linear growth. A selection bias among the remaining short-stature patients may exist, with an overrepresentation of patients who had not responded to rhGH in the past or who had been determined to be poor candidates for rhGH based on skeletal survey, sexual maturity rating or prior adverse events with rhGH.
Conclusion
A high proportion of pediatric HD patients have short stature, and poor growth at initiation and while on dialysis remains an outcome that needs improvement. In this study, we have shown that recombinant human growth hormone is an underutilized therapy in the pediatric HD population. We have also identified black race, increased BMI and recent dialysis initiation as factors that are associated with decreased rhGH use in short-stature pediatric HD patients. Attention to these associations should be included in the management of linear growth that includes attention to nutrition, treatment of anemia, knowledge of mid-parental height and degree of skeletal maturity, and patient and family wishes. Larger body size should not preclude evaluation of linear growth and the potential of benefit from rhGH. Likewise, race should not be a barrier to rhGH use and the potential economic, cultural and societal etiologies of racial disparities in prescribing patterns should be investigated. Identifying potential rhGH underutilization in pediatric ESRD patients cannot fully address the growth issues in this prevalent population, and the high frequency of short stature indicates the importance of improving growth outcomes before short stature develops and before progression to ESRD.
References
Furth SL, Hwang W, Yang C, Neu AM, Fivush BA, Powe NR (2002) Growth failure, risk of hospitalization and death for children with end-stage renal disease. Pediatr Nephrol 17:450–455
Vimalachandra D, Craig JC, Cowell C, Knight JF (2001) Growth hormone for children with chronic renal failure. Cochrane Database Syst Rev CD003264
Haffner D, Schaefer F, Nissel R, Wuhl E, Tonshoff B, Mehls O (2000) Effect of growth hormone treatment on the adult height of children with chronic renal failure. German Study Group for Growth Hormone Treatment in Chronic Renal Failure. N Engl J Med 343:923–930
Haffner D, Wuhl E, Schaefer F, Nissel R, Tonshoff B, Mehls O (1998) Factors predictive of the short- and long-term efficacy of growth hormone treatment in prepubertal children with chronic renal failure. The German Study Group for Growth Hormone Treatment in Chronic Renal Failure. J Am Soc Nephrol 9:1899–1907
Berard E, Crosnier H, Six-Beneton A, Chevallier T, Cochat P, Broyer M (1998) Recombinant human growth hormone treatment of children on hemodialysis. French Society of Pediatric Nephrology. Pediatr Nephrol 12:304–310
Neu AM, Ho PL, McDonald RA, Warady BA (2002) Chronic dialysis in children and adolescents. The 2001 NAPRTCS Annual Report. Pediatr Nephrol 17:656–663
Seikaly MG, Ho PL, Emmett L, Fine RN, Tejani A (2003) Chronic renal insufficiency in children: the 2001 Annual Report of the NAPRTCS. Pediatr Nephrol 18:796–804
Tai TW, Kalia A (2001) A baseline study of pediatric dialysis in Texas. Pediatr Nephrol 16:1002–1010
Fujisawa Y, Kida K (1996) Effect of growth hormone (GH) therapy on parathyroid hormone metabolism in a girl with GH deficient short stature and chronic renal failure. J Pediatr Endocrinol Metab 9:555–558
Watkins SL (1996) Does renal osteodystrophy develop and/or progress during the course of rhGH treatment? Br J Clin Pract Suppl 85:59–60
Fine RN (1997) Growth hormone treatment of children with chronic renal insufficiency, end-stage renal disease and following renal transplantation—update 1997. J Pediatr Endocrinol Metab 10:361–370
Daugirdas JT (1995) Simplified equations for monitoring Kt/V, PCRn, eKt/V, and ePCRn. Adv Ren Replace Ther 2:295–304
Goldstein SL (2001) Hemodialysis in the pediatric patient: state of the art. Adv Ren Replace Ther 8:173–179
Wong CS, Gipson DS, Gillen DL, Emerson S, Koepsell T, Sherrard DJ, Watkins SL, Stehman-Breen C (2000) Anthropometric measures and risk of death in children with end-stage renal disease. Am J Kidney Dis 36:811–819
Furth SL, Stablein D, Fine RN, Powe NR, Fivush BA (2002) Adverse clinical outcomes associated with short stature at dialysis initiation: a report of the North American Pediatric Renal Transplant Cooperative Study. Pediatrics 109:909–913
Furth SL, Hwang W, Neu AM, Fivush BA, Powe NR (2003) Effects of patient compliance, parental education and race on nephrologists’ recommendations for kidney transplantation in children. Am J Transplant 3:28–34
Hidalgo G, Tejani C, Clayton R, Clements P, Distant D, Vyas S, Baqi N, Singh A (2001) Factors limiting the rate of living-related kidney donation to children in an inner city setting. Pediatr Transplant 5:419–424
Furth SL, Garg PP, Neu AM, Hwang W, Fivush BA, Powe NR (2000) Racial differences in access to the kidney transplant waiting list for children and adolescents with end-stage renal disease. Pediatrics 106:756–761
Kuczmarski RJ, Ogden CL, Grummer-Strawn LM, Flegal KM, Guo SS, Wei R, Mei Z, Curtin LR, Roche AF, Johnson CL (2000) CDC growth charts: United States. Adv Data 314:1–27
Author information
Authors and Affiliations
Corresponding author
Additional information
The views expressed in this manuscript are those of the authors and do not necessarily reflect official policy of the Centers for Medicare & Medicaid Services. This article was co-authored by LCDR Gregory H. Gorman, MC, USNR, while a Fellow in Pediatric Nephrology at the Johns Hopkins Medical Institutions. The views expressed in this article are those of the authors and do not reflect the official policy or position of the Department of the Navy, Department of Defense, or the US Government
Rights and permissions
About this article
Cite this article
Gorman, G., Fivush, B., Frankenfield, D. et al. Short stature and growth hormone use in pediatric hemodialysis patients. Pediatr Nephrol 20, 1794–1800 (2005). https://doi.org/10.1007/s00467-005-1893-x
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00467-005-1893-x