Abstract
Background
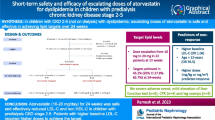
Dyslipidemia is an important cardiovascular risk factor in steroid-resistant nephrotic syndrome (SRNS). Efficacy of statins for treatment of hyperlipidemia in children with SRNS is unclear.
Methods
This prospective, randomized, double-blind, placebo-controlled, parallel-group clinical trial enrolled 30 patients with SRNS, aged 5–18 years, with serum low-density lipoprotein cholesterol (LDL-C) levels between 130 and 300 mg/dl, to receive a fixed dose of atorvastatin (n = 15, 10 mg/d) or placebo (n = 15) by block randomization in a 1:1 ratio. Primary outcome was change in serum LDL-C at 12 months. Change in levels of other lipid fractions, carotid intima-media thickness (cIMT), flow-mediated dilation (FMD) of the brachial artery, and adverse events were also evaluated.
Results
At the end of 12 months, atorvastatin was not superior to placebo in reducing plasma LDL-C levels, median percentage reduction 15.8% and 9.5% respectively, in atorvastatin and placebo arms (n = 14 in each; P = 0.40). Apolipoprotein B levels significantly declined with atorvastatin in modified intention-to-treat analysis (P = 0.01) but not in the per-protocol analysis. There was no significant effect on other lipid fractions, cIMT and FMD. Adverse events were similar between groups. Change in serum albumin was negatively associated with change in serum LDL-C, very low-density lipoprotein cholesterol, total cholesterol, triglyceride, and apolipoprotein B (P < 0.001), irrespective of receiving atorvastatin, age, gender, body mass index, and serum creatinine.
Conclusions
Atorvastatin, administered at a fixed daily dose of 10 mg, was not beneficial in lowering lipid levels in children with SRNS; rise in serum albumin was associated with improvement in dyslipidemia.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Nephrotic syndrome is a risk factor for accelerated atherosclerosis [1]. Dyslipidemia, hypoalbuminemia, hypercoagulable state, hypertension, and steroid-induced obesity contribute to this risk [2]. While these abnormalities resolve with disease remission in steroid responsive patients [3, 4], they persist in children with steroid-resistant nephrotic syndrome (SRNS). Dyslipidemia is an important modifiable risk factor that may also aggravate glomerulosclerosis and contribute to progression of renal injury [5]. Nephrotic syndrome alters pathways involved in the synthesis, transport, remodeling, and catabolism of lipids leading to elevated total cholesterol, triglycerides (TG), apolipoprotein B (apoB)-containing lipoproteins (very low-density lipoprotein [VLDL] and low-density lipoprotein [LDL]), and lipoprotein(a) [6]. Statins inhibit hepatic 3-hydroxy-3-methylglutaryl-CoA (HMG-CoA) reductase. It reduces cholesterol synthesis and upregulates LDL receptors causing clearance of atherogenic LDL cholesterol (LDL-C) and apoB-containing lipoproteins from the circulation [6]. Statins have demonstrated long-term safety and efficacy to reduce LDL-C by 25–35% in children with familial hypercholesterolemia [7, 8]. Beneficial effect on endothelial dysfunction, reflected by reduced progression of carotid intima-media thickness (cIMT) and improved flow-mediated dilation (FMD) of the brachial artery, has been shown in patients with familial hypercholesterolemia [8] and nephrotic syndrome [9] treated with statins. However, a Cochrane systematic review of randomized trials including 191 adults with idiopathic nephrotic syndrome failed to demonstrate superiority of statins over placebo in reducing total and LDL cholesterol [10]. While, various guidelines recommend considering statins in childhood nephrotic syndrome with persistently high fasting LDL-C [1, 11, 12], there is no clear consensus on its use because high-quality evidence from randomized trials is lacking. We therefore proposed to examine, in a prospective randomized controlled trial, whether administration of statins was effective in improving dyslipidemia, cIMT and brachial artery FMD in children with SRNS.
Methods
Trial design
This prospective, randomized, placebo-controlled, parallel-group clinical trial was designed to assess the efficacy of atorvastatin (10 mg/day) to reduce serum LDL-C levels in patients with steroid-resistant nephrotic syndrome. This study was conducted from July 2011 to February 2015 at a tertiary care center following approval by the Institute ethics committee and Drug Controller General of India. The trial was registered at the Clinical Trials Registry of India (http://ctri.nic.in; CTRI 2012/07/002761).
Participants
Patients, aged 5–18 years, with SRNS were screened. Nephrotic syndrome was defined as the presence of nephrotic-range proteinuria (3–4+ proteinuria by dipstick; spot urine protein to creatinine ≥ 2 mg/mg), hypoalbuminemia (albumin < 2.5 g/dl), and edema. Steroid resistance was defined as absence of remission despite treatment with prednisolone at a dose of 2 mg/kg/d for 4 weeks. Patients with LDL-C levels between 130 and 350 mg/dl (detected on two occasions 1 week apart), who were receiving stable doses of immune-suppressive medication for at least 6 months were eligible for randomization. Patients with nephrotic syndrome secondary to systemic lupus or Henoch Schonlein purpura, estimated glomerular filtration rate (eGFR) [13] less than 30 mL/min/1.73 m2, stage 2 hypertension, creatinine kinase (CK) levels more than three times the upper limit of normal, history of jaundice or raised transaminases in the last 6 months, use of lipid-lowering drugs in the previous 3 months, and family history of premature cardiovascular disease (≤ 55 years in men or ≤ 65 years in female [14]) or residence > 250 km away were excluded. Informed written consent was obtained from either parent before enrollment.
Randomization, allocation, and blinding
Allocation sequence was computer generated. Patients were stratified based on degree of proteinuria (≤ 2+ and ≥ 3+ on dipstick) and randomly assigned in a 1:1 ratio, in permuted blocks, to receive either 10 mg atorvastatin (Storvas; Ranbaxy Laboratories) or identical-appearing tablets as a single daily dose on empty stomach. Treatment allocations were concealed in opaque, sealed envelopes that were opened at randomization. Medication, sufficient to last for 12 weeks, was packed in identical containers and labeled with unique serial numbers based on the randomization list, ensuring allocation concealment. Procedures for randomization, packing, and distribution of medications were done by individuals who were not involved in trial implementation. The investigators, patients, and outcome assessors were blinded to the randomization schedule.
Measurements
Patients’ weight and height were recorded; weight-for-age, height-for-age, and body mass index-for-age standard deviation scores (SDS) were derived based on WHO growth references [15]. Blood pressure was measured thrice and mean systolic and diastolic pressures were used to derive corresponding percentiles [16].
Serum total cholesterol, LDL-C, VLDL cholesterol (VLDL-C), high-density lipoprotein cholesterol (HDL-C), triglycerides, apolipoprotein A (apoA), and apolipoprotein B (apoB) were estimated following a 12-h overnight fast. Total cholesterol and triglyceride levels were measured using enzymatic endpoint method [17]. HDL was estimated after precipitation of LDL and VLDL using phosphotungstic acid and magnesium [18]. LDL cholesterol (mg/dl) was calculated as follows [19]:
LDL cholesterol = Total cholesterol − triglyceride/adjustable factor − HDL
where the adjustable factor was established as the strata specific median triglyceride: VLDL-C ratio [19] to adjust for high triglyceride levels in patients with nephrotic syndrome.
Apolipoproteins A, B, and high-sensitivity C-reactive protein (hs-CRP) were estimated by nephelometry (Randox, UK) and sandwich ELISA (BioCheck Inc., Foster City, CA), respectively.
cIMT and brachial artery FMD were determined by the radiologist using high-resolution ultrasonography with multi-frequency linear probe (5–12 MHz) and standard image settings [20]. Bilateral distal common carotid arteries, 1 cm proximal to the bifurcation, were imaged during end diastole, with the patient in supine position and the neck slightly extended. cIMT was defined as the distance between the leading edges of the lumen–intima interface and the media–adventitia interface of the far wall of the carotid artery; mean of two recordings on both side was calculated. Assessment of brachial artery FMD was done after 10-min rest in a temperature controlled room, in fasting state [21]. A blood pressure cuff was applied to the widest part of the forearm below the antecubital fossa, inflated to 50 mmHg above systolic BP and deflated after 4 min. Images were obtained at baseline, following inflation, immediately after deflation and 90 s after deflation; maximum dilatation was recorded. The change in the diameter of brachial artery from the baseline expressed as a percentage of the baseline diameter represented the FMD. All studies were done by a single radiologist; the intra-observer coefficient of variation of cIMT and brachial FMD at our center is 1.9% and 2.2%, respectively.
Follow-up
Patients were evaluated for blood pressure, evidence of infection, and adverse effects during follow-up at 1, 3, 6, 9, and 12 months. Blood counts and levels of lipids, creatinine, albumin, electrolytes, aspartate and alanine aminotransferase (AST, ALT), alkaline phosphatase, CK, hs-CRP, and 24-h urine protein were measured at each visit. cIMT and brachial artery FMD were done at baseline, 6 months and 12 months.
Patients in both groups were instructed to take the National Cholesterol Education Program (NCEP) Step 1 diet (less than 300 mg cholesterol and less than 30% of total calories from fat, of which less than 10% was saturated fat) throughout the trial period. Diet charts were provided, and dietary intake was evaluated at each follow-up visit by dietary recall to ensure compliance. Enalapril (0.2 to 0.5 mg/kg) or additional treatment with amlodipine (0.1 to 0.3 mg/kg/d) was instituted to control blood pressure. All patients received daily supplements of calcium carbonate (250 to 500 mg) and vitamin D.
Outcomes
The primary outcome was the percent change in levels of LDL-C at 12 months. Secondary outcomes at 12 months were (i) percent change in levels of total cholesterol, triglycerides VLDL-C, HDL-C, apoA, and apoB; (ii) percent change in brachial artery FMD and cIMT; and (iii) frequency and type of adverse events. Safety assessments included clinical and laboratory evaluation and monitoring for adverse events, with reports to the ethics committee. Criteria for withdrawal from study were LDL-C > 350 mg/dl (confirmed on two occasions 1 week apart), elevation of CK level more than 3 times or AST/ALT level more than twice the upper limit of normal persisting on two consecutive measurements 2 weeks apart, and eGFR < 30 mL/min/1.73 m2 or a serious adverse event.
Statistical analysis
Continuous data were expressed as median (interquartile range) or mean ± SD. Data were analyzed by Pearson’s chi-square or Fisher’s exact test, as appropriate. Wilcoxon rank-sum test or Student’s t test were used for comparison. Generalized estimating equations (GEE) were used to analyze predictors of serial values of lipids over 12 months. Linear regression on log-transformed variables was used to evaluate association of change in cIMT and FMD with lipid levels and atorvastatin administration. Data was analyzed using Stata version 14.0 (StataCorp 2015); P < 0.05 was considered significant.
For calculation of sample size, we assumed a reduction of 25% in the LDL-C in atorvastatin-treated group and 5% in placebo group following NCEP step 1 diet. On the basis of a previous study that showed the mean LDL-C level in children with SRNS was 163 ± 20 mg/dl [22], 12 subjects were required in each group to detect a difference of 20% between the groups with an alpha error of 0.05 and power of 90%. Assuming a drop out of 10%, sample size of 28 subjects was estimated (Stata version 11.0; StataCorp 2009). Since primary outcome was change in levels of LDL-C from baseline, analyses were based on modified intention-to-treat approach that included all randomized participants who had at least one post-baseline measurement to calculate the primary outcome; last observation was carried forward. We also report per-protocol analyses on patients who were followed up for 12 months.
Results
Of 60 patients assessed, 30 were excluded (25 did not meet eligibility criteria, and 5 did not consent; Fig. 1). Of the 30 randomized participants, 15 were assigned to receive treatment with atorvastatin and 15 with placebo. Four patients were lost to follow-up (two in placebo, two in intervention group) and therapy discontinued in another three. Discontinuation of therapy was due to lower respiratory tract infection in one patient in the placebo group and reduction of eGFR < 30 ml/1.73m2/min in two patients in the intervention arm. Since two patients did not return after the randomization visit, primary outcome data was analyzed in 28 patients using modified intention-to-treat analysis.
Baseline characteristics
Children aged 11.6 ± 3.6 years, predominantly boys (70%), were randomized to receive 10 mg atorvastatin daily or placebo. Baseline parameters were similar between the groups (Table 1). Twenty percent patients were younger than 10 years of age. The renal histology included minimal change disease (MCD, 9), focal segmental glomerulosclerosis (FSGS, 9), membranoproliferative glomerulonephritis (MPGN, 11), and membranous nephropathy (1). Mean duration of disease was 50 ± 37 months. None were receiving calcineurin inhibitors during study period; patients either discontinued calcineurin inhibitors at least 6 months prior to enrolment (N = 27) or received only 0.2–0.3 mg/kg of alternate day oral prednisolone for sub-nephrotic-range proteinuria (N = 3). All patients received enalapril for control of proteinuria; other ACE inhibitors or angiotensin receptor blockers were not used.
Lipid profile, cIMT, and FMD at 12-month follow-up
Table 2 shows mean lipid levels during 12-month follow-up. The use of atorvastatin compared to placebo did not significantly change lipid levels over 12 months after adjusting for age, gender, body mass index (BMI), and serum creatinine (GEE, P > 0.1). At 12 months, the LDL-C levels were similar in the two groups [mean difference 21.7 (95% CI − 57.9 to 101.4) mg/dl]. The median percentage change in serum LDL-C between baseline and 12 months was 15.8% and 9.5% in the intervention and placebo arms, respectively, on modified intention-to-treat analysis of 28 patients (P = 0.41, Table 3). Similar change in LDL-C was also found on per-protocol analysis of 23 patients (16.2% versus 9.5% with atorvastatin and placebo respectively, P = 0.30). Serum LDL-C was < 130 mg/dl at 12 months in five patients (35.7%) treated with atorvastatin compared to four patients (28.6%) in the placebo group (P = 0.69). Median percentage change in total cholesterol, triglyceride, VLDL-C, HDL-C, apoA, and hs-CRP was not significantly different in the two groups (Table 3, P > 0.5). There was significant decline in apoB levels in patients treated with atorvastatin compared to placebo (respective median change 19.9% versus 1.1%, P = 0.008). However, this decline was not statistically significant in the per-protocol analysis (17.1% versus 3.9% respectively, P = 0.19).
Since a fixed dose of atorvastatin was used, we also analyzed the effect of weight-based dosing. Mean dose of atorvastatin was 0.39 ± 0.12 mg/kg (range 0.26 to 0.64 mg/kg). There was no significant correlation between change in lipid fractions and per-kg dose (P > 0.1). Change in lipid levels were similar among children with the higher (> 0.39 mg/kg) versus lower doses (< 0.39 mg/kg; P > 0.1).
There was no significant difference in cIMT between patients administered atorvastatin and placebo (P = 0.7 and 0.9 at 6 months and 12 months, respectively; Table 2). Median FMD at 12 months was 10.7 (9.2–16.2) % in patients receiving atorvastatin compared to 13.2 (8.3–15.8) % in those receiving placebo (P = 1.0). Overall, mean cIMT showed a statistically insignificant decline from 0.456 ± 0.06 at baseline to 0.437 ± 0.05 after 12 months in all patients (P = 0.11). Similarly, median FMD at baseline was 11.3 (6.7–18.8) % and 12.2 (8.8–15.9) % at 12 months (P = 1.0). There was no significant association between cIMT or FMD and change in lipid levels or per-kg dose of atorvastatin (data not shown).
Predictors of serum lipid levels
Following 12-month follow-up, median serum albumin and 24-h urine protein levels in atorvastatin and placebo groups were 2.8 (1.9–3.4) g/dl, 2.9 (2–3.9) g/dl, 800 (70–1500) mg, and 595 (165–1375) mg, respectively (P = 0.9 for both). Change in BMI, systolic and diastolic blood pressure SDS, and estimated GFR were similar between the intervention and placebo groups over 12-month follow-up (P > 0.5). On multivariate analysis, change in serum albumin was negatively associated with change in levels of LDL-C, VLDL-C, total cholesterol, triglyceride, and apoB irrespective of receiving atorvastatin and adjusting for age, gender, BMI, and serum creatinine (GEE, P < 0.001); no significant association was obtained with HDL-C and apoA. Change in serum albumin did not vary by histopathological diagnosis (P = 0.32) and association with change in eGFR was not seen (P = 0.60); albumin infusions were not used. Change in proteinuria was not associated with blood lipid levels.
Adverse events
Most common adverse events were infections, comprising upper respiratory tract infection (27 episodes), acute gastroenteritis (6 episodes), and pyoderma (2 episodes) (Table 4). One patient in the placebo group had an episode of pneumonia requiring hospitalization, hence was reported as a serious adverse event and was withdrawn from the study at 3 months. Median creatinine kinase at 12-month follow-up was 96 (58–160.5) IU/l and 108.3 (56.5–153.5) IU/l in the intervention and placebo group respectively (normal 39–308 IU/l). Two patients in the placebo arm had transient asymptomatic elevation of serum CK (380 and 382 IU/l) that spontaneously resolved within 2 weeks. None had CK more than 3-times the upper limit of normal or symptoms suggestive of rhabdomyolysis. Cramps and pain in lower limbs and backache occurred in 9 and 8 patients in the atorvastatin and placebo group, respectively, that was associated with normal CK and resolved without discontinuation of study medication (Table 4). Median levels of aspartate and alanine aminotransferases at 12 months were 21 (19–30) IU/l and 18 (12–24) IU/l respectively, in the atorvastatin group and 22.5 (19.3–35.3) IU/l and 17.5 (15–27.5) IU/l in the placebo group (normal 10–35 IU/l and 10–40 IU/l). One patient in the atorvastatin group had asymptomatic elevation of alanine aminotransferase level more than twice the upper limit of normal (117 IU/l) that declined to normal within 2 weeks.
Discussion
This randomized controlled trial assessed the efficacy of a fixed dose of atorvastatin to decrease hypercholesterolemia in children with refractory nephrotic syndrome. At the end of 12 months, atorvastatin administered at a dose of 10 mg/day was not superior to placebo in reducing plasma LDL-C levels. While atorvastatin significantly decreased serum apoB levels by 20% as compared to 1% with placebo, this result lost statistical significance in the per-protocol analysis. There was no beneficial effect on other lipid fractions (total cholesterol, triglyceride, VLDL-C, HDL-C, and apoA) on cIMT and brachial artery FMD.
There is limited data on the role of statins in treating dyslipidemia associated with refractory nephrotic syndrome (Table 5). Experience in pediatric age group is limited to only two prospective uncontrolled studies demonstrating decline in triglycerides, LDL-C, and total cholesterol by 30–40% in 19 patients over a period of 6–60 months [23, 24]. While we observed that 36% patients had LDL-C levels below 130 mg/dl at 12 months, this was not significantly different from placebo. In adults with nephrotic-range proteinuria, studies demonstrating beneficial effect of statins included clinically heterogeneous population comprising post-renal transplant patients [26], lupus nephritis [26, 27], Alport syndrome [28], interstitial nephritis [28], and idiopathic membranous nephropathy [29], limiting generalizability of these results to children with nephrotic syndrome predominantly due to minimal change disease or focal segmental glomerulosclerosis. Table 5 shows four randomized controlled trials conducted in adults with nephrotic syndrome that were included in a Cochrane systematic review [10, 30,31,32,33]. In this review, concordant to our findings, no significant difference was found in levels of serum LDL-C (mean difference − 5.1 mg/dL, 95% CI − 68.3 to 58.2; n = 40), total cholesterol (mean difference − 53.0 mg/dL, 95% CI − 159.5 to 53.5; n = 92), and triglyceride (mean difference − 38.9 mg/dL, 95% CI − 110.2 to 32.6; n = 40), between statins and control group after 3 months of therapy. However, most results were based on single study data and trials included were at high risk of reporting and selection bias. Other studies in the review showing reduction in levels of triglycerides, total, and LDL-C with statins reported outcomes as median/mean without standard deviation [30, 31] or had methodological flaws [25], limiting their inclusion in the final meta-analysis [10]. We observed a mean difference of 21.7 mg/dl in LDL-C levels between atorvastatin and placebo groups following 12-month therapy that was greater than reported in the Cochrane review; however, this was not statistically significant and confidence intervals were large. While one study demonstrated significant rise in HDL-C with statins (mean difference 5.4 mg/dL, 95% CI 2.3 to 8.5; n = 40) [32], other studies in the review did not show this effect, similar to the present study. We observed significant decline in apoB levels with atorvastatin similar to previous reports showing increased clearance of apoB with statins [25]. We could not explain the pathophysiological mechanism causing decline in apoB levels in the absence of reduction in cholesterol levels. It has been reported that apoB plays an important role in dysfunction of vascular endothelium and is associated with coronary artery calcification [34]. Therefore, our finding of isolated reduction in apoB with atorvastatin requires further evaluation in a larger cohort.
Structural and functional abnormality on vascular imaging in nephrotic syndrome, assessed respectively by ultrasonographic measurement of increased cIMT [22, 35] and reduced FMD of the brachial artery [36], represents one of the earliest stages of atherogenesis. A previous open-label study showed improvement in brachial artery FMD following atorvastatin in 8 out of 10 adults with nephrotic syndrome that was significantly correlated to reduction of non-HDL-C [9]. Paucity of information exists on serial cIMT and FMD measurements in children with renal diseases especially nephrotic syndrome. In a series of 22 post-renal transplant patients, mean cIMT showed a declining trend from 0.46 to 0.43 mm with strict blood pressure control over 9-year follow-up [37]. Similarly, median decline in cIMT by 0.004 mm/year observed in the current study may have been due to dietary modifications and ACE inhibition. In children with chronic kidney disease (CKD), FMD significantly improved from 6.7 to 9.2% with high-dose vitamin D therapy over 12 weeks [38]; patients in the present study had a higher FMD at baseline (11.3%). In another trial, 10 mg/day atorvastatin failed to change FMD (9.8 to 8%) in 8 children with CKD over 8 weeks [39]. No significant improvement in brachial artery FMD in the present study may be explained by insignificant change in lipid levels with statins.
Previous trials have shown a decline in serum lipid fractions with statins paralleling rise in serum albumin in adults with nephrotic syndrome (Table 5). The impact of improvement of albumin on subsequent lipid levels in adults with nephrotic syndrome is well known [40]; this finding has not been explored in refractory nephrotic syndrome in pediatric patients. We observed that rise in serum albumin was significantly associated with decline in serum LDL-C, triglyceride, and total cholesterol levels irrespective of the allocated treatment, age, sex, BMI, and serum creatinine in post hoc analysis; rise in serum albumin was not associated with glomerular filtration rate, histopathological diagnosis, or specific therapy. The molecular link between proteinuria and hypertriglyceridemia has been suggested to be podocyte injury triggered circulating factor angiopoietin-like-4 that inhibits clearance of triglycerides by lipoprotein lipase [41]. Podocyte damage also upregulates serum proprotein convertase subtilisin kexin type 9 (PCSK9) that degrades LDL receptors and results in hyperlipidemia [42]. This state of acquired LDL receptor deficiency may hamper the action of statins, which act by upregulation of LDL receptors [43]. Statins therefore have no effect upon these complex pathophysiological mechanisms linking podocyte damage and hyperlipidemia that may explain the inefficiency of statins to lower cholesterol levels in the present study. As evident from our findings, given the central role of proteinuria and hypoalbuminemia in the pathogenesis of dyslipidemia, the target should be reversal or attenuation of proteinuria and therapeutic intervention should aim at the renal–hepatic axis that regulates plasma cholesterol [6].
Atorvastatin at a dose of 10 mg/day was safe and well tolerated in the present study. Myalgia or lower extremity pain was complained by similar number of patients receiving atorvastatin and placebo; this was not associated with CK elevation. Prior studies have demonstrated long-term tolerability of statin in children older than 8 years with familial hypercholesterolemia [44]. Higher doses of atorvastatin, administered at 20 mg/day, were safe in children older than 10 years [45]. While safety of statins has been extensively examined in adults, there is a concern that when initiated in early childhood, it may adversely affect nervous system, immune function, hormonal milieu, and other systems. Since atorvastatin reduces LDL-C and triglycerides in a dose-dependent manner, an escalating dosing schedule in non-responders could possibly have revealed a beneficial effect in the present trial. However, children younger than 10 years of age constituted a fifth of the present cohort and limited information on the long-term effect of statins on neurological and pubertal development, especially in young children precluded incorporating dose escalation in the present trial design. While we did not observe a significant effect of higher per-kilogram dosing, trend of declining lipid levels among patients administered atorvastatin and the attrition of 23% suggests that the trial may have been under powered rather than atorvastatin being clearly ineffective. Post hoc power was reduced to 68% with the current sample size and effect sizes, suggesting a type II error. It is also possible that treatment effects might have been obscured by the introduction of diet and ACE inhibition in both groups. Despite these limitations, this is the first prospective randomized controlled trial assessing the efficacy of a promising therapy for hyperlipidemia in children with SRNS with a relatively long follow-up. The results of this study are generalizable to children with steroid resistance and major biopsy diagnoses of minimal change, focal segmental glomerulosclerosis, and membranoproliferative glomerulonephritis.
Conclusion
The findings from this study suggest that there is no clear benefit of a fixed dose of atorvastatin on lowering lipid levels in children with unremitting nephrotic syndrome; therapy to raise serum albumin may instead be useful. While it seems logical to treat hyperlipidemia for prevention of accelerated atherosclerosis, there is no proven benefit of statins on overall cardiovascular morbidity and mortality in children [10] and possible side effects are clear limitations for any therapeutic enthusiasm. However, significant gaps in the evidence call for adequately powered studies with longer follow-up and involving higher doses of statins if necessary, to confirm our findings.
References
National Heart, Lung, and Blood Institute (2011) Expert panel on integrated guidelines for cardiovascular health and risk reduction in children and adolescents: summary report. Pediatrics 128(Suppl 5):S213–S256
Querfeld U (1999) Should hyperlipidemia in children with the nephrotic syndrome be treated? Pediatr Nephrol 13:77–84
Kniazewska MH, Obuchowicz AK, Wielkoszynski T, Zmudzinska-Kitczak J, Urban K, Marek M, Witanowska J, Sieron-Stoltny K (2009) Atherosclerosis risk factors in young patients formerly treated for idiopathic nephrotic syndrome. Pediatr Nephrol 24:549–554
Lechner BL, Bockenhauer D, Iragorri S, Kennedy TL, Siegel NJ (2004) The risk of cardiovascular disease in adults who have had childhood nephrotic syndrome. Pediatr Nephrol 19:744–748
Keane WF (1994) Lipids and the kidney. Kidney Int 46:910–920
Vaziri ND (2016) Disorders of lipid metabolism in nephrotic syndrome: mechanisms and consequences. Kidney Int 90:41–52
Kusters DM, Avis HJ, de Groot E, Wijburg FA, Kastelein JJ, Wiegman A, Hutten BA (2014) Ten-year follow-up after initiation of statin therapy in children with familial hypercholesterolemia. JAMA 312:1055–1057
Vuorio A, Kuoppala J, Kovanen PT, Humphries SE, Tonstad S, Wiegman A, Drogari E (2014) Statins for children with familial hypercholesterolemia. Cochrane Database Syst Rev:CD006401
Dogra GK, Watts GF, Herrmann S, Thomas MA, Irish AB (2002) Statin therapy improves brachial artery endothelial function in nephrotic syndrome. Kidney Int 62:550–557
Kong X, Yuan H, Fan J, Li Z, Wu T, Jiang L (2013) Lipid-lowering agents for nephrotic syndrome. Cochrane Database Syst Rev:CD005425
Nishi S, Ubara Y, Utsunomiya Y, Okada K, Obata Y, Kai H, Kiyomoto H, Goto S, Konta T, Sasatomi Y, Sato Y, Nishino T, Tsuruya K, Furuichi K, Hoshino J, Watanabe Y, Kimura K, Matsuo S (2016) Evidence-based clinical practice guidelines for nephrotic syndrome 2014. Clin Exp Nephrol 20:342–370
Gipson DS, Massengill SF, Yao L, Nagaraj S, Smoyer WE, Mahan JD, Wigfall D, Miles P, Powell L, Lin JJ, Trachtman H, Greenbaum LA (2009) Management of childhood onset nephrotic syndrome. Pediatrics 124:747–757
Schwartz GJ, Gauthier B (1985) A simple estimate of glomerular filtration rate in adolescent boys. J Pediatr 106:522–526
Expert Panel on Detection, Evaluation, and Treatment of High Blood Cholesterol in Adults (2001) Executive summary of the third report of the National Cholesterol Education Program (NCEP) expert panel on detection, evaluation, and treatment of high blood cholesterol in adults (adult treatment panel III). JAMA 285:2486–2497
de Onis M, Onyango AW, Borghi E, Siyam A, Nishida C, Siekmann J (2007) Development of a WHO growth reference for school-aged children and adolescents. Bull World Health Organ 85:660–667
National High Blood Pressure Education Program Working Group on High Blood Pressure in Children and Adolescents (2004) The fourth report on the diagnosis, evaluation, and treatment of high blood pressure in children and adolescents. Pediatrics 114:555–576
Wentz PW, Cross RE, Savory J (1976) An integrated approach to lipid profiling: enzymatic determination of cholesterol and triglycerides with a centrifugal analyzer. Clin Chem 22:188–192
Steele BW, Koehler DF, Azar MM, Blaszkowski TP, Kuba K, Dempsey ME (1976) Enzymatic determinations of cholesterol in high-density-lipoprotein fractions prepared by a precipitation technique. Clin Chem 22:98–101
Martin SS, Blaha MJ, Elshazly MB, Toth PP, Kwiterovich PO, Blumenthal RS, Jones SR (2013) Comparison of a novel method vs the Friedewald equation for estimating low-density lipoprotein cholesterol levels from the standard lipid profile. JAMA 310:2061–2068
Touboul PJ, Hennerici MG, Meairs S, Adams H, Amarenco P, Bornstein N, Csiba L, Desvarieux M, Ebrahim S, Hernandez Hernandez R, Jaff M, Kownator S, Naqvi T, Prati P, Rundek T, Sitzer M, Schminke U, Tardif JC, Taylor A, Vicaut E, Woo KS (2012) Mannheim carotid intima-media thickness and plaque consensus (2004–2006–2011). An update on behalf of the advisory board of the 3rd, 4th and 5th watching the risk symposia, at the 13th, 15th and 20th European Stroke Conferences, Mannheim, Germany, 2004, Brussels, Belgium, 2006, and Hamburg, Germany, 2011. Cerebrovasc Dis 34:290–296
Corretti MC, Anderson TJ, Benjamin EJ, Celermajer D, Charbonneau F, Creager MA, Deanfield J, Drexler H, Gerhard-Herman M, Herrington D, Vallance P, Vita J, Vogel R, International Brachial Artery Reactivity Task Force (2002) Guidelines for the ultrasound assessment of endothelial-dependent flow-mediated vasodilation of the brachial artery: a report of the International Brachial Artery Reactivity Task Force. J Am Coll Cardiol 39:257–265
Ksiazek J, Niemirska A, Lipka M, Grenda R (2006) Evaluation of arterial intima-media thickness (IMT) in children with idiopathic nephrotic syndrome--preliminary report. Przegl Lek 63(Suppl 3):205–207
Coleman JE, Watson AR (1996) Hyperlipidaemia, diet and simvastatin therapy in steroid-resistant nephrotic syndrome of childhood. Pediatr Nephrol 10:171–174
Sanjad SA, al-Abbad A, al-Shorafa S (1997) Management of hyperlipidemia in children with refractory nephrotic syndrome: the effect of statin therapy. J Pediatr 130:470–474
Toto RD, Grundy SM, Vega GL (2000) Pravastatin treatment of very low density, intermediate density and low density lipoproteins in hypercholesterolemia and combined hyperlipidemia secondary to the nephrotic syndrome. Am J Nephrol 20:12–17
Golper TA, Illingworth DR, Morris CD, Bennett WM (1989) Lovastatin in the treatment of multifactorial hyperlipidemia associated with proteinuria. Am J Kidney Dis 13:312–320
Rabelink AJ, Hene RJ, Erkelens DW, Joles JA, Koomans HA (1988) Effects of simvastatin and cholestyramine on lipoprotein profile in hyperlipidaemia of nephrotic syndrome. Lancet 2:1335–1338
Thomas ME, Harris KP, Ramaswamy C, Hattersley JM, Wheeler DC, Varghese Z, Williams JD, Walls J, Moorhead JF (1993) Simvastatin therapy for hypercholesterolemic patients with nephrotic syndrome or significant proteinuria. Kidney Int 44:1124–1129
Rayner BL, Byrne MJ, van Zyl SR (1996) A prospective clinical trial comparing the treatment of idiopathic membranous nephropathy and nephrotic syndrome with simvastatin and diet, versus diet alone. Clin Nephrol 46:219–224
Olbricht CJ, Wanner C, Thiery J, Basten A (1999) Simvastatin in nephrotic syndrome. Simvastatin in Nephrotic Syndrome Study Group. Kidney Int Suppl 71:S113–S116
Gheith OA, Sobh MA, Mohamed Kel S, El-Baz MA, El-Husseini F, Gazarin SS, Ahmed HA, Rasem MW, Amer GM (2002) Impact of treatment of dyslipidemia on renal function, fat deposits and scarring in patients with persistent nephrotic syndrome. Nephron 91:612–619
Sharma M, Nand N, Aggarwal HK, Nand D (2004) Evaluation of effects of lovastatin on hypercholesterolaemia and renal functions in nephrotic syndrome. J Indian Acad Clin Med 5:143–146
Gheith O, Sheashaa H, Abdelsalam M, Shoeir Z, Sobh M (2009) Efficacy and safety of Monascus purpureus Went rice in children and young adults with secondary hyperlipidemia: a preliminary report. Eur J Intern Med 20:e57–e61
Yu Q, Zhang Y, Xu CB (2015) Apolipoprotein B, the villain in the drama? Eur J Pharmacol 748:166–169
Hooman N, Isa-Tafreshi R, Otukesh H, Mostafavi SH, Hallaji F (2013) Carotid artery function in children with idiopathic nephrotic syndrome. Nefrologia 33:650–656
Rahul I, Krishnamurthy S, Satheesh S, Biswal N, Bobby Z, Lakshminarayanan S (2015) Brachial artery flow-mediated dilatation and carotid intima medial thickness in pediatric nephrotic syndrome: a cross-sectional case-control study. Clin Exp Nephrol 19:125–132
Balzano R, Lindblad YT, Vavilis G, Jogestrand T, Berg UB, Krmar RT (2011) Use of annual ABPM, and repeated carotid scan and echocardiography to monitor cardiovascular health over nine yr in pediatric and young adult renal transplant recipients. Pediatr Transplant 15:635–641
Aytac MB, Deveci M, Bek K, Kayabey O, Ekinci Z (2016) Effect of cholecalciferol on local arterial stiffness and endothelial dysfunction in children with chronic kidney disease. Pediatr Nephrol 31:267–277
Mackie FE, Rosenberg AR, Harmer JA, Kainer G, Celermajer DS (2010) HMG CoA reductase inhibition and endothelial function in children with chronic kidney disease (CKD)--a pilot study. Acta Paediatr 99:457–459
Appel GB, Blum CB, Chien S, Kunis CL, Appel AS (1985) The hyperlipidemia of the nephrotic syndrome. Relation to plasma albumin concentration, oncotic pressure, and viscosity. N Engl J Med 312:1544–1548
Clement LC, Mace C, Avila-Casado C, Joles JA, Kersten S, Chugh SS (2014) Circulating angiopoietin-like 4 links proteinuria with hypertriglyceridemia in nephrotic syndrome. Nat Med 20:37–46
Haas ME, Levenson AE, Sun X, Liao WH, Rutkowski JM, de Ferranti SD, Schumacher VA, Scherer PE, Salant DJ, Biddinger SB (2016) The role of proprotein convertase subtilisin/kexin type 9 in nephrotic syndrome-associated hypercholesterolemia. Circulation 134:61–72
Prescott WA Jr, Streetman DA, Streetman DS (2004) The potential role of HMG-CoA reductase inhibitors in pediatric nephrotic syndrome. Ann Pharmacother 38:2105–2114
Braamskamp MJ, Kusters DM, Avis HJ, Smets EM, Wijburg FA, Kastelein JJ, Wiegman A, Hutten BA (2015) Long-term statin treatment in children with familial hypercholesterolemia: more insight into tolerability and adherence. Paediatr Drugs 17:159–166
McCrindle BW, Ose L, Marais AD (2003) Efficacy and safety of atorvastatin in children and adolescents with familial hypercholesterolemia or severe hyperlipidemia: a multicenter, randomized, placebo-controlled trial. J Pediatr 143:74–80
Funding
This study was funded by Indian Council for Medical Research.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
This study was conducted from July 2011 to February 2015 at a tertiary care center following approval by the Institute ethics committee and Drug Controller General of India. The trial was registered at the Clinical Trials Registry of India (http://ctri.nic.in; CTRI 2012/07/002761). Informed written consent was obtained from either parent before enrollment.
Conflict of interest
The authors declare that they have no conflict of interest.
Rights and permissions
About this article
Cite this article
Hari, P., Khandelwal, P., Satpathy, A. et al. Effect of atorvastatin on dyslipidemia and carotid intima-media thickness in children with refractory nephrotic syndrome: a randomized controlled trial. Pediatr Nephrol 33, 2299–2309 (2018). https://doi.org/10.1007/s00467-018-4036-x
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00467-018-4036-x