Abstract
Nephrotic syndrome in children is a clinical manifestation of different histopathological subtypes. There is a paucity of recent large studies dealing with the histopathological spectrum from developing countries. A prospective study was performed from January 1990 to December 2000 at our center, involving 600 children (with age of onset up to 16 years) with idiopathic nephrotic syndrome (INS). The objectives were: (1) to study the histopathological distribution of different subtypes of INS and (2) to compare the clinical and biochemical parameters at the time of diagnosis of minimal change disease (MCD) with non-MCD subtypes. For the purpose of this study we analyzed only those children with INS who underwent biopsies. The study group included 290 children in which adequate biopsy reports were available. There were 213 males and 77 females. Mean age at onset of INS was 7.9+5.1 years. Facial edema was found in 286 (98.6%), microhematuria in 120 (41.3%), gross hematuria in 7 (2.5%), and hypertension in 77(26.8%) patients. All patients of the study group were seronegative for HBsAg and HIV. Focal and segmental glomerulosclerosis (FSGS) was the most common histopathological subtype, occurring in 110 of 290 children (38%). Other subtypes included MCD in 95 children (32%), membranoproliferative glomerulonephritis (MPGN) in 44 children (15%), mesangioproliferative glomerulonephritis in 33 children (11%), membranous glomerulonephritis in 5 children (2%), and diffuse mesangial sclerosis in 3 children (1%). In children under 8 years of age, MCD was the most common entity, whereas FSGS predominated in children with age at onset greater than 8 years. The age at onset of nephrotic syndrome was significantly higher in the non-MCD group than the MCD group. The incidence of hypertension, microhematuria, and gross hematuria was significantly lower in the MCD group. MCD remains the most common histopathological subtype in Indian children with INS and onset under 8 years of age. The incidence of MPGN continues to be high. MCD can be differentiated from non-MCD subtype by younger age at onset, absence of hypertension, and absence of microscopic hematuria.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Nephrotic syndrome in children is a clinical manifestation of different histopathological subtypes. Minimal change disease (MCD) remains the most common cause of idiopathic nephrotic syndrome (INS), especially in children under 8 years of age [1]. Few studies have suggested changing trends of histopathology of nephrotic syndrome, with an increasing incidence of focal segmental glomerulosclerosis (FSGS) in both adults as well as children [2, 3, 4]. Reports from developed countries indicate a decreasing incidence of membranoproliferative glomerulonephritis (MPGN) [5], although similar data from developing countries are lacking. There is a paucity of recent large studies dealing with the histopathological spectrum in these countries.
When INS is first diagnosed in a child, a common steroid protocol is usually followed regardless of the underlying histopathology [6]. Although many workers believe that MCD, mesangioproliferative glomerulonephritis (MesPGN), and FSGS represent different ends of the spectrum of the same disease, the long-term prognosis of the non-MCD subtypes is poorer [7]. Hence, it is still important to analyze the clinicopathological spectrum of INS. This also helps us evaluate whether it is possible to predict non-MCD subtypes based on clinical features at the time of presentation. Hence, we prospectively evaluated the histopathological spectrum of children with INS with the following objectives: (1) to study the histopathological distribution of different subtypes of INS and (2) to compare the clinical and biochemical parameters of MCD with non-MCD subtypes.
Patients and methods
A prospective study was performed from January 1990 to December 2000 at our center, involving 600 children (with age at onset up to 16 years) with INS. These patients comprised a homogenous racial group representing the Northern and Eastern Indian populations and proportionately included patients from different socioeconomic groups. Most had been treated earlier by other physicians and referred to our unit for management. Our hospital is the only pediatric nephrology center in the entire state and also serves three other neighboring states, with an approximate population of 300 million. Children with HBsAg seropositivity, HIV seropositivity, and underlying secondary causes of nephrotic syndrome were excluded from the analysis.
At presentation, they were evaluated clinically for hypertension, hematuria, anthropometric parameters (height, weight, and body surface area), and systemic involvement. They were investigated for confirmation of nephrotic syndrome, exclusion of secondary causes, HbsAg, and HIV seropositivity, and renal function. All patients fulfilled the International Study of Kidney Disease in Children (ISKDC) criteria, for the diagnosis of nephrotic syndrome: nephrotic-range proteinuria (urinary spot protein/creatinine >2.0), hypoalbuminemia (serum albumin <2.5 g/dl), hyperlipidemia (serum cholesterol >200 mg/dl), and/or edema [6]. After informed consent, kidney biopsy was performed in the following situations: (1) age at onset younger than 1 year and older than 8 years, (2) no response to 8 weeks of prednisolone therapy, (3) frequent relapser (FR), steroid-dependent (SD), and steroid non-responder (SNR) categories before cytotoxic therapy, and (4) unusual clinical features (hypertension and gross hematuria) and/or laboratory abnormalities (abnormal renal function) [6, 8]. The biopsy specimens were evaluated histopathologically by light and immunofluorescence microscopy. The antibodies used for immunofluorescence were IgG, IgA, IgM, and C3. Histopathological findings were interpreted by the same pathologists, with similar criteria as in our previous study [6]. An adequate biopsy was defined as the presence of at least 5 glomeruli in the specimen on light microscopy [9]. The histopathological diagnosis was made according to standard definitions. MCD was defined histopathologically by the absence of major structural changes [10]. FSGS was diagnosed when at least 1 of the glomeruli was involved, with a process of capillary collapse, obliteration, and sclerosis. A diagnosis of MesPGN was made in the presence of diffuse mesangial hypercellularity lacking immune deposits [11]. MPGN was characterized by diffuse mesangial and cellular proliferation and thickening of capillary walls, with a split or double-contoured appearance [5]. For the purpose of this study we analyzed only those children with INS who underwent biopsies.
Children with MCD, FSGS, and MesPGN subtypes were treated with steroids according to the protocol defined in our earlier study [6]. Based on the number of relapses subsequently, these children were categorized into infrequent relapser, FR, SD, and SNR categories, according to standard guidelines [6]. Cyclophosphamide was administered in FR, SD with steroid side effects, and SNR children, when consent was obtained. Cyclophosphamide was given orally at a dose of 2.5 mg/kg per day for 3 months or in monthly pulses of 500 mg/m2 administered intravenously for 6 months [6, 12]. Children with mesangiocapillary glomerulonephritis were administered steroids according to the ISKDC protocol [13]. Hypertension was defined as systolic or diastolic blood pressure >95th percentile for age, gender, and height on three separate occasions [14]. Microscopic hematuria was defined as the presence of >3 red blood cells per high-power field in a spun urine specimen.
Renal insufficiency was defined as a persistent elevation in serum creatinine level beyond the normal range for the patient's age [15]. The incidence of a subtype was calculated according to total biopsies. Clinical features and biochemical parameters were compared among various subtypes. The results were analyzed for statistical significance using Student′s t-test and chi-squared test by the Microstat statistical analysis software (Ecosoft, USA).
Results
Six hundred children with INS were analyzed during this period. Kidney biopsy was performed in 309 of these children. Of these, 19 children were excluded from the study due to underlying secondary causes, inadequate biopsies where repeat biopsies could not be performed, and loss to follow-up. The study group included 290 children in which adequate biopsy reports were available. There were 213 males and 77 females. Mean age at onset of INS was 7.9+5.1 years. Facial edema was found in 286 (98.6%), microhematuria in 120 (41.3%), gross hematuria in 7 (2.5%), and hypertension in 77 (26.8%) patients. All patients of the study group were seronegative for HBsAg and HIV.
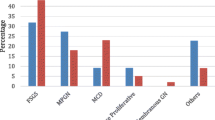
In those children with INS who underwent biopsy, FSGS was the most common histopathological subtype, occurring in 110 of 290 children (38%). Other subtypes included MCD in 95 children (32%), primary MPGN in 44 children (15%), MesPGN in 33 children (11%), membranous glomerulonephritis in 5 children (2%), and diffuse mesangial sclerosis in 3 children (1%). MCD was the most common entity in children under 8 years of age, whereas FSGS predominated in children with age at onset >8 years.
The clinical features of various histopathological subtypes are depicted in Table 1. The mean age at onset of nephrotic syndrome was significantly higher in the non-MCD group than in the MCD group (P<0.001). The incidence of hypertension and microhematuria was significantly (P<0.001) lower in MCD. The mean blood urea nitrogen (BUN) and serum creatinine at presentation were also significantly (P=0.002 and 0.02, respectively) lower in MCD. Total serum protein and albumin levels were similar (P=0.19 and 0.52, respectively) in MCD and non-MCD groups (Table 2).
Discussion
The underlying histopathological characteristics in nephrotic syndrome are of immense significance in determining steroid responsiveness and long-term prognosis [7, 16, 17, 18]. We analyzed the histopathological pattern of INS in our population by evaluating 290 children who selectively underwent biopsy, according to criteria defined earlier [8], and had a homogenous ethnic background.
In children with onset of nephrotic syndrome under 8 years of age, MCD was the most commonly encountered entity in our study. However, FSGS was the most common lesion beyond 8 years, as well as in the entire study group. Recently, FSGS has been reported to be increasing in adults [3, 4]. We have also previously reported an increasing incidence of FSGS in our patient population, although this is stable now [6]. MPGN accounted for 7.5% of all children with INS in the ISKDC study [7]. However, recent studies from Europe, Japan, and the United States indicate a decreasing incidence of MPGN [5, 19]. In an earlier study from India by Srivastava et al. [20], MPGN accounted for 3.5% of children. However, in this study all children with INS were biopsied—a practice no longer followed. This selection bias could influence the observed distribution of histopathological entities. In our study, unlike those from western countries, we observed that the incidence of primary MPGN continues to be high. This could be because, unlike in western countries, environmental factors, such as infection, might not have changed much over the years in India. The incidence of membranous nephropathy was less than that reported previously in children with INS [18]. This might be because electron microscopy was not performed, thus introducing the risk for missing very early (stage I) membranous lesions. In our study MCD was found in 33% of children and MesPGN in 11% of patients. The incidence of MesPGN tends to vary according to geographical area. A lower incidence of MesPGN was reported in the west versus 17.6% of all NS in Saudi Arabia [21].
MCD, FSGS, and MesPGN subtypes constituted the major group in our study population, comprising 83% of the cases. In younger children, MCD still remains the most common histopathological entity, even in children who are biopsied selectively. Patients with steroid-sensitive infrequent nephrotic syndrome were not biopsied. This selection bias might have influenced the frequency of histopathological subtypes. Most clinicians would like to treat MCD, FSGS, and MesPGN with a common steroid protocol. However, it is important to clinically differentiate between MCD and other histological subtypes of INS, as this is of long-term prognostic significance. In our study, the age at onset of nephrotic syndrome was significantly greater in the non-MCD group. Also the incidence of hypertension, microhematuria, and gross hematuria was significantly lower in the MCD subgroup. Thus, the absence of these features may indicate MCD as underlying etiology. The BUN and serum creatinine were also significantly lower in MCD. Total serum protein and albumin was similar in MCD and non-MCD group.
In conclusion, MCD remains the most common histopathological subtype in children with onset of nephrotic syndrome under 8 years of age. The incidence of MPGN continues to be high in Indian children. MCD can be differentiated from the non-MCD group by younger age at onset of nephrotic syndrome, and a lower incidence of hypertension and microscopic hematuria.
References
Mallick NP (1991) Epidemiology and natural course of idiopathic nephrotic syndrome. Clin Nephrol 35:S3–S7
Haas M, Spargo BH, Coventry S (1995) Increasing incidence of focal segmental glomerulosclerosis among adult nephropathies: a 20 year renal biopsy study. Am J Kidney Dis 26:740–750
Bonilla-Felix M, Parra C, Ferris M, Swinford RD, Brannan P, Portman RJ (1997) Focal segmental glomerular sclerosis (FSGS) in children with idiopathic nephrotic syndrome (NS) is the incidence increasing. J Am Soc Nephrol 8:82A
Gulati S, Sharma AP, Sharma RK, Gupta A (1999) Changing trends of histopathology in childhood nephrotic syndrome. Am J Kidney Dis 34:646–650
Iitaka K, Saka T, Yagisawa K, Aoki Y (2000) Decreasing hypocomplementemia and membranoproliferative glomerulonephritis in Japan. Pediatr Nephrol 14:794–796
Gulati S, Kher V, Sharma RK, Gupta A (1994) Steroid response pattern in Indian children with nephrotic syndrome. Acta Pediatr Scand 83:530–533
International Study of Kidney Disease in Children (1977) Ten years of activity: a report for the International Study of Kidney Disease in Children. In: Batsford SR (ed) Glomerulonephritis. Wiley, New York, pp 201–209
Broyer M, Meyrier A, Niaudet P, Habib R (1998) Minimal change and focal segmental glomerulosclerosis. In: Davison AM, Cameron JS, Grunfeld JP, Kerr DNS, Ritz E, Winerals CS (eds) Oxford textbook of clinical nephrology. Oxford University Press, Oxford, pp 493–535
Oberholzer M, Torhorst J, Perret E, Mihatsch MJ (1983) Minimum sample size of kidney biopsies for semi-quantitative and quantitative evaluation. Nephron 34:192–195
Churg J, Habib R, White RH (1970) Pathology of nephrotic syndrome in children: a report for the ISKDC. Lancet I:1299–1302
The Southwest Pediatric Nephrology Study Group (1983) Childhood nephrotic syndrome associated with diffuse mesangial hypercellularity. Kidney Int 23:87–89
Elhence R, Gulati S, Kher V, Gupta A, Sharma RK (1994) IV pulse cyclophosphamide—a new regime for steroid-resistant minimal change nephrotic syndrome. Pediatr Nephrol 8:1–3
Tarshish P, Bernstein J, Tobin JN, Edelmann CM (1992) Treatment of mesangiocapillary glomerulonephritis with alternate-day prednisone—a report of the International Study of Kidney Disease in children. Pediatr Nephrol 6:123–130
(1996) Update on the 1987 task force report on high blood pressure in children and adolescents: a working group report from the National High Blood Pressure Education Program. Pediatrics 98:649–658
Schwartz GJ, Haycock GB, Spitzer A (1976) Plasma creatinine and urea concentration in children: normal values for age and sex. J Pediatr 88:828–830
International Society of Kidney Disease in Children (1978) Nephrotic syndrome in children: prediction of histopathology from clinical and laboratory characteristics at time of diagnosis. Kidney Int 13:159–165
International Society of Kidney Disease in Children (1981) The primary nephrotic syndrome in children: identification of patients with minimal change nephrotic syndrome from initial response to prednisone. J Pediatr 98:561–564
White RH, Glasgow EF, Mills RJ (1970) Clinicopathological study of nephrotic syndrome in childhood. Lancet I:1353–1359
Simon P, Ramee MP, Ang KS, Cam G (1987) Variations of primary GN incidence in a rural area of 400,000 inhabitants in the last decade. Nephron 45:171
Srivastava RN, Mayekar G, Anand R, Chaudhary VP, Ghai OP, Tandon HD (1975) Nephrotic syndrome in Indian children. Arch Dis Child 50:626–630
Abdurrahman MB, Elidrissy AT, Shipkey FH, Al Rasheed S, Al Mugeiren M (1990) Clinicopathological features of childhood nephrotic syndrome in Saudi Arabia. Ann Trop Pediatr 10:125–132
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Kumar, J., Gulati, S., Sharma, A.P. et al. Histopathological spectrum of childhood nephrotic syndrome in Indian children. Pediatr Nephrol 18, 657–660 (2003). https://doi.org/10.1007/s00467-003-1154-9
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00467-003-1154-9