Abstract.
To investigate the incidence of acute pyelonephritis (APN) and renal scarring in children with febrile urinary tract infection (UTI), 191 of 216 (88%) children with their first episode of UTI received 99mTc-dimercaptosuccinic acid renal single-photon emission computed tomography. They were investigated within 7 days of admission and were followed for 6 months. One hundred and six patients (49.1%) underwent a voiding cystourethrogram. The incidence of vesicoureteric reflux (VUR) in group I (≤1 year old) was 22%, group II (1–5 years old) 69%, and group III (5–17 years old) 44%. The overall incidence of APN in febrile UTI was 70% (male 66%, female 76%, P=0.110). Children had a higher incidence of APN than infants (P<0.05 in group I vs. II and group I vs. III). Of patients with APN, 57% (35/61) showed renal scar formation. VUR was found in 31%(24/78) of children with APN and 58% (14/24) of children with renal scar. In addition, children with high-grade VUR were more susceptible to APN and scar formation than those with low-grade VUR (P<0.05). Older children with a first febrile UTI had a higher incidence of APN than infants (≤1 year), and half of the children with APN developed a renal scar.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Urinary tract infection (UTI) is a common disorder in the pediatric population and especially in infants [1]. Clinical features of acute pyelonephritis (APN) or upper UTI include fever, flank pain, pyuria, and a positive urine culture. However, the signs and symptoms of upper UTI are often nonspecific and misleading in pediatric patients, especially in neonates and infants. Technetium 99m-dimercaptosuccinic acid scintigraphy (DMSA) is a noninvasive imaging modality that has high sensitivity and specificity to detect renal inflammation. The application of single-photon emission computed tomography (SPECT) further enhances the sensitivity of DMSA in the detection of APN to 96% [2, 3, 4, 5, 6]. The renal damage from the initial insult of APN leads to the subsequent development of an irreversible renal scar in 50%–65% of affected children [2, 6]. However, Benador et al. [7] reported that the incidence of renal scar can be as high as 86% in children between 1 and 5 years of age. Renal scarring with repetitive infection can result in hypertension, chronic renal failure, and end-stage renal disease [8, 9, 10, 11]. However, the incidence of APN and renal scarring associated with pediatric UTI cannot be reliably determined by clinical parameters. The aim of our study was to investigate, using DMSA renal SPECT, the incidence of APN and sequelae of renal scarring in children with their first febrile UTI and to correlate the presence of vesicoureteric reflux (VUR) with APN and renal scarring.
Patients and methods
From November 1996 to December 1999, a total of 314 children were admitted to our medical center with the diagnosis of febrile UTI. Two hundred and sixteen children, 132 boys and 84 girls (age range 1–176 months, mean 23±2.4 months) were enrolled in this study. The age distribution in group I was 3.8±2.4 months, median 3 months, group II 34.8±15.6 months, median 30 months, and group III 94.3±27.1 months, median 88.5 months. Diagnostic criteria included fever with a core temperature of 38°C or higher and positive urine culture. The definition of a positive urine culture was either growth of microorganisms over 105 colony-forming units/ml from clean-voided midstream urine in older children, or over 103 colony-forming units/ml from suprapubic puncture in younger children. Renal ultrasonography was performed in each patient to exclude any abnormal renal contour. Patients with genitourinary abnormalities, except VUR, and a history of recurrent UTI were excluded. Parental consent was obtained before the study and the study was approved by the Human Ethics Committee of our hospital.
Empiric parenteral antibiotic treatment with cephalothin (Ulothin, U Liang Chemical and Pharmaceutical, Taoyuan, Taiwan) and gentamicin (Yung Shin Pharmaceutical Industrial, Taichung, Taiwan) were prescribed for all patients for at least 3 days, and then adjusted according to a bacterial susceptibility test for a total of around 10–14 days. Parenteral antibiotics were changed to the oral form after the patient was afebrile. To ensure cure of the primary UTI, at least one negative urine culture was required after a total treatment course. Outpatient clinic follow-up was arranged regularly for these patients, and urinalyses and urine cultures were performed monthly.
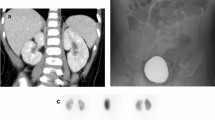
Initial DMSA renal SPECT was performed within 1 week of admission. The second DMSA renal SPECT was performed at 6 months after acute infection for all but 1 patient, who received a DMSA renal SPECT at 4 months. For DMSA renal SPECT imaging, each subject was injected intravenously with 2.5 MBq/kg of body weight (minimal dose 20 MBq) of 99mTc DMSA. Imaging was initiated approximately 2–3 h later. We used a triple-headed rotating gamma camera (Multispect3, Siemens Medical Systems, Hoffman Estates, Ill., USA) with high-resolution collimators. The SPECT data were acquired over a circular 360° rotation, 120 steps, and 35 s per step in a 128×128×16 matrix. Reconstruction was performed with filtered back projection by using a Butterworth filter (cut-off frequency 0.55 of the Nyquist frequency, power factor 7) with attenuation correction according to the Chang method [12]. Any photopenic area in the renal cortex was considered abnormal.
The radionuclide scans were used as the gold standard for the diagnosis of APN. Two experienced nuclear medicine physicians unaware of the patients′ clinical presentations visually assessed the SPECT images independently to make their diagnosis. In general, DMSA changes persisting beyond 3 months are likely to be due to permanent scarring rather than APN [13]. The scan was considered to reflect an acute inflammation process when at least one area of decreased focal or diffuse cortical uptake of DMSA was noted, with the renal outline preserved. If one or more areas of focal renal cortical defect were consistently associated with defects in the renal outline, i.e., little or no DMSA uptake and loss of volume in the previous involved cortex, a renal scar was diagnosed [14].
Voiding cystourethrograms (VCUG) were investigated after acute inflammation subsided, about 2–4 weeks later. Briefly, an 8-Fr feeding tube was inserted into the bladder through the urethra, the catheter was taped to the leg, and then a film of the abdomen was taken to make sure the catheter was in the bladder. The tube in the bladder was then connected to a bottle of a special contrast material that was dripped by gravity until the bladder was filled. Then a series of images were taken to find any liquid that had gone backwards to one or both ureters when the patient emptied his or her bladder. After the patient had voided completely, a final image was taken to determine how well the bladder had emptied. However, indications to perform VCUG were not influenced by the results of renal ultrasonography. The results were evaluated for the presence and grades of VUR according to the international grading system [15]. For the purposes of comparison between grading of VUR and association of APN or renal scar, grades I and II were grouped together as low-grade VUR and grade III-V as high-grade VUR. If patients had bilateral VUR, they were grouped according to the side of higher grade.
To analyze the incidence of APN, renal scar, and VUR in different ages, the subjects were divided into three age groups: group I ≤1 year old, group II 1–5 years old, and group III 5–15 years old.
Results are expressed as mean±SD. Clinical parameters of sex, age groups, DMSA results, and VCUG grading were analyzed with a chi-squared test. Fisher exact tests were applied for cases with insufficient expected cell frequencies. Statistical significance was set at P<0.05. All statistical analyses were performed using a commercial software program (StatView 5.01, Abacus Concepts, Berkeley, Calif., USA).
Results
The first febrile UTI occurred more frequently in male infants (<1 year old) than in females ≥1 year old (Table 1). One hundred and ninety-one (88%) patients received DMSA renal SPECT and 133 patients were diagnosed with APN [group I 63% (82/131), group II 86% (25/29), group III 84% (26/31)]. During the acute phase of UTI, APN was found in a significantly higher proportion of children >1 year old than in infants (group I vs. II and group I vs. III, P<0.05). The proportion with APN did not differ significantly between group II and group III (Table 1), but there were significant differences in the incidence of UTI or APN between the sexes (Tables 1 and 2, all P<0.001). Overall, the incidence of APN in first febrile UTI was 70% (male 66%, female 76%, P=0.110).
During the follow-up period, 61 of 133 (46%) patients with APN received a DMSA renal SPECT examination after an average of 10 months (4–28 months, median 9 months) and 35 (57%) patients showed scar formation. Although group II had a higher incidence of renal scar (79%), there were no significant differences between these three groups (Table 2).
One hundred and six patients with first febrile UTI underwent VCUG investigation and 35 (33%) patients had VUR (group I 22%, group II 69%, group III 44%). The group II children had a significantly higher incidence of VUR than patients <1 year old (group I) (P<0.05). Overall, the differences in incidence of low-grade VUR and high-grade VUR during first febrile UTI were not significant between these three age groups (Table 1).
Of 133 patients with APN, 78 underwent VCUG, 24 (31%) of whom showed VUR. Group II children also had a higher incidence of VUR than group I (P<0.001). A comparison of the grading of VUR and APN in different age groups showed a significant relationship between high-grade VUR and APN, but no relationship between low-grade VUR and APN (Table 2).
In total, 35 patients developed renal scars, and of these, 24 (69%) underwent a VCUG and 14 (58%) had VUR (Table 3). The frequency of high-grade VUR was significantly higher in patients who developed renal scars than low-grade VUR (P<0.05). Furthermore, we found no significant difference in the frequency of APN or renal scar formation between the low-grade VUR group and the group without VUR (Table 4). There were 6 patients with bilateral VUR; 5 of the 6 patients with bilateral VUR had bilateral scarring. One patient showed bilateral VUR with a right side grade of 3 and a left side grade of 2, with a renal scar on the right side.
Discussion
It has been estimated that approximately 1% of boys and 3% of girls will experience a symptomatic UTI before the 11th year of life [16, 17]. The prevalence of UTI in boys is higher in the first 3 months of life [18]. Our study showed that both febrile UTI and APN were more prevalent in males under 1 year and females over 1 year.
In our study, more than 60% (group I 63%, group II 86%, and group III 84%) of first febrile UTI involved the kidney, and the incidence of APN, higher in the older age group, was nearly the same as that reported by Benador et al. [6]. The incidence of APN in infants (63%) was similar to that in previous studies [7, 19]. Several studies [20, 21] have reported that the susceptibility of the renal parenchyma to infection varies with age, with those under 1 year at greatest risk. However, our study revealed that APN was more common in older children. We suppose this might be due to the different criteria for admission in infants and older children. Renal scarring after APN was equally prevalent in the three age groups (Table 2). We believe that the severity of the inflammatory process and the volume of kidney involved are the major contributing factors for renal scar formation, independent of age [22]. This means that both the host immunological defense and microbiological virulence factors are critical co-factors for renal scarring [23].
Although VUR was predominant in group II, the number of patients was too small to draw any conclusion. Nevertheless, our results showed that the prevalence of VUR did not decline with age in children with febrile UTI. Although, high-grade VUR allows migration of bacteria into the parenchyma, APN and renal scarring still could occur in the absence of reflux. In the present study, the frequency of APN without VUR was 69% and that of renal scarring without VUR was 42%. Biggi et al. [24] also reported that severe renal infection can result even in the absence of VUR. In our study, 57% (35/61) of children with APN produced irreversible lesions of the renal parenchyma, irrespective of VUR. The relationship between the extent of kidney inflammation in the acute phase and the late outcome in the presence or absence of VUR is still unexplored. We hypothesize that VUR is one of the multiple risk factors in APN and renal scar formation, others being host susceptibility, urinary tract obstruction, inflammatory response, and therapeutic delay.
The present study also shows that high-grade VUR has greater correlation with APN and renal scar formation than low-grade VUR. This suggests that we might prescribe prophylactic antibiotics for selected patients with high-grade VUR.
In conclusion, there is a 70% incidence of APN in children with first febrile UTI, and nearly half develop a renal scar. However, most of those with renal scarring showed a small unifocal area on the DMSA scan. The long-term clinical significance of these unifocal areas of renal scarring is, as yet, unknown. The scars, however, can alert pediatricians and allow the prevention of repeated UTI. We need to monitor the long-term renal sequelae of these patients, because further study of the long-term renal sequelae associated with renal scarring may reduce the size of the risk group.
Finally, the incidence of febrile UTI or APN was higher in males than females under the age of 1 year, and the reverse was true thereafter. Since VUR was present in a third of our patients with APN, half of whom showed scar formation, other risk factors should be evaluated in infants with APN and renal scar formation.
References
Hoberman A, Chao HP, Keller DM, Hickey R, Davis HW, Ellis D (1993) Prevalence of urinary tract infection in febrile infants. J Pediatr 123:17–23
Jakobsson B, Soderlundh S, Berg U (1992) Diagnostic significance of 99mTc-dimercaptosuccinic acid (DMSA) scintigraphy in urinary tract infection. Arch Dis Child 67:1338–1342
Jakobsson B, Nolstedt L, Svensson L, Soderlundh S, Berg U (1992) 99mTechnetium-dimercaptosuccinic acid scan in the diagnosis of acute pyelonephritis in children: relation to clinical and radiological findings. Pediatr Nephrol 6:328–334
Rushton HG, Majd M, Chandra R, Yim D (1988) Evaluation of 99mtechnetium-dimercapto-succinic acid renal scans in experimental acute pyelonephritis in piglets. J Urol 140:1169–1174
Majd M, Rushton HG, Chandra R, Andrich MP, Tardif CP, Rashti F (1996) Technetium-99m-DMSA renal cortical scintigraphy to detect experimental acute pyelonephritis in piglets: comparison of planar (pinhole) and SPECT imaging. J Nucl Med 37:1731–1734
Benador D, Benador N, Slosman DO, Nussle D, Mermillod B, Girardin E (1994) Cortical scintigraphy in the evaluation of renal parenchymal changes in children with pyelonephritis. J Pediatr 124:17–20
Benador D, Benador N, Slosman D, Mermillod B, Girardin E (1997) Are younger children at highest risk of renal sequelae after pyelonephritis? Lancet 349:17–19
Wallace DM, Rothwell DL, Williams DI (1978) The long-term follow-up of surgically treated vesicoureteric reflux. Br J Urol 50:479–484
Jacobson SH, Eklof O, Eriksson CG, Lins LE, Tidgren B, Winberg J (1989) Development of hypertension and uraemia after pyelonephritis in childhood: 27 year follow up. BMJ 299:703–706
Jacobson SH, Eklof O, Lins LE, Wikstad I, Winberg J (1992) Long-term prognosis of post-infectious renal scarring in relation to radiological findings in childhood--a 27-year follow-up. Pediatr Nephrol 6:19–24
Goonasekera CD, Shah V, Wade AM, Barratt TM, Dillon MJ (1996) 15-year follow-up of renin and blood pressure in reflux nephropathy. Lancet 347:640–643
Chang L (1978) A method for attenuation correction in radionuclide computed tomography. IEEE Trans Nucl Sci 25:683–643
Jakobsson B, Svensson L (1997) Transient pyelonephritic changes on 99mTechnetium-dimercaptosuccinic acid scan for at least five months after infection. Acta Paediatr 86:803–807
Goldraich NP, Ramos OL, Goldraich IH (1989) Urography versus DMSA scan in children with vesicoureteric reflux. Pediatr Nephrol 3:1–5
Lebowitz RL, Olbing H, Parkkulainen KV, Smellie JM, Tamminen-Mobius TE (1985) International system of radiographic grading of vesicoureteric reflux. International Reflux Study in Children. Pediatr Radiol 15:105–109
Winberg J, Andersen H, Bergstrom T, Jacobsson B, Larson H, Lincoln K (1974) Epidemiology of symptomatic urinary tract infection in childhood. Acta Pediatr Scand [Suppl] 252:1–20
Jodal U (1987) The natural history of bacteriuria in childhood. Infect Dis Clin North Am 1:713–729
Stull TL, LiPuma JJ (1991) Epidemiology and natural history of urinary tract infections in children. Med Clin North Am 75:287–297
Goldraich NP, Goldraich IH (1995) Update on dimercaptosuccinic acid renal scanning in children with urinary tract infection. Pediatr Nephrol 9:221–226
Martinell J, Claesson I, Lidin-Janson G, Jodal U (1995) Urinary infection, reflux and renal scarring in females continuously followed for 13–38 years. Pediatr Nephrol 9:131–136
Gleeson FV, Gordon I (1991) Imaging in urinary tract infection. Arch Dis Child 66:1282–1283
Chiou YY, Wang ST, Tang MJ, Lee BF, Chiu NT (2001) Renal fibrosis: prediction from acute pyelonephritis focus volume measured at99mTc dimercaptosuccinic acid SPECT. Radiology 221:366–370
Smellie JM, Edwards D, Normand IC, Prescod N (1981) Effect of vesicoureteric reflux on renal growth in children with urinary tract infection. Arch Dis Child 56:593–600
Biggi A, Dardanelli L, Cussino P, Pomero G, Noello C, Sernia O, Spada A, Camuzzini G (2001) Prognostic value of the acute DMSA scan in children with first urinary tract infection. Pediatr Nephrol 16:800–804
Acknowledgements.
This study was supported in part by grants from the National Science Council of the Republic of China (NSC 89–2314-B-006–028) and the Scientific Funds of the National Cheng Kung University Medical Center (no. 033, 2000).
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Lin, KY., Chiu, NT., Chen, MJ. et al. Acute pyelonephritis and sequelae of renal scar in pediatric first febrile urinary tract infection. Pediatr Nephrol 18, 362–365 (2003). https://doi.org/10.1007/s00467-003-1109-1
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00467-003-1109-1