Abstract
We have examined, in a randomized crossover trial, the antiproteinuric effect of treatment with low- (0.2 mg/kg daily) and high-dose (0.6 mg/kg daily) enalapril in 25 consecutive patients with steroid-resistant nephrotic syndrome (SRNS). Patients in group A (n=11) received enalapril at low doses for 8 weeks, followed by 2 weeks of washout and then at high doses for 8 weeks. Those in group B (n=14) initially received enalapril at high and then low doses. Patients continued to receive treatment with tapering doses of prednisolone; none received concomitant therapy with daily oral or intravenous steroids, alkylating agents, cyclosporine, non-steroidal anti-inflammatory drugs, and other antihypertensive medications. The urine albumin-to-creatinine (Ua/Uc) ratio and the percentage reduction were determined for each phase of therapy. Baseline clinical, biochemical, and histological features were comparable in the two groups. In the first phase, treatment with low-dose enalapril (group A) resulted in median 34.8% Ua/Uc reduction compared with 62.9% with high doses (group B) (P<0.01). High-dose enalapril was associated with a significant reduction in Ua/Uc ratio in both groups. The combined median Ua/Uc (95% confidence interval) reduction in the low-dose phase was 33% (−10.3% to 72.4%) and in the high-dose 52% (15.4%–70.4%) (P<0.05). The median Ua/Uc ratio at the end of 20 weeks was 1.1 and 1.8 in groups A and B, respectively (P>0.05). Systolic and diastolic blood pressure reductions were similar in both groups. No period or carry-over effect was found. Prolonged treatment with enalapril thus resulted in a dose-related reduction in nephrotic-range proteinuria. Titration of the dose of enalapril may be a useful strategy for achieving substantial reduction of proteinuria in children with SRNS.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Most children with nephrotic syndrome respond to corticosteroid therapy with remission of proteinuria. Approximately 10%–15% patients who do not respond to such treatment are defined as having steroid resistance [1]. Persistent proteinuria in patients with steroid-resistant nephrotic syndrome (SRNS) results in severe hypoalbuminemia, edema, hyperlipidemia, and recurrent infections. Proteinuria is also considered a risk factor for progression of glomerulosclerosis [2]. Experimental studies show that persistent nephrotic-range proteinuria induces an increased synthesis of vasoactive and proinflammatory substances, the appearance of cellular infiltrates, tubulointerstitial fibrosis, and progressive renal disease [2]. Interventions to reduce proteinuria are therefore likely to be beneficial both in the short- and long-term management of patients with SRNS.
A number of clinical studies have confirmed the antiproteinuric effect of angiotensin-converting enzyme (ACE) inhibitors in adults with glomerular diseases [3, 4]. The experience in children is limited to a few case series involving small numbers of patients [5, 6, 7, 8, 9, 10]. While studies in adults suggest that the antiproteinuric effect of these drugs might be dose related [11], the dose for an optimal antiproteinuric effect has not been examined in children. In view of the lack of pediatric data, dosages for an antiproteinuric response have been empirically based on their dose-response for blood pressure. Enalapril has thus been used at doses between 0.2 and 0.6 mg/kg per day [8, 9, 10]. These doses are effective and well tolerated in most instances.
Considering the benefits of proteinuria reduction and lack of data on the dosage of ACE inhibitors, we have investigated, in a randomized crossover trial, the antiproteinuric effect of treatment with low- and high-dose enalapril in patients with SRNS.
Patients and methods
Patients with idiopathic SRNS, between the age of 1 and 16 years, attending the Pediatric Nephrology Services of this hospital between August 1998 and December 1999, were eligible for the study. Patients with initial as well as late resistance were included. Initial steroid resistance was defined as absence of remission of proteinuria despite treatment with prednisolone at a daily dose of 2 mg/kg for 4 weeks, followed by 1.5 mg/kg on alternate days for another 4 weeks. Those who responded initially but failed to respond to daily treatment during a subsequent relapse were defined as having late resistance. Remission was defined as urine showing nil or traces of protein by Dipstix examination on 3 consecutive days [12]. It is our policy to obtain renal histology in patients showing initial or late steroid resistance.
The exclusion criteria were: (1) severe hypertension (systolic or diastolic blood pressure that was above the 99th percentile for the age and sex) [13]; (2) glomerular filtration rate below 70 ml/min per 1.73 m2 [14]; (3) secondary nephrotic syndrome, e.g., systemic lupus erythematosus, Henoch-Schonlein purpura, hepatitis B infection, and amyloidosis; (4) single functioning kidney; and (5) concurrent or previous treatment with daily or intravenous corticosteroids, alkylating agents, levamisole, cyclosporine, or intravenous albumin in the preceding 4 weeks. Patients living more than 50 km from the hospital or those unable to come for 4-weekly follow-up visits were also excluded.
Study design
A prospective, randomized, crossover design was chosen to eliminate inter-patient variations. Informed consent was obtained from the parents. The Department Review Committee approved the study.
Patients continued to receive alternate-day prednisolone during the study. Diuretics (furosemide) were used, if indicated, for control of significant edema. Treatment with non-steroidal anti-inflammatory drugs and calcium channel and beta-adrenergic blockers was discontinued. All patients entered a 2-week washout period to eliminate the effect of previous therapy. Before starting therapy with enalapril, height, weight, and blood pressure were measured. Hypertension was defined as blood pressure more than the 95th percentile for age and sex [13].
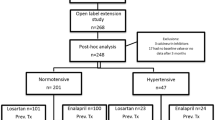
Computer-generated random numbers were used to randomly allocate patients to groups A or B. Patients in group A received low-dose (0.2 mg/kg per day) enalapril for 8 weeks, followed by 2 weeks of washout and finally high-dose enalapril (0.6 mg/kg per day) for another 8 weeks. Those in group B received high-dose enalapril for the first 8 weeks, followed by 2 weeks of washout and then low-dose enalapril for 8 weeks (Fig. 1). Enalapril was administered in two divided doses. All patients were on a salt-restricted diet and were instructed not to change their protein intake during the study. Urinary urea and sodium were used as markers of dietary protein and sodium intake, respectively.
Follow-up visits were scheduled at 2, 6, 10, 12, 16, and 20 weeks. At each visit, weight, height, and blood pressure were measured. Blood levels of urea, creatinine, electrolytes, albumin, and cholesterol were determined. Urinary excretion of albumin, creatinine, sodium, and urea were measured using a 6-h urine specimen. The urine albumin-to-creatinine ratio (Ua/Uc) was calculated at each visit. The percentage Ua/Uc reduction was determined for each phase of therapy. For example, the Ua/Uc reduction percentage for the first phase of therapy was:
In order to further examine the effect of enalapril dosage, the Ua/Uc reduction percentage was compared using combined data of the high-dose and low-dose phases of both groups.
Significant reduction was arbitrarily defined as a Ua/Uc reduction percentage of more than 40% at the end of 18 weeks of treatment with enalapril. We investigated whether there were any differences in the characteristics of patients who showed a significant reduction in proteinuria compared with those who did not.
Statistical analysis
Statistical analysis was performed using the software package Stata 6.0 [15]. Descriptive analysis was performed for baseline parameters. Values represent median (95% confidence interval) unless specified. Chi-squared test, Wilcoxon rank-sum and signed rank tests were applied as appropriate. P<0.05 was considered significant.
Analysis of the crossover trial
The ‘period effect’ was determined to assess whether the severity of nephrotic syndrome had altered during the study. The ‘carry-over effect’ was estimated to examine if the washout was effective and exclude the effect of previous therapy [16]. Since these tests are inherently weak, P<0.1 was considered significant.
Results
Twenty-nine patients with idiopathic SRNS were enrolled and randomized to groups A (n=14) and B (n=15). Four patients (3 and 1 in groups A and B, respectively) who did not attend the first follow-up appointment were excluded. The baseline clinical and biochemical parameters of subjects in groups A (n=11, 9 boys) and B (n=14, 9 boys) are shown in Table 1. While the age at onset and inclusion into the study was lower in group B, the differences were not statistically significant. Renal histology was suggestive of minimal change disease, focal segmental glomerulosclerosis, membranoproliferative glomerulonephritis, and mesangioproliferative glomerulonephritis in 1, 4, 4, and 2 and 3, 5, 3, and 3 patients in groups A and B, respectively.
Patients in group A initially received enalapril at a low dose (mean 0.21±0.03, range 0.16–0.27 mg/kg per day) followed by high-dose therapy (0.62±0.09, range 0.54–0.77 mg/kg per day). Patients in group B received enalapril at a high dose (0.61±0.08, range 0.53–0.76 mg/kg per day) followed by low-dose therapy (0.23±0.01, range 0.18–0.26 mg/kg per day).
Low-dose versus high-dose enalapril
The sequential 6-h urinary albumin excretion and Ua/Uc ratios are shown in Table 2. Both were similar in groups A and B at baseline (P=0.6) and at the end of the study (P=0.6, Wilcoxon rank sum test).
High-dose enalapril was associated with a significant reduction in Ua/Uc ratio in groups A and B (P<0.01 and 0.001, respectively). Considering only the initial 10 weeks of the study, before crossover, the Ua/Uc reduction percentage was significantly greater in patients receiving high-dose enalapril (group B) than in those receiving low-dose enalapril (group A) (Table 3). A similar difference was found between high-dose and low-dose treatment within group B. However, differences within group A, between high- and low-dose therapies, were not significant. It is noteworthy that the urinary albumin excretion and Ua/Uc ratios continued to decline throughout the study (Table 2). The Ua/Uc ratio at the end of 20 weeks was 1.1 and 1.8 in groups A and B, respectively (P=0.6).
Following enalapril therapy, the 6-h urine albumin excretion decreased by 74.2% each in groups A and B. Blood levels of albumin increased by 46.9% in group A and 28.1% in group B at 20 weeks (Table 4). A significant increase in albumin levels was found within 8 weeks of enalapril therapy in patients of group A (P<0.005). Blood levels of cholesterol declined by 22.1% and 21.7% in groups A and B, respectively.
Combined data from both groups showed a median Ua/Uc reduction percentage of 52% (15.4%–70.4%) and 33% (−10.3% to 72.4%) during high-dose and low-dose phases, respectively. These differences were statistically significant (P<0.05).
Enalapril therapy resulted in a reduction of systolic and diastolic blood pressure in both groups. The median systolic and diastolic blood pressures were 120 mm and 80 mmHg at baseline and declined to 114.3 and 74.4 mmHg, respectively, after 8 weeks of therapy in group A (P<0.05). In group B, the systolic and diastolic pressures were 110 mmHg and 70 mmHg at baseline, and 106 mmHg and 65.4 mmHg, respectively, after 8 weeks. There was a slight increase in blood pressure during the washout period, followed by a similar decline during the next 8 weeks. The dose of enalapril did not influence the percentage reduction in systolic and diastolic blood pressure, which was similar at the end of 8 and 16 weeks of treatment in both groups. Urinary levels of urea and sodium remained similar through the study period, indicating no effect of dietary protein and sodium on the observed efficacy of enalapril. No period or carry-over effect (P>0.5) was demonstrated. Three patients receiving enalapril had a dry cough that subsided after stopping the treatment.
Determinants of response
Of 25 subjects, 17 had a significant reduction in proteinuria. There were no differences in the age, sex, renal histology, presence of hypertension, and change in systolic or diastolic blood pressure and serum creatinine in patients showing a significant reduction in proteinuria. The median Ua/Uc percentage reduction following 18 weeks of treatment was 48.1% (20.9%–78.7%) and 46.2% (33.4%–79.1%) in patients with and without hypertension, respectively (P=0.8). The baseline Ua/Uc ratio was higher [median 5.9 (2.7–12)] in patients who showed more than a 40% reduction of proteinuria [median 3.1 (1.3–5.0)] (P=0.08).
Discussion
We have prospectively examined the antiproteinuric efficacy of low- and high-dose enalapril in children with SRNS. Data following the initial 8 weeks showed that treatment with enalapril at 0.6 mg/kg per day resulted in an almost twofold higher Ua/Uc percentage reduction compared with 0.2 mg/kg per day. The antiproteinuric effect declined following reduction of the enalapril dose (Table 3, group B) (P<0.01). The dose-related differences persisted when results from low and high-dose phases of both groups were combined. Thus, the antiproteinuric effect of enalapril appears dose related at the dosage used in this study. The absence of period and carry-over effects further suggests that our analysis is valid. Therapy was safe and well tolerated in both groups.
These findings are similar to others, which show a 50%–80% decline in proteinuria in children with nephrotic syndrome [5, 6, 7, 8, 9]. A recent meta-analysis, in adult subjects, found that therapy with ACE inhibitors resulted in a 40% (95% confidence interval 36.8%–42.8%) reduction in proteinuria [3]. Contrary to a previous report [11], we noted a stronger antiproteinuric effect in subjects with higher baseline proteinuria. It is possible that this phenomenon is similar to systemic hypertension, where the highest percentage reductions occur in individuals starting with the highest blood pressures.
It is unlikely that the reduction in urinary albumin excretion in our patients was due to a spontaneous change in the course of the disease. The duration of steroid resistance, before institution of therapy with enalapril, ranged from 6 to 96 months. None of the patients simultaneously received specific therapy, apart from alternate-day steroids, which could induce reduction in proteinuria. The subjects ingested an almost-constant diet in terms of total calories, protein, and salt. The observed benefits could thus not be attributed to dietary changes, and represent the effect of enalapril.
The mechanism of the antiproteinuric effect of ACE inhibitors is not clearly understood. Reduction of systemic and intraglomerular pressures [17] and improved size selectivity of glomerular basement membrane [9, 18] are considered important in mediating this effect. A significant finding supporting the latter mechanism is that, while the hemodynamic effect of ACE inhibition occurs rapidly and is soon stable, the antiproteinuric effect increases with time [11, 19]. In the present study, it was noteworthy that reduction in systolic and diastolic blood pressure occurred in the first 8 weeks of therapy and did not change significantly thereafter. However, the impact of enalapril on albuminuria increased temporally and was similar in patients with or without hypertension.
Previous reports on the antiproteinuric effect of ACE inhibitors also show that reductions of blood pressure and proteinuria are not necessarily concordant [19]. Heeg et al. [11] examined the effect of increasing doses of lisinopril on nephrotic-range proteinuria in adults. Proteinuria fell by 27%-±-20% on low-dose treatment (median 5 mg/day) and by 50%±17% on high-dose (median 10 mg/day) lisinopril. Another study examined the antiproteinuric effect of 5, 10, 15, and 20 mg lisinopril/day in adults with IgA nephropathy [20]. While blood pressure decreased 22% with the lowest dose, no further decrease was seen at higher doses. However, proteinuria progressively decreased by 39%, 44%, 61%, and 67% with increasing doses of lisinopril. Ruggenenti et al. [21] recently showed that treatment with lisinopril ameliorated hypertriglyceridemia and hypercholesterolemia in a dose-dependent manner, particularly in subjects with hypoalbuminemia. Different findings were reported by Haas et al. [22] who found that high doses of spirapril, beyond that necessary for control of hypertension, did not lead to a further reduction in proteinuria.
An important limitation of this trial was that the duration of each course of therapy was limited to 8 weeks and the Ua/Uc ratios were not documented to be stable before changing the dosage. Since the effect of ACE inhibitors increases with time [11], it might be reasoned that the results might represent the effect of time rather than differences in dosage. The present choice of 8 weeks of therapy was based on previous experience showing stability of antiproteinuric effects by 4–10 weeks [11, 19]. Our results during the initial 8 weeks clearly show that treatment with high-dose enalapril had a significantly greater antiproteinuric effect. Statistical analysis of the data did not show evidence of ‘carry-over’ of previous treatment. Therefore, while we believe that our analysis is convincing, time dependency should be considered while evaluating the dose response of ACE inhibitors.
Apart from blood pressure control, reduction of proteinuria is an independent and essential treatment target for renoprotection [23]. Controlled trials have shown that for comparable blood pressure reductions, agents that more effectively decrease proteinuria are more renoprotective [24]. A recent meta-analysis showed that therapy with ACE inhibitors significantly reduced blood pressure and urinary protein excretion, and was associated with slower progression to end-stage renal disease [4]. The benefits of therapy were stronger in those with higher proteinuria at the onset. The mechanism behind the benefits is not clear, but might be related to a greater antiproteinuric effect in subjects with higher baseline proteinuria, as was observed in the present study. Our findings of a 20% decline in blood cholesterol following prolonged administration of enalapril extend those reported previously [5, 8, 19, 21]. Reduction in levels of blood lipids would potentially reduce the risks of progressive renal injury [25] and ischemic heart disease.
Considering the prognostic impact of reduction of proteinuria, we propose that the dosage of enalapril be titrated for antiproteinuric effect. Therapy with enalapril should be begun at a dose of 0.2 mg/kg and gradually increased to 0.5–0.6 mg/kg, aiming to achieve a 40%–50% reduction in proteinuria. While side effects of therapy are unusual, blood levels should be monitored for creatinine and electrolytes. Amelioration of nephrotic-range proteinuria is expected to reduce edema, improve nitrogen balance, and favorably effect the rate of progression of renal disease.
References
Niaudet P (1999) Steroid-resistant idiopathic nephrotic syndrome. In: Barratt TM, Avner ED, Harmon WE (eds) Textbook on pediatric nephrology, 4th edn. Williams Wilkins, Baltimore, pp 749–763
Praga M, Morales E (2002) Renal damage associated with proteinuria. Kidney Int [Suppl] 82:42–46
Gansevoort RT, Sluiter WJ, Hemmelder MH, Zeeuw D de, Jong PE de (1995) Antiproteinuric effect of blood-pressure-lowering agents: a meta-analysis of comparative trials. Nephrol Dial Transplant 10:1963–1974
Jafar TH, Schmid CH, Landa M, Giatras I, Toto R, Remuzzi G, Maschio G, Brenner BM, Kamper A, Zucchelli P, Becker G, Himmelmann A, Bannister K, Landais P, Shahinfar S, Jong PE de, Zeeuw D de, Lau J, Levey AS (2001) Angiotensin-converting enzyme inhibitors and progression of nondiabetic renal disease. A meta-analysis of patient-level data. Ann Intern Med 135:73–87
Trachtman H, Gauthier B (1988) Effect of angiotensin-converting enzyme inhibitor therapy on proteinuria in children with renal disease. J Pediatr 112:295–298
Fitzwater DS, Brouhard BH, Cunningham RJ 3rd (1990) Use of angiotensin converting enzyme inhibitors for the treatment of focal segmental glomerulosclerosis. Am J Dis Child 144:522
Milliner DS, Morgenstern BZ (1991) Angiotensin converting enzyme inhibitors for reduction of proteinuria in children with steroid-resistant nephrotic syndrome. Pediatr Nephrol 5:587–590
Proesmans W, Wambeke IV, Dyck MV (1996) Long-term therapy with enalapril in patients with nephrotic-range proteinuria. Pediatr Nephrol 10:587–589
Delucchi A, Cano F, Rodriguez E, Wolff E, Gonzalez X, Cumsille MA (2000) Enalapril and prednisone in children with nephrotic-range proteinuria. Pediatr Nephrol 14:1088–1091
Lama G, Luongo I, Piscitelli A, Salsano ME (2000) Enalapril: antiproteinuric effect in children with nephrotic syndrome. Clin Nephrol 53:432–436
Heeg JE, Jong PE de, Hem GK van der, Zeeuw D de (1989) Efficacy and variability of the antiproteinuric effect of ACE inhibition by lisinopril. Kidney Int 36:272–279
Indian Pediatric Nephrology Group (2001) Consensus statement on management of steroid sensitive nephrotic syndrome. Indian Pediatr 38:975–986
National Heart, Lung and Blood Institute (1987) Report of the Second Task Force on Blood Pressure Control in Children. Pediatrics 79:1–25
Schwartz GJ, Haycock GB, Edelmann CM Jr, Spitzer A (1976) A simple estimate of glomerular filtration rate in children derived from body length and plasma creatinine. Pediatrics 58:259–263
Stata Corporation (1993) Stata Reference Manual, Release 3.1, 6 edn. College Station, Texas
Pocock SJ (ed) (1986) Clinical trials: a practical approach. Wiley, New York, pp 110–122
Bedogna V, Valvo E, Casagrande P, Braggio P, Fontanarosa C, Dal Santo F, Alberti D, Maschio G (1990) Effects of ACE inhibition in normotensive patients with chronic glomerular disease and normal renal function. Kidney Int 38:101–107
Ruggenenti P, Mosconi L, Vendramin G, Moriggi M, Remuzzi A, Sangalli F, Remuzzi G (2000) ACE inhibition improves glomerular size selectivity in patients with idiopathic membranous nephropathy and persistent nephrotic syndrome. Am J Kidney Dis 35:381–391
Gansevoort RT, Zeeuw D de, Jong PE de (1993) Dissociation between the course of the hemodynamic and antiproteinuric effects of angiotensin I converting enzyme inhibition. Kidney Int 44:579–584
Palla R, Panichi V, Finato V, Parrini M, Andreini B, Bianchi AM, Giovannini L, Migliori M, Bertelli AA (1994) Effect of increasing doses of lisinopril on proteinuria of normotensive patients with IgA nephropathy and normal renal function. Int J Clin Pharmacol Res 14:35–43
Ruggenenti P, Mise N, Pisoni R, Arnoldi F, Pezzotta A, Perna A, Cattaneo D, Remuzzi G (2003) Diverse effects of increasing lisinopril doses on lipid abnormalities in chronic nephropathies. Circulation 107:586–592
Haas M, Leko-Mohr Z, Erler C, Mayer G (2002) Antiproteinuric versus antihypertensive effects of high-dose ACE inhibitor therapy. Am J Kidney Dis 40:458–463
Ruggenenti P, Perna A, Mosconi L, Pisoni R, Remuzzi G (1998) Urinary protein excretion rate is the best independent predictor of ESRF in non-diabetic proteinuric chronic nephropathies. “Gruppo Italiano di Studi Epidemiologici in Nefrologia” (GISEN). Kidney Int 53:1209–1216
Peterson JC, Adler S, Burkart JM, Greene T, Hebert LA, Hunsicker LG, King AJ, Klahr S, Massry SG, Seifter JL (1995) Blood pressure control, proteinuria, and the progression of renal disease. The Modification of Diet in Renal Disease Study. Ann Intern Med 123:754–762
Mulec H, Johnsen SA, Wiklund O, Bjorck S (1993) Cholesterol: a renal risk factor in diabetic nephropathy? Am J Kidney Dis 22:196–201
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Bagga, A., Mudigoudar, B.D., Hari, P. et al. Enalapril dosage in steroid-resistant nephrotic syndrome. Pediatr Nephrol 19, 45–50 (2004). https://doi.org/10.1007/s00467-003-1314-y
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00467-003-1314-y