Abstract
Background
Cumulative musculoskeletal stress during operative procedures can contribute to the development of chronic musculoskeletal injury among surgeons. This is a concern in laparoscopic specialties where trainees may incur greater risk by learning poor operative posture or technique early in training. This study conducted an initial investigation of the physical stress encountered during the conduct of foregut laparoscopic surgery.
Methods
Subjects were divided into two groups based on their surgical experience level, high experience (HE), consisting of two attending surgeons, and low experience (LE), consisting of two fellow surgeons and a surgical chief resident. Nine distinct foregut laparoscopic procedures were observed for data collection within these groups. Electromyographic (EMG) activity was collected at the bilateral neck, shoulders, biceps, triceps, and lower back for each procedure. Physical workload was measured using percent reference voluntary contractions (%RVC) for each surgeon’s muscle activities. Fatigue development was assessed using the median frequency of EMG data between two consecutive cases. Subjects completed a NASA-TLX survey when surgery concluded.
Results
LE surgeons experienced higher levels of %RVC in the lower back muscles compared to HE surgeons. LE fatigue level was also higher than HE surgeons across most muscle groups. A decrease in median frequency in six of the ten muscle groups after performing two consecutive cases, the largest decrements being in the biceps and triceps indicated fatigue development across consecutive cases for both surgeon groups.
Conclusion
Surgeons developed fatigue in consecutive cases while performing minimally invasive surgery (MIS). HE surgeons demonstrated a lower overall physical workload while also demonstrating different patterns in muscle work. The findings from this study can be used to inform further ergonomic studies and the data from this study can be used to develop surgical training programs focused on the importance of surgeon ergonomics and minimizing occupational injury risk.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Minimally invasive surgery (MIS) provides a significant advantage over traditional open approaches in terms of surgical outcomes and accelerated patient recovery [1]. However, the influence of the laparoscopic approach on surgeons’ physical workload during MIS procedures is one area where there is a paucity of data that might better inform occupational health considerations in this population. The typical body posture for surgeons performing MIS procedures is standing upright, focused on a monitor with arms abducted outward for extended periods while holding and operating the laparoscopic instruments [2]. There is also a component of rotational workload as the surgeon reaches to return or receive instruments from the scrub technician or nurse during the procedure. Posture during laparoscopic operations is much more static when compared to open operations, which limits natural posture changes and can contribute to an increase in workload. Laparoscopic tasks generally also require more time and effort to perform [3,4,5].
A number of laparoscopists have reported pain, stiffness, and fatigue as a result of performing multiple MIS procedures [6]. Other studies have confirmed that surgeons are at risk for developing work-related musculoskeletal symptoms due to specific operative postures that are associated with MIS [7, 8]. What is more alarming is the report that 87% of surgeons who perform MIS regularly admit to some degree of occupational injury [9]. In another survey of 300 surgeons, the neck and lower back were reported to be the most prevalent painful body sites [10]. Muscles that were cited as needing treatment as a result of MIS workload in a survey of 1400 surgeons were the shoulders, lower back, neck, and upper back [11]. The neck and back muscles, in particular, have been reported to be a source of pain in multiple surveys [8, 10, 12]. In studies utilizing surface EMG electrodes to monitor muscle activity and fatigue, MIS was found to be more strenuous when compared to robotic-assisted surgery [12, 13].
The operative workload of surgeons is a significant factor in the development of musculoskeletal issues. The average general surgeon performs about 500 procedures annually [14]. Unsurprisingly, more procedures performed correlates to increased reports of musculoskeletal symptoms [9, 11, 15, 16]. Proficient surgeons also have heavy workloads, as experienced general surgeon faculty can also spend up to 70 hours each week providing clinical care [17].
There is a correlation between the length of surgery and fatigue development for MIS in addition to the higher physical load required for MIS, which also puts surgeons at risk for developing fatigue [12, 18,19,20]. Unsurprisingly, increased physical loading results in greater strain on muscles [6, 19, 21]. Previous studies have found mixed results in equating surgeon operative experience with the development of fatigue. One study in a simulated surgical environment determined that surgeons with more experience do have slightly reduced fatigue development [19], while a similar study found that the experience level of the surgeon did not have any effect on fatigue development whatsoever [18]. More recently, a study utilizing surface EMG sensors to measure muscle fatigue found a trend of increased fatigue when a surgeon performed a more advanced role (being primary surgeon versus assisting surgeon) [20].
It has been challenging for researchers to objectively evaluate the physical workload of surgeons during actual MIS procedures. In most studies, surgeon physical load and fatigue were mainly assessed using subjective approaches, such as self-reporting surveys, observations from live surgeries, or simulated surgeries [5, 6, 8, 10, 11, 18, 22]. Unfortunately, these studies can only provide subjective ratings which may not reflect the true level of physical workload. Likewise, the value of self-reported surveys are often limited in an environment that discourages complaints about stress or fatigue [21]. Observational studies may not accurately detect muscle fatigue that is often not visible. Some studies have investigated surgeons' physical workload utilizing objective measurements [12, 13, 20, 23]. However most of these studies were performed in simulated environments and the effect of surgeons’ experience level on the physical workload of surgeons was not considered.
In order to address these limitations, the aim of our study was to investigate the objective physical workload experienced by surgeons during live laparoscopic procedures. Further, we sought to explore the effect of the surgeons' experience level on their physical workload and fatigue development.
Materials and methods
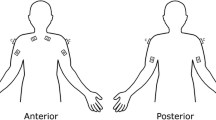
After approval of the experiment protocol by the IRB at Oregon Health and Science University (OHSU), five surgeons were recruited from the Foregut Unit at OHSU for the study. This group was evaluated over the course of nine MIS procedures. The high experience (HE) group consisted of two academic laparoscopic foregut surgeons with over 30 combined years of advanced laparoscopic practice. The low experience group (LE) consisted of two MIS fellows (9 months of advanced laparoscopic experience) and a surgical chief resident (no advanced laparoscopic experience). The independent variables for this study were surgeon experience level (high vs. low) and surgery order (1st vs. 2nd). The dependent variable was the physical workloads experienced across ten different muscle groups. Figure 1 shows these groups to include the right and left posterior neck and shoulders (superior and inferior descending trapezius), biceps, triceps, and lower back muscles (latissimus dorsi). Physical workload was measured as the percentage of reference voluntary contractions (%RVC) and median frequency (MF) (Hz). Higher %RVC indicated a higher physical workload because it is a comparison with the subject’s baseline muscle activity doing moderate muscle movements. Higher physical workloads were also indicated by decreasing MF. A final MF that was lower than the initial MF was indicative of fatigue development due to muscle fatigue over time. The immediate fatigue development was measured by the decrement of MF across two consecutive surgeries. Consecutive surgeries were defined as the same procedure performed immediately after the first on a different patients with no break in between.
Consent was obtained from every subject before their participation. Prior to surgery, wireless electromyography (EMG) sensors (Delsys Trigno, Delsys Inc, Natick, MA, USA) were attached to the ten selected muscle groups. Baseline muscle activity values were taken over a 10 second period for each muscle group. For the neck muscles, the subject was instructed to stand against the wall with their hands put behind their head and to push their head backward as much as they could. For the shoulder muscles, the subject was seated with 90° shoulder abduction and holding a 5 lb. weight on the hand of the target side. For the biceps, the subject was seated with their elbows flexed at 90° holding a 5 lb. weight in the hand of the target side. For the triceps, the subject was seated with 45° shoulder extension angle and holding a 5 lb. weight in the hand of the target side. For the low back muscles, the subject was instructed to hold a 5 lb. weight in each hand while bending their trunk forward with straight knees and back and keeping the wrists at the knee level and looking forward.
After the RVC collection the surgeon performed a MIS procedure. All surgeons performed gastric bypasses acting as primary surgeons for the duration of the surgery. During surgery, the activities of the ten muscle groups were collected for ten seconds every 10 minutes throughout the length of the procedure using the EMG sensors. The length of the procedure was defined to be from incision to removal of the laparoscopic ports. Immediately after completing the procedure, each subject was asked to complete a NASA-TLX (Task Load Index) survey. This survey asks a respondent to subjectively rate their perceived mental and physical workload after completion of a specific task [24].
Surgeon experience as related to muscle activity was determined using mean normalized %RVC. For each muscle, the average reading of a surgeon was taken as a percent of the RVC data collected prior to surgery. These values were then averaged with surgeons of the same experience level to obtain the overall %RVC. To compare the physical workload between two surgeon experience levels, the means of the %RVC and the MF were compared for each of the ten muscle groups of the two experience levels. To explore the fatigue development of each muscle group among the two experience levels, the means of the MF for two consecutive surgeries on a single day were calculated.
The raw EMG data was analyzed using Delsys software. The root mean squared and mean MF of each 10 second EMG data recording was calculated out. Microsoft Excel 2013 (Microsoft Corporation, Redmond, WA, USA) was used to organize and calculate out the descriptive statistics of the EMG and NASA-TLX data. Due to the small sample size, no statistical analysis was performed. Only descriptive statistics of the dependent variables were calculated.
Results
Four female and one male surgeon were recruited. Demographics data of the subjects are shown in Table 1.
Nine surgeries were observed in total. For all observed cases, the subjects all performed as the primary surgeon. The average surgery length of all nine cases was 77 ± 30.5 min. The average surgery length of the two surgeon groups, HE and LE, were 60 ± 19 min and 90 ± 33 min, respectively. To avoid distractions introduced by EMG sensors, EMG data was not collected during the case which was performed by the chief resident. Therefore, muscle activities measurements, %RVC and MF, were collected from eight out of nine observed surgeries.
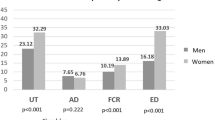
The %RVC of the HE group was slightly higher than that of the LE group across the majority of muscle groups (Fig. 2). However, the %RVC in the lower back areas of the LE surgeons were much higher than that of the HE surgeons (96% vs. 38% on the right and 208% vs. 49% on the left, respectively).
Across eight observed surgeries, MF in all observed muscle groups was higher in the HE surgeon group as compared to the LE group except for the right and left triceps (Fig. 3). The largest decrements were 19.2 Hz and 14.3 Hz and 10.9 Hz in the left back and right and left biceps, respectively.
Only two subjects performed consecutive cases, one HE surgeon and one LE surgeon. Therefore, only the trend of the fatigue development could be investigated in this study. A trend of decreasing MF was found in six of the ten muscle groups (Fig. 4). The biggest decrement was 5.3 Hz in the left bicep. A trend toward increasing MF was found in the right neck, left shoulder, and right and left back with the biggest increment being 16.0 Hz in the right back.
Table 2 outlines the NASA-TLX ratings for all nine surgeons after completion of their procedures. LE surgeons reported higher mental and temporal demands, as well as higher effort and frustration compared to HE surgeons. The biggest difference was present in frustration (59.5 vs. 23.8, respectively).
Discussion
LE surgeons exhibited significantly greater %RVC in the lower back muscles compared to the HE surgeons, indicating a greater physical workload for LE surgeons. HE surgeons also had higher MF than LE surgeons, indicating that LE surgeons experienced greater fatigue. Comparing MF between two consecutive cases, surgeons overall experienced decrements in six out of ten muscle groups, with the greatest decrements in the bicep and tricep muscles. HE surgeons reported lower workload scores in most individual categories, with the largest differences between LE scores in frustration and temporal workload.
Our results suggest that between two experience levels, muscle activation was higher in LE surgeons and body parts were used differently between HE and LE surgeons. LE surgeons had significantly higher %RVC in the lower back muscles (Fig. 2). HE surgeons had greater %RVC compared to LE surgeons for the remaining muscle groups, but not to a significant extent compared to the differences in back muscle %RVC. This is consistent with our expectation that LE surgeons will experience higher %RVC compared to HE surgeons. In previous studies, surgeons with less experience were found to have higher levels of muscle activity when compared to surgeons with greater experience [16, 19, 20]. Muscle use variation between amateurs and professionals likely occurs because having more experience increases how efficiently muscles are used while completing a task. Therefore, the greater muscle activity of LE surgeons is likely due to their lower experience level [25, 26].
Considering the fatigue difference between two surgeon groups, HE surgeons had higher MF than LE surgeons for all but two muscle groups in overall MF comparisons (Fig. 3). This agrees with the expectation that HE surgeons would experience less muscle fatigue overall when compared to LE surgeons. A previous study in a simulated surgical environment indicated that higher experience level correlated to a slight decrease in fatigue development [19]. When coupled with the trend that HE surgeons have lower levels of muscle use, a lower level of fatigue development is to be expected.
In terms of the fatigue development across two consecutive cases, both surgeon groups experienced MF decrements in the right and left sides of biceps and triceps, right shoulder, and left neck muscles groups between the first and second surgery (Fig. 4). This is consistent with previous findings that while performing surgical techniques EMG MF decreases over time [12, 18]. The greatest decrements were experienced in both right and left biceps and tricep muscle groups. This may indicate that the biceps and triceps are the muscle groups that are more vulnerable to fatigue development while performing MIS. This is consistent with previous studies in simulated surgical environments have found that the arm muscles are at greatest risk for fatigue during laparoscopic surgery [27, 28].
Studies performed in live surgical environments found results contrary to this, often finding that the back, shoulder, and neck muscles were most prone to fatigue development in MIS [12, 13, 20, 23].These differences might be due to small sample size, subject pool, and type of surgery and duration of observation. Many of the previous studies had differing subject pools of either mostly male or all male subjects, whereas our subject pool of individuals was solely female from which EMG measurements were taken. Additionally, the type and duration of MIS differed between studies as well, which may reflect only the conditions of those particular procedures and their length instead of the effect of all MIS.
HE surgeons reported lower levels of NASA-TLX mental, temporal, effort, and frustration compared to LE surgeons but had greater physical demand. This is consistent with our expectation that HE surgeons would experience lower workload levels. In previous studies in simulated surgical environments, HE surgeons performing laparoscopic techniques also reported lower NASA-TLX workloads [28, 29]. One study found HE surgeons reported lower frustration and temporal demands, but approximately equal or greater physical demands compared to LE surgeons [28]. These findings are consistent with ours. The greater physical demand reported by the HE surgeons may be associated with the overall greater age of the HE surgeons in comparison to the LE surgeons. Long-term practice in the OR can cause cumulative damage to a surgeon. When coupled with a body that is overall aging the physical demands of surgery, although unchanged, are more difficult for the surgeon to perform as before [30]. Additionally, the higher performance workload of HE surgeons may be due to the structure of an academic surgeon’s practice. Because academic HE surgeons supervise many individuals when compared to LE surgeons the greater pressure to perform well is not surprising.
The limitation of our study is the small sample size, as only two surgeons (one HE and one LE) were observed for consecutive case fatigue development and eight cases total being observed for overall MF and %RVC. As a result, only basic data analysis was performed on the collected data. No statistic conclusions can be drawn from the results of our comparisons. However, several trends have been identified and the findings from this study can provide new knowledge of surgeons’ workload associated with live surgeries which can serve as a basis for further research regarding surgeon experience and fatigue development and it seems reasonable to offer the following preliminary conclusions.
Conclusion
Surgeons who regularly perform laparoscopic surgery are at risk of developing musculoskeletal disorders or injuries. How surgeon experience level and performing consecutive surgeries affect fatigue development has not been extensively investigated before in live surgical environments. Our findings suggest that, between high experience and low experience surgeons, low experience surgeons have greater muscle use and fatigue development while performing MIS. The muscles most at risk for developing fatigue, regardless of experience level, are arm muscles, specifically the biceps and triceps.
Change history
27 September 2022
A Correction to this paper has been published: https://doi.org/10.1007/s00464-022-09619-7
References
Kane RL et al (1995) The outcomes of elective laparoscopic and open cholecystectomies. J Am Coll Surg 180(2):136–145
Szeto G et al (2010) A study of surgeons’ postural muscle activity during open, laparoscopic, and endovascular surgery. Surg Endosc 24(7):1712–1721
Nguyen NT et al (2001) An ergonomic evaluation of surgeons’ axial skeletal and upper extremity movements during laparoscopic and open surgery. Am J Surg 182(6):720–724
Berguer R, Chen J, Smith WD (2003) A comparison of the physical effort required for laparoscopic and open surgical techniques. Arch Surg 138(9):967–970
Aitchison LP et al (2016) The ergonomics of laparoscopic surgery: a quantitative study of the time and motion of laparoscopic surgeons in live surgical environments. Surg Endosc 30(11):5068–5076
Stomberg MW et al (2010) Work-related musculoskeletal disorders when performing laparoscopic surgery. Surg Laparosc Endosc Percutan Techn 20(1):49–53
Szeto GP et al (2009) Work-related musculoskeletal symptoms in surgeons. J Occup Rehabil 19(2):175–184
Yang L et al (2020) Impact of procedure type, case duration, and adjunctive equipment on surgeon intraoperative musculoskeletal discomfort. J Am Coll Surg 230(4):554–560
Park A et al (2010) Patients benefit while surgeons suffer: an impending epidemic. J Am Coll Surg 210(3):306–313
Dalager T et al (2019) Surgery is physically demanding and associated with multisite musculoskeletal pain: a cross-sectional study. J Surg Res 240:30–39
Plerhoples TA, Hernandez-Boussard T, Wren SM (2012) The aching surgeon: a survey of physical discomfort and symptoms following open, laparoscopic, and robotic surgery. J Robot Surg 6(1):65–72
Dalager T et al (2020) Surgeons’ posture and muscle strain during laparoscopic and robotic surgery. Br J Surg 107(6):756–766
Dalsgaard T et al (2020) Robotic surgery is less physically demanding than laparoscopic surgery: paired cross sectional study. Ann Surg 271(1):106–113
Valentine RJ et al (2011) General surgery workloads and practice patterns in the United States, 2007 to 2009: a 10-year update from the American Board of Surgery. Ann Surg 254(3):520–526
Franasiak J et al (2012) Physical strain and urgent need for ergonomic training among gynecologic oncologists who perform minimally invasive surgery. Gynecol Oncol 126(3):437–442
McDonald ME et al (2014) Physician pain and discomfort during minimally invasive gynecologic cancer surgery. Gynecol Oncol 134(2):243–247
Winslow ER, Bowman MC, Klingensmith ME (2004) Surgeon workhours in the era of limited resident workhours. J Am Coll Surg 198(1):111–117
Slack P et al (2008) The effect of operating time on surgeons’ muscular fatigue. Ann R Coll Surg Engl 90(8):651–657
Uhrich M et al (2002) Assessment of fatigue, monitor placement, and surgical experience during simulated laparoscopic surgery. Surg Endosc 16(4):635–639
Gonzalez-Sanchez M et al (2017) Comparison of fatigue accumulated during and after prolonged robotic and laparoscopic surgical methods: a cross-sectional study. Surg Endosc 31(3):1119–1135
Berguer R (1999) Surgery and ergonomics. Arch Surg 134(9):1011–1016
Wauben L et al (2006) Application of ergonomic guidelines during minimally invasive surgery: a questionnaire survey of 284 surgeons. Surg Endosc 20(8):1268–1274
Armijo PR et al (2019) Ergonomics of minimally invasive surgery: an analysis of muscle effort and fatigue in the operating room between laparoscopic and robotic surgery. Surg Endosc 33(7):2323–2331
Hart SG (2006) NASA-task load index (NASA-TLX); 20 years later. In: Proceedings of the human factors and ergonomics society annual meeting. Sage Publications, Los Angeles, CA
Hemal A, Srinivas M, Charles A (2001) Ergonomic problems associated with laparoscopy. J Endourol 15(5):499–503
Winges SA, Furuya S (2015) Distinct digit kinematics by professional and amateur pianists. Neuroscience 284:643–652
Berguer R, Remler M, Beckley D (1997) Laparoscopic instruments cause increased forearm fatigue: a subjective and objective comparison of open and laparoscopic techniques. Minim Invasive Ther Allied Technol 6(1):36–40
Lee GI et al (2014) Comparative assessment of physical and cognitive ergonomics associated with robotic and traditional laparoscopic surgeries. Surg Endosc 28(2):456–465
Stefanidis D et al (2007) Construct and face validity and task workload for laparoscopic camera navigation: virtual reality versus videotrainer systems at the SAGES Learning Center. Surg Endosc 21(7):1158–1164
Liberman A, Shrier I, Gordon P (2005) Injuries sustained by colorectal surgeons performing colonoscopy. Surg Endosc 19(12):1606–1609
Funding
N/A.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Disclosures
The authors Tegan Thurston, James P. Dolan, Farah Husain, Andrea Stroud, Kenneth Funk, Charlie Borzy, and Xinhui Zhu have no conflicts of interest to disclose.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
This article was corrected to fix the spelling of Farah Husain's name.
Rights and permissions
Springer Nature or its licensor holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Thurston, T., Dolan, J.P., Husain, F. et al. Assessment of muscle activity and fatigue during laparoscopic surgery. Surg Endosc 36, 6672–6678 (2022). https://doi.org/10.1007/s00464-021-08937-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00464-021-08937-6