Abstract
Background
Women surgeons may experience more ergonomic challenges while performing surgery. We aimed to assess ergonomics between men and women surgeons.
Methods
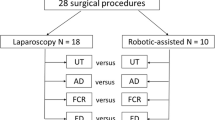
Laparoscopic surgeons from a single institution were enrolled. Demographics and intraoperative data were collected. Muscle groups were evaluated objectively using surface electromyography (EMG; TrignoTM, Delsys, Inc., Natick, MA), and comprised upper trapezius (UT), anterior deltoid, flexor carpi radialis (FCR), and extensor digitorum (ED). Comparisons were made between women (W) and men (M) for each muscle group, assessing maximal voluntary contraction (MVC) and median frequency (MDF). The Piper Fatigue Scale-12 (PFS-12) was used to assess self-perceived fatigue. Statistical analyses were performed using SPSS v26.0, α = 0.05.
Results
18 surgeries were recorded (W:8, M:10). Women had higher activation of UT (32% vs 23%, p < 0.001), FCR (33% vs 16%, p < 0.001), and ED (13% vs 10%, p < 0.001), and increased effort of ED (90.4 ± 18.13 Hz vs 99.1 ± 17.82 Hz). Comparisons were made between W and M for each muscle group, assessing MVC and MDF.
Conclusions
After controlling for surgeon’s height and duration of surgery, an increase in muscle activation was seen for women laparoscopic surgeons. Since poor ergonomics could be a major cause of work-related injuries, we must understand differences in ergonomics between men and women and evaluate which factors impact these variations.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Surgeons across all specialties are faced with a high risk of debilitating musculoskeletal injury as a direct result of operating. Musculoskeletal injury is associated with the tasks unique to each medical profession, and has been described in specialties including urology, dermatology and gynecological surgery [1,2,3]. Ergonomic challenges resulting in injury have been described according to surgical approach. Nevertheless, all approaches (open, laparoscopic, and robotic) have high rates of work-related musculoskeletal disorders and injury [4,5,6]. Prevalence rates of musculoskeletal disorders associated with surgical careers range between 23 and 87%, depending on surgical specialty and approach [2]. This is suggestive of a highly prevalent, yet understudied problem among surgeons. The subsequent discomfort associated with ergonomic difficulties can lead to pain, suffering, loss of surgical ability, and even worsen patient outcomes if uncorrected [5, 7].
Majority of research groups have explored ergonomics within a single specialty. In urology, for example, studies have investigated whether different approaches may offer a solution to musculoskeletal injury [3]. Other studies have investigated level of training as it relates to ergonomics, calling for an emphasis on ergonomics studies within surgical residency [8]. Little research has been done to investigate factors unique to the workforce itself, such as ergonomics impact by gender. One study investigated laparoscopic surgeons for gender differences in ergonomics using a 23-item web-based survey [9]. The authors found that women surgeons experience more discomfort and receive more treatment for hand and wrist pain compared to their men counterparts [9].
There is a body of anecdotal evidence lacking objective measurements addressing the issue of gender differences in the operating room. Given that women now make up over 50% of admitted students in medical school, it is far past time to ensure that barriers, such as additional ergonomic challenges in the operating room, are not hindering their advancement or belonging in the surgical field [10]. Thus, we aimed to determine how self-perceived fatigue and objectively measured muscle activation and effort of the upper limb differ between men and women surgeons performing laparoscopic surgeries.
Material and methods
Study design
Surgeons performing laparoscopic procedures at a single institution from June/2017 to August/2017 were enrolled. At the time of the study, there were 77 surgeons and 20 gynecologists associated with the university. Only surgeons who were currently performing laparoscopic procedure and those who were past their learning curve for laparoscopic procedures (more than 100 cases performed) were selected. Procedures performed by surgical residents and procedures that were converted to another surgical approach were excluded. Surgeons with current musculoskeletal disorders of the upper limb were also excluded from the study. Surgical fields included general surgery, transplant, colorectal, obstetrics and gynecology, and urology. Data were collected on surgeon’s age and height, gender, hand dominance, specialty, years of practicing after residency, presence of musculoskeletal disorders in the upper limb, and average of case performed per month. Intraoperative data included type of surgical approach and operative time. This prospective study was approved by our Institutional Review Board and written consent was obtained for all participants.
Self-perceived fatigue
Surgeons replied to the validated Piper Fatigue Scale-12 (PFS-12) at the beginning and at the end of each surgical procedure [5]. This survey allows for the measurement of self-perceived fatigue and comprises five spheres: behavioral, affective, sensory, cognitive, and overall self-perceived fatigue. A higher score in PFS-12 is representative of increased self-perceived fatigue.
Muscle effort and activation
Objective muscle activation was assessed using the Trigno wireless surface electromyography (EMG; Delsys, Inc., Natick, MA, USA). The detailed protocol for the EMG technique was followed and described in our previous work [5]. Surface EMG sensors were affixed over the surgeon’s dominant upper limb during surgery. Data were collected on the following muscles: upper trapezius (UT), anterior deltoid (AD), flexor carpi radialis (FCR), and extensor digitorum (ED). Resting EMG and maximal voluntary contraction (MVC) were recorded before surgical scrub. These data were normalized to reduce inter-subject variability, and data were presented as a percentage of MVC (%MVC). Median frequency (MDF) was also used for the assessment of muscle fatigue during static force exertion. A higher %MVC is an indicator of higher muscle activation, whereas a lower MDF is an indicator of increased muscle effort [5]. Surgeons’ muscle effort and activation were evaluated while surgeons performed subtasks equivalent across surgeries: dissection, retraction, and suturing.
Statistical analysis
Surgeons were grouped according to their gender, women (W) and men (M), and comparisons were made between these two groups, controlling for the surgeon’s height. Self-perceived fatigue was compared before and after the surgical procedure within and between groups. However, %MVC and MDF were compared between groups. Each surgery was then divided into four quartiles, according to operative room time, and comparisons were made to evaluate fatigue levels over time (Q4 minus Q1), to control for duration of surgery. Data were presented as frequencies for categorical data and mean ± standard deviation or median for the continuous data, according to normality. Pearson chi-square tests and repeated measures analysis of variance were used where appropriate. Statistical analyses were done using SPSS v26.0, with α = 0.05.
Results
18 surgeries were recorded (W: 8, M: 10). All surgeons were right-handed, and no surgeon reported current injury. Mean age (W: 41 ± 6.2 years, M: 39 ± 6.2 years; p = 0.763) and mean height (W: 170 ± 9.5 cm, M: 163 ± 11.9 cm; p = 0.361) were similar between groups. Likewise, no differences were seen for mean cases performed per month (W: 20 ± 11.9, M: 28 ± 10.4; p = 0.29) and mean years of practice (W: 6 ± 4.1 years, M: 5 ± 3.9 years; p = 0.543). The distribution of the surgeries recorded in this study was the following: five bariatric surgeries (W: N = 2, M: N = 3), six foregut-related procedures (W: N = 2, M: N = 4), four hernia repairs (W: N = 2, M: N = 2), two gynecological surgeries (W: N = 2), one hepatectomy (M: N = 1), and one kidney transplant (W: N = 1). Median operating room time was similar between W (204.5 [210–263] min) and M (204.5 [182.8–250] min), p = 0.600. There were no intraoperative complications during the surgical procedures included in this study.
Self-perceived sensory (p = 0.026) and cognitive (p = 0.045) fatigue scores were higher among women surgeons at the end of the surgery, while no differences were seen in the M group (Table 1). Overall, no differences were seen between M and W groups for all four subscales evaluated with PFS-12.
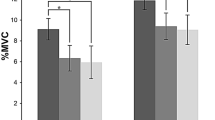
After controlling for surgeon’s height, EMG analysis performed for all subtasks combined revealed a statistically significant increase in %MVC for women surgeons in three muscle groups: UT (32% vs 23%, p < 0.001), FCR (33% vs 16%, p < 0.001), and ED (13% vs 10%, p < 0.001), when compared to men (Fig. 1). Likewise, women had increased muscle effort in ED (W: 90.4 ± 18.13 Hz, M: 99.1 ± 17.82 Hz). Nonetheless, male surgeons had increased muscle effort in UT (W: 63.5 ± 8.29 Hz, M: 60.2 ± 10.43 Hz). Subsequently, analyses controlled for surgery duration revealed similar findings, with muscle activation levels over time being higher in the W group for UT and ED, both p < 0.001 (Fig. 2). Conversely, no differences in muscle activation or effort were seen within each surgeon’s group over time, all p > 0.05.
Discussion
This study found that women surgeons had increased muscle activation of the upper limb and reported higher fatigue levels while performing laparoscopic surgery when compared to their male counterparts. The main difference seen was on the increased muscle activation of shoulder and wrist muscle groups in the women group. Additionally, women reported higher rates of self-perceived fatigue after performing laparoscopic procedures, specifically for the components of cognitive and sensory fatigue. Men surgeons, on the other hand, reported no significant difference in self-perceived fatigue at the end of surgical procedure.
The transition to laparoscopic surgery is associated with numerous benefits to patients including reduced perioperative morbidity, enhanced postoperative recovery, earlier return to work, and cosmetic advantages [5, 11]. An often underappreciated cost of this approach, however, is injury and disability for surgeons resulting from poor ergonomics [5]. A systematic review of 16 articles found a 24% prevalence of musculoskeletal injuries among plastic surgeons, with the cervical spine being the most affected site [12]. An online survey study of 127 surgeons revealed that 44% of the cohort suffered from musculoskeletal disorders, while nearly a third of the respondents requiring medical leave due to this issue [13]. Another survey of 104 plastic surgeons demonstrated that over half of respondents had neck injury, followed by 32% who reported back injuries. Interestingly, only 22% reported having any type of ergonomic training during their career [14]. Our previous work indicated that performing laparoscopic procedures results in higher activation of the upper trapezius and extensor of the wrists of surgeons, which could lead to long-term musculoskeletal injuries [5].
Despite the accumulated knowledge for work-related injuries of laparoscopic surgeons, especially when assessing only one surgical specialty, few studies have objectively evaluated the relationship between gender and ergonomics in the operating room. Especially considering that several studies evaluated plastic surgeons, which might not be the best representation of laparoscopic surgeons. Numerous studies have established that women surgeons experience these consequences at a higher rate than their men counterparts [9, 11, 15]. However, the vast majority of existing literature is based on self-reported responses to nonstandardized survey questions with results being significantly impacted by nonresponse bias [9, 15, 16]. Our study sought to investigate objective differences in ergonomics between men and women surgeons performing laparoscopic procedures.
A survey of nearly 300 laparoscopic surgeons found that a higher case volume was associated with increased reported symptoms of neck and upper and lower extremities. In addition, women reported increased symptoms in the upper extremities, whereas men in the lower [11]. In the current study, both men and women had similar average of cases performed per month, and we did find that women had higher activation of muscle groups in the upper limb. Additionally, surgeons did not report the same level of subjective fatigue when compared to their objective muscle activation. Another survey of 314 laparoscopic surgeons, still, although glove size was found to be significantly correlated with reported issues of the upper limb of laparoscopic surgeons, these studies did not evaluate among studies as a factor.
Given that nearly 60% might be only slightly or not aware of the recommendations made by the field of surgical ergonomics [11], it is critical to not only provide objective data on the effect of ergonomics for informed decisions, but also to disseminate and implement policies that address those issues.
A recent web-based survey study conducted by Sutton et al. found that a similar percentage of men and women surgeons attributed physical discomfort to the laparoscopic approach. Compared to men wearing the same glove size, however, women are more likely to receive treatment for their hands (21 vs 3%, p = 0.016) and experience more neck, shoulder, and upper back discomfort (77 vs. 27%, p = 0.004). [9] After controlling for the surgeon’s height and duration of surgery, we also found women surgeons performing laparoscopic procedures to have an overall increase in upper limb muscle activation, as measured by significantly higher %MVC.
Another large survey study by Berguer et al. eliciting 726 responses from members of professional surgical societies found that 87% of women surgeons can be expected to experience significant difficulty using laparoscopic instruments based on hand size alone [15]. Smaller-handed surgeons experience more difficulties using laparoscopic instruments since grip spans that are too large will decrease the maximum grip force during use [17]. Given that women’s median glove size is significantly smaller than men’s (6.5 vs 7.5, p < 0.001), [18] the higher rates of muscle activation measured in our women group was expected in this study. Specifically, we found women surgeons to have significantly increased use of upper trapezius, flexor carpi radialis, and extensor digitorum muscles compared to men (UT: 32.29 vs 23.12; FCR: 13.89 vs 10.19; ED: 33.03 vs 16.18; all p < 0.001). These findings corroborate with our previous publication stating that both UT and ED had the highest muscle activation in surgeons performing laparoscopic procedures. One hypothesis for the difference observed in ergonomics between gender is related to laparoscopic staplers and scissors, which are reported to cause the most difficulty for smaller-handed and women surgeons [15]. Hence, redesign of laparoscopic instrument handles and adjustment of surgical table heights offer the most promising solutions to these ergonomic challenges [9].
Regarding self-perceived fatigue, women surgeons reported increased cognitive and sensory fatigue compared to men peers at the end of surgical procedures in the current study (p = 0.045 and p = 0.026, respectively). Cognitive fatigue correlates to a feeling of patience, ability to concentrate, and to think clearly; however, sensory fatigue relates to the degree that the surgeon is feeling strong/weak, awake/sleepy, and refreshed/tired [5]. Our results indicate that women surgeons perceived a higher level of mental workload at the end of the surgery, whereas men surgeons did not. This is associated with the surface EMG objective measurements that showed increased muscle activation and poor ergonomics in the women group [5, 19].
Our small sample size is a notable limitation of this study. Given that we only recorded the first surgical case of the day, we are not able to assess the difference in fatigue levels after a full operative day. Additionally, we only evaluated the muscles of the upper limb and do not have information related to muscle groups of the back or lower extremities which also contribute to physical discomfort. We also did not include information regarding table height, use of steps, training level of the surgeon’s assistant, nor patient waist circumference, which could have impacted the evaluation of surgeon’s ergonomics in this study. Surgeon’s glove size was also not collected. Still, we were able to standardize the data analysis across all surgical procedures, including only common surgical subtasks, and considering the time of surgery. In fact, sub-analyses were performed between men and women for each surgical task, and similar results were found to the overall analyses. Therefore, we reported the overall analysis in the manuscript. Additionally, this is the first study that evaluated objectively measurements in the operating room between women and men surgeons performing laparoscopic surgeries across six surgical specialties. As we collect more data, sub-analysis of glove size, handgrip, and % body fat between men and women, as well as the difference in instrumentation could also be studied [5].
Conclusion
While there has been significant interest in this field over the last several years, most of the research has been limited to survey studies which elicit concern regarding several types of bias such as undercoverage, response, nonresponse, and voluntary response bias. Objective data captured using surface EMG can be used to measure muscle effort and activation to better assess the long-term impact of work-related musculoskeletal injuries among surgeons. After controlling for the surgeon’s height and duration of surgery, our data revealed an overall increase in shoulder and wrist muscle activation for women performing laparoscopic procedures. Women reported increased self-perceived sensory and cognitive fatigue at the end of the surgical procedure, while men did not. Results from this study could inform the creation of recommendations to improve ergonomics for women and men surgeons. Further studies are needed to evaluate which factors affect these variations in ergonomics between men and women surgeons and to assess the long-term impact of muscle activation in work-related injuries. Long-term selective use of these different muscle sets may be correlated with different patterns of injury.
References
Catanzarite T, Tan-Kim J, Menefee SA (2018) Ergonomics in gynecologic surgery. Curr Opin Obstet Gynecol 30(6):432–440
Catanzarite T, Tan-Kim J, Whitcomb EL, Menefee S (2018) Ergonomics in surgery: a review. Female Pelvic Med Reconstr Surg 24(1):1–12
Lloyd GL, Chung ASJ, Steinberg S, Sawyer M, Williams DH, Overbey D (2019) Is your career hurting you? The ergonomic consequences of surgery in 701 urologists worldwide. J Endourol 33(12):1037–1042
van Det MJ, Meijerink WJ, Hoff C, Totte ER, Pierie JP (2009) Optimal ergonomics for laparoscopic surgery in minimally invasive surgery suites: a review and guidelines. Surg Endosc 23(6):1279–1285
Armijo PR, Huang CK, High R, Leon M, Siu KC, Oleynikov D (2019) Ergonomics of minimally invasive surgery: an analysis of muscle effort and fatigue in the operating room between laparoscopic and robotic surgery. Surg Endosc 33(7):2323–2331
Kokosis G, Dellon LA, Lidsky ME, Hollenbeck ST, Lee BT, Coon D (2019) Prevalence of musculoskeletal symptoms and ergonomics among plastic surgery residents: results of a national survey and analysis of contributing factors. Ann Plast Surg. 85:310–315
Dianat I, Bazazan A, Souraki Azad MA, Salimi SS (2018) Work-related physical, psychosocial and individual factors associated with musculoskeletal symptoms among surgeons: implications for ergonomic interventions. Appl Ergon 67:115–124
Perez-Duarte FJ, Sanchez-Margallo FM, Diaz-Guemes Martin-Portugues I, Sanchez-Hurtado MA, Lucas-Hernandez M, Uson GJ (2012) Ergonomics in laparoscopic surgery and its importance in surgical training. Cir Esp 90(5):284–291
Sutton E, Irvin M, Zeigler C, Lee G, Park A (2014) The ergonomics of women in surgery. Surg Endosc 28(4):1051–1055
Heiser S (2018) Women were majority of US medical school applicants in 2018. AAMCNews, The Association of American Medical Colleges, Washington, D.C.
Park A, Lee G, Seagull FJ, Meenaghan N, Dexter D (2010) Patients benefit while surgeons suffer: an impending epidemic. J Am Coll Surg 210(3):306–313
Epstein S, Tran B, Capone A, Ruan Q et al (2018) Work-related musculoskeletal disorders among plastic surgeons: a systematic review. J Reconstr Microsurg 34:553–562
Janki S, Mulder EEAP, IJzermans JNM, Tran TCK (2017) Ergonomics in the operating room. Surg Endosc 31:2457–2466
Kokosis G, Dellon LA, Lidsky ME, Hollenbeck ST, Lee BT, Coon D (2019) Prevalence of musculoskeletal symptoms and ergonomics among plastic surgery residents: results of a national survey and analysis of contributing factors. Ann Plast Sur 85:310–315
Berguer R, Hreljac A (2004) The relationship between hand size and difficulty using surgical instruments: a survey of 726 laparoscopic surgeons. Surg Endosc 18(3):508–512
Shepherd JM, Harilingam MR, Hamade A (2016) Ergonomics in laparoscopic surgery—a survey of symptoms and contributing factors. Surg Laparosc Endosc Percutan Tech 26(1):72–77
Blackwell JR, Kornatz KW, Heath EM (1999) Effect of grip span on maximal grip force and fatigue of flexor digitorum superficialis. Appl Ergon 30(5):401–405
Adams DM, Fenton SJ, Schirmer BD, Mahvi DM, Horvath K, Nichol P (2008) One size does not fit all: current disposable laparoscopic devices do not fit the needs of female laparoscopic surgeons. Surg Endosc 22(10):2310–2313
González-Sánchez M, González-Poveda I, Mera-Velasco S, Cuesta-Vargas AI (2017) Comparison of fatigue accumulated during and after prolonged robotic and laparoscopic surgical methods: a cross-sectional study. Surg Endosc 31(3):1119–1135
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Disclosures
Dr. Dmitry Oleynikov is the stockholder for Virtual Incision Corporation, nonrelated to the current work. Dr. Rodrigues Armijo, Ms. Laura Flores, Dr. Bhavani Pokala, Dr. Chun-Kai Huang, and Dr. Joseph Siu have nothing to disclose.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Armijo, P.R., Flores, L., Pokala, B. et al. Gender equity in ergonomics: does muscle effort in laparoscopic surgery differ between men and women?. Surg Endosc 36, 396–401 (2022). https://doi.org/10.1007/s00464-021-08295-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00464-021-08295-3