Abstract
Introduction
Postoperative pancreatic fistula (POPF) following distal pancreatectomy (DP) remains the most frequent complication, potential precursor of more serious events, and mechanisms behind POPF development are not clear. Primary aim of the current study is to investigate correlations between patients’ characteristics, including technical intraoperative data assessed by retrospective video review of laparoscopic DP (L-PD), and development of clinically relevant (CR-)POPF and major complication.
Methods
Patients undergoing L-DP whose surgery video was available for review were included in this study. Retrospective video review, performed by two surgeons blinded for postoperative outcomes, was focused on pancreatic neck transection and identification of pancreatic capsule disruption (PCD)/staple line bleeding (SLB). Correlation between clinical, demographic, and intraoperative factors and CR-POPF/major complications and assessment of factors associated with PCD and SLB were investigated.
Results
Of 41 L-DP performed at our institution (June 2015–June 2020) using a triple-row stapler (EndoGIA™ Reloads with Tri-Staple™), surgery video was available for 38 patients [men/women, 13/25; median age (range) 62 (25–84) years; median BMI (range) 24 (17–42)]. PCD and SLB occurred in 15(39%) and 19(50%) patients and were concomitant in 9(24%). CR-POPF and major complications occurred in 8(21%) and 12(31%) patients, respectively. PCD, SLB, and PCD + SLB rates were significantly higher among patients with CR-POPF, compared to patients without (all p < 0.05). Among patients with PCD, pancreatic thickness at pancreatic transection site was higher (19 mm), compared to non-PCD patients (13 mm, p < 0.001). A directly proportional relation between PCD, CR-POPF, and major complication rate and pancreatic thickness was confirmed by ROC analysis (AUC = 0.949, 0.798, and 0.740, respectively).
Conclusion
PCD and SLB close to the staple line detected by retrospective video-review are intraoperatively detectable indicators of severe pancreatic traumatism and a potential precursors of CR-POPF following L-PD. Given the strict correlation between PCD and pancreatic thickness, alternative techniques to stapled closure for pancreatic transection may be recommended for patients with a thick pancreas and modification in postoperative care may be considered in patients with PCD/SLB.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Despite improvements in surgical and perioperative management, the incidence of postoperative pancreatic fistula (POPF) remains high [1,2,3,4] and clinically relevant (CR-)POPF still represents the main catalyst for the development of additional complications, like intra-abdominal collection, PPH, delayed gastric emptying, with consequent increased length of postoperative hospital stay, increased rates of readmission following discharge, reoperation, and mortality, while negatively affecting the possibility and the time to return to postoperative intended oncologic treatment. While reliable predictors of CR-POPF have been identified and used to build a valid risk score for patients undergoing pancreatoduodenectomy [1], for distal pancreatectomy (DP) studies investigating risk factors for POPF are limited mainly because of the more rare indication for DP, compared to pancreatoduodenectomy. Results from the largest available study on outcomes following DP confirmed the actual difficulty in identifying CR-POPF prognosticators [5], however, the understanding of mechanisms behind CR-POPF development following DP is of utmost importance because it may contribute to the identification and the better care of patients more at risk for this complication.
This study aims at identifying, among patients undergoing laparoscopic DP (L-DP) with stapled pancreatic transection, factors associated with postoperative outcomes, and benefitting from the availability of videos of surgeries (since 2017 all L-PD performed at our Institution are recorded), at investigating intraoperative factors that may predict CR-POPF and major postoperative complications, with a particular focus on the phase of pancreatic transection and stump closure.
Material and methods
Patients selection
A retrospective investigation of the prospectively maintained pancreatic resection database of the Department of General Surgery of Istituto Ospedaliero Fondazione Poliambulanza identified 241 patients who underwent pancreatic resection from June 2015 until June 2020. Following exclusion of 152 patients who underwent a whipple procedure (n = 105) or a total pancreatectomy (n = 39) or a pancreatic enucleation (n = 3) or other pancreatic resections (n = 5), 89 patients undergoing a DP were identified.
At our Institution, a laparoscopic approach is always attempted for patients undergoing a DP, except in case of anesthetic contraindication. Though patients affected by a tumor with vascular infiltration and requiring vascular resection and reconstruction were initially operated with an open approach, with increasing experience we do not consider such situation an absolute contraindication to the laparoscopic approach anymore [6, 7]. After exclusion of patients operated on with an open approach (n = 29) or for whom a conversion from laparoscopy to open was needed [for intraoperative bleeding (n = 2), for technical impossibility to proceed laparoscopically due to treitz invasion (n = 1), and for adhesions due to previous surgery (n = 3)], 54 patients who underwent a L-DP were identified. Following exclusion of patients for whom video of operation was not available (n = 12) or prefiring parenchymal compression before pancreatic stapler transection was not performed (n = 3) or no stapled parenchymal transection was performed (n = 1), remaining 38 patients finally represented the study population [Radical Antegrade Modular Pancreatosplenectomy (RAMPS, n = 13), distal pancreatosplenectomy (DPS, n = 18), and spleen preserving distal pancreatectomy (SPDP, n = 7)] (Fig. 1). Approval by the local ethical committee was obtained for this study.
Patient data collection
Preoperative, intraoperative, pathological and postoperative data of study patients were extracted from our institutional database and investigated. In particular, demographic data included patient age, sex, and body mass index (BMI), clinical data included the presence or not of comorbidities, the ASA score, previous history of pancreatitis, albumin serum value, and preoperative oncologic treatment (chemotherapy or chemoradiotherapy) in case of malignancy, operative data included type and duration of surgery, the need for a resection extended to close organs and for vascular resection/reconstruction, pathological data included tumor type and diameter and surgical margin status.
Surgical technique and patient management
A detailed description of our standardized technique for L-RAMPS has been previously published by our group [8]. Concerning L-DPS, peripancreatic dissection at the pancreatic inferior margin starts at the neck of the pancreas, at the point where the superior mesenteric vein underpasses the pancreas, and is continued left to completely separate the transverse mesocolon from the pancreas body and tail. Thereafter, the retropancreatic tunnel is dissected at the pancreatic neck, the splenic artery is transected after closure, and the pancreas is transected with stapler. Subsequently, the splenic vein is dissected and transected after closure with ligation and clips or with vascular stapler and the specimen mobilization is completed with spleno-diaphragmatic ligaments. Concerning L-SPDP, we adopted the technique of splenic vessels preservation: following peripancreatic dissection which is started about 2 cm right to the pancreatic lesion for which the procedure is performed and continued left with opening of the peritoneum at the pancreatic inferior margin, the pancreatic tail is identified. At this point, a retropancreatic tunnel is carefully prepared 2 cm right to the pancreatic lesion and the pancreas is transected with stapler. Subsequently, careful dissection of the pancreas from splenic vessels is performed, with separation of pancreatic vessels after closure with metallic clips or coagulation.
The surgical technique was selected according to preoperative diagnosis and to tumor location: L-RAMPS was performed for patients preoperatively diagnosed with high grade malignancies [mainly pancreatic ductal adenocarcinoma (PDAC)], L-SPDP for patients diagnosed with low-grade disease located in the pancreatic tail, L-PS for patients diagnosed with intermediate grade malignancy disease or by low grade malignancies located in the pancreatic body.
Pancreatic transection was performed with Endo-GIA Ultra Tri-Staple™ after a pre-firing compression with the same stapler. We used different kinds of cartridges, chosen according to intraoperative pancreatic thickness evaluation. Endo-GIA cartridges were classified according to staple height at closure (as predetermined by the manufacturers) in camel (1.25 mm), purple (1.75 mm), or black (2.25 mm). Clips over the pancreatic stapled line were placed according to operator preference.
In all patients included in this study, a silicon multi-tubular drain was placed in the abdomen at the end of surgery, with the intra-abdominal extremity possibly close to the pancreatic stump. Amylase activity was measured on serum and drain liquid at postoperative day 1, 3, 5, and 7. Intravenous Cefazolin was used as perioperative antibiotic prophylaxis. Somatostatin analogue was subcutaneously administered thrice a day since the day of surgery until the third postoperative day, and its administration was continued, in case of persistent elevated amylase serum activity, until normalization. In case of absence of pancreatic leak or infection, the abdominal drain was removed at postoperative day 5 or repeatedly retracted until removal. When a pancreatic leak protracted more than 10 days or in presence of drain liquid infection, the drain was replaced by interventional radiologists with a pig-tail drain, which was repeatedly retracted, in case of drain output reduction, until removal. In case of radiologic evidence of abdominal collection not adequately drained by the surgical drain, a radiological interventional drain of the collection, with eventual placement of a pig-tail drain, was performed.
Preoperative CT scan and video review data collection
Characteristic of pancreas, including pancreatic thickness, width, and fat infiltration and pancreatic duct diameter, were evaluated on preoperative 2-mm-slice high-resolution multi-detector computed tomography (CT) scan images by an experienced pancreatic radiologist (L.M.). Pancreatic thickness and width were measured at the site of pancreatic transection (determined based on the operative report) on preoperative CT scan: in particular, pancreatic thickness was measured on axial cuts (Fig. 2A1, D1) [9], pancreatic width on sagittal cuts (Fig. 2A2, D2).
Two oncologic surgeons (R.L. and A.M.), blinded for patients’ identity and postoperative outcomes, retrospectively and independently reviewed the videos of pancreatic stapled transection and recorded the following intraoperative technical data: Endo-GIA stapler cartridge used for transection, pancreatic capsule disruption (PCD) and staple line bleeding (SLB) respectively defined as a disruption/discontinuation of the pancreatic capsule and as a bleeding close to the staple line, both occurring soon after the pancreatic stapled transection (Figs. 2B, C, E and F; videos 1 and 2), and placement of hemostatic clips at pancreatic staple line. Disagreements during video review process were discussed by two reviewers until an agreement was reached.
A–C A 64 years old female underwent a L-DPS for high gr NET. Pancreatic thickness and width (A1 and A2) were measured (black dotted lines) anterior to splenic vein (black asterisk). Figures B and C show pancreatic capsule integrity with minimal staple line bleeding (camel cartridge used for transection). This patient had an uneventful postoperative recovery. D–F A 71 years old female underwent L-DPS for pancreatic body mucinous cyst. Pancreatic thickness (D1) and width (D2) were measured as indicated above. Figures E and F show posterior PCD and SLB (black cartridge used for transection). Postoperative period was characterized by a CR-POPF
Postoperative pancreatic fistula and complications definition and grading
International Study Group of Pancreatic Surgery (ISGPS) criteria [10] were used to diagnose and grade postoperative pancreatic fistula: in case of transient fistula without clinical consequences, with drain fluid amylase concentration higher than 3 times the upper normal serum value on or after postoperative day 3, a biochemical leak was diagnosed; in case of pancreatic fistula requiring changes in management (e.g. persistent drainage > 3 weeks, percutaneous or endoscopic drainage, angiographic procedures for bleeding, or signs of infection without organ failure) or requiring major changes in clinical management (e.g., reoperation, organ failure, or death), a POPF graded B and C was diagnosed, respectively, and such situation brought to a diagnosis of CR-POPF.
Postoperative complications were graded according to Clavien-Dindo classification [11]: complications graded equal to or higher than 3 were defined as major complications.
Statistical analysis
Statistical analysis was performed using the SPSS statistical software (version 23.0; SPSS Inc., Chicago, IL, USA). Demographic, clinical, radiologic, intraoperative, pathological characteristics were compared among patients according to the postoperative occurrence of CR-POPF, major complication, and of PCD and SLB separately and concomitant. Categorical variables were presented using frequency and percentages and were compared between groups using the Chi-square test or Fisher exact test, as appropriate. Continuous variables were presented as median and range and compared using Mann–Whitney U-test. Results with a p value < 0.05 were considered statistically significant; all p values were two-tailed. The performance of pancreatic thickness in predicting PCD, CR-POPF, and major complications was assessed using receiver operating characteristics (ROC) analysis. The accuracy of pancreatic thickness discriminating patients with and without PCD, CR-POPF, and major complications, respectively, was assessed by calculating the Area Under the Curve (AUC) and the asymptotic significance level of each curve compared with the diagonal reference line (area under the curve ¼ 0.500).
Results
Patient characteristics and comparison according to postoperative pancreatic fistula and major complications occurrence
As shown in Table 1, among 38 patients included in the current study the male to female ratio was roughly 1:2 and the median age and BMI were 62 years and 24, respectively. In 76% of patients one or more comorbidities were present, with 47% of patients having an ASA score higher than 2. Preoperative serum albumin median value was 4.2 g/dL. Respectively, 10.4% and 7.9% of patients had a history of previous pancreatitis and received a preoperative oncologic treatment (including chemotherapy or radiotherapy). Concerning preoperative CT scan evaluation of pancreas characteristics, median pancreatic thickness and width were 14 mm and 27 mm, respectively, and 29% of patients showed clear signs of pancreatic fat infiltration.
Concerning surgical data, median operation duration was 255 min and surgery consisted in L-RAMPS in 34% of patients, L-DPS in 48%, and L-SPDP in the remaining 18%. In all patients, before pancreatic stapled transection, a prefiring compression was performed, with a median duration of 75′. Immediately following pancreatic stapled transection, during which a camel (vascular), a purple (intestinal), and a black (high-volume) cartridge were used in 13%, 29%, and 58% of cases, a PCD occurred in 39% of patients, an SLB in 50%, and PCD and SLB were concomitant in 24% of patients. Horizon clips at staple line were used in 24% of patients to perform hemostasis and in 26% of patients were placed with a preventive purpose to cover the staple line complete length. The pancreatic resection was extended to the stomach in 2 cases and to the first jejunal loop at treitz in one case.
According to pathological assessment, final diagnosis was PDAC in 29% of patients, IPMN in 13%, NET in 26%, and other in 32%. Median tumor diameter was 30 mm and surgical margin positive for tumor cell was observed in 2 patients, both operated for PDAC. Concerning postoperative outcomes, overall and major complications occurred in 71% and 32% of patients, respectively. A post-pancreatectomy hemorrhage (PPH) occurred in 4 patients, a reoperation was needed in two patients, and the median length of hospital stay following surgery was 10 days.
CR-POPF occurred in 8 (out of 38, 21%) patients, all requiring radiologic interventional maneuvers to replace the surgical drain or to drain one or more abdominal collections, and was followed by PPH in 3 patients: one patient, following a L-SPDP, developed a bleeding from a pancreatic dorsal artery 8 days after surgery, and needed for urgent reoperation for hemostasis; one patient, on antiplatelet therapy for recent coronary stent placement, experienced a hemoperitoneum following L-RAMPS without clear sign of active bleeding at contrast enhanced CT scan and was treated conservatively with packed red blood cells and plasma transfusions, until bleeding gradually and spontaneously stopped; the last patient, following hospital discharge, had a bleeding from a jejunal artery and was treated with radiologic interventional embolization. Concerning characteristics of patients according to CR-POPF, a significantly higher median pancreatic thickness was observed in patients with CR-POPF, compared to those without CR-POPF. Concerning data gathered from retrospective video-review analysis, incidence of PCD and SLB, occurring both separately and concomitantly, were significantly higher among CR-POPF patients, compared to patients without CR-POPF. Finally, concerning postoperative outcomes, rates of major complications and PPH were significantly higher in case of CR-POPF occurrence.
Concerning patients with a major complication, this was directly related to a CR-POPF in 8 (67%) out of 12 patients, while in remaining 4 cases pulmonary embolism occurred and needed for Intensive Care Unit admission in one patient, hemoperitoneum occurred in two patients and was treated with packed red blood cells and plasma in one case and with emergency operation in the other, and an abdominal infected collection was treated with interventional radiologic drain in the last patient. Concerning differences in patient characteristics according to the occurrence of major complication, higher pancreatic thickness and higher rates of PCD overall and concomitant to SLB among patients with major complication was observed, compared to patients with minor/no postoperative complication.
Analysis of factors associated with PCD, SLB, and concomitant PCD and SLB
PCD occurred in 15 patients, SLB in 19, and concomitant PCB and SLB in 9. Patients with PCD had significantly higher pancreatic thickness and were more frequently male, compared to patients without PCD. Patients with and without PCD also differed according to type of surgery performed, with significant higher rate of SPDP, and concomitant lower rates of DSP and RAMPS, among PCD patients, compared to patients without PCD. Concerning comparison of patients with versus without SLB, significant differences regarding male sex rate and BMI, both higher among SLB patients compared to patients without SBL, could be found. Concerning patients with PCD + SLB, rate of male sex, pancreatic thickness, BMI were all significantly higher compared to patients without concomitant PCD and SBL. Furthermore, significant higher rate of SPDP, and concomitant lower rates of RAMPS, were observed among patients with PCD + SLB, as well as significantly higher rates of postoperative major complications and of PPH (Table 2).
Accuracy of measured pancreatic thickness for predicting PCD, CR-POPF, and major complication
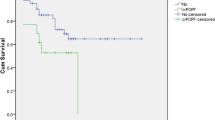
The ROC analysis revealed that 15.5 mm was the best cut-off value of pancreatic thickness to predict the occurrence of PCD (AUC = 0.949, confidence interval (CI) 0.887–1, asymptotic significance level p < 0.001), CR-POPF (AUC = 0.798, CI 0.632–0.963, asymptotic significance level p = 0.010), and major complication (AUC = 0.740, CI 0.565–0.916, asymptotic significance level p = 0.019) (Fig. 3).
Receiver operating characteristics curves for pancreatic thickness in the prediction of postoperative outcomes. ROC means receiving operating curve; AUC area under the curve, CI confidence interval, SE standard error, p values represent asymptotic significance (null hypothesis, AUC = .500); PCD means pancreatic capsule disruption; CR-POPF, clinically relevant postoperative pancreatic fistula
Discussion
In this analysis of postoperative outcomes of patients undergoing L-DP with triple-row stapled pancreatic transection we identified, by retrospective blinded surgery video-review focused on the step of pancreatic transection, intraoperative occurrence of PCD and SLB as predictors of CR-POPF and of postoperative major complications; in addition, a strong association between pancreatic thickness at transection point, measured on preoperative CT scan, and PCD occurrence was found.
Previous researches focused on identification of factors associated with CR-POPF highlighted the importance of patient related factors, indicating a younger age, male sex, comorbidities and nutritional status, surrogated by lower albumin serum value and by higher BMI, with an increased risk for CR-POPF occurrence. In addition, multiple surgical factors have been associated with the risk of CR-POPF, like increased operative time, multivisceral resection, splenectomy, and intraoperative blood loss [12,13,14,15]. Among factors pancreas-related, in addition to pancreatic duct obstruction due to increased Oddi sphincter pressure [16, 17], pancreatic thickness is probably the most studied [9, 18,19,20,21,22], with strong evidence associating increasing pancreatic thickness with an increased risk of CR-POPF, independently of pancreatic transection method and surgical approach.
Our results, showing a strong association between increasing pancreatic thickness (measured on preoperative contrast enhanced CT scan axial cuts, Fig. 2) and worsening of postoperative outcomes, with increasing rates of CR-POPF and major complication (Fig. 3), are consistent with such evidence. Through ROC analysis, a cut-off of 15.5 mm for pancreatic thickness was identified and a pancreatic thickness higher than 15.5 mm could predict a risk of CR-POPF with a sensibility and specificity of 75% and 74%, respectively, and a risk of major complication with a sensibility and specificity of 67% and 77%, respectively.
Recognized correlation between pancreatic thickness and CR-POPF has further encouraged research focused on the best modality for pancreatic stump closure, especially in case of thick pancreas, however, without a recognized superiority of stump suture closure [23, 24] over stapled closure, as well as without a clear benefit of the use of tissue patches at the staple line [25] or of staple line reinforcement [13, 26, 27], stapled closure remains one of the most commonly used pancreatic transection technique. Subsequent research has highlighted the importance of (i) techniques of pancreatic prefiring compression before pancreatic stapling in reducing POPF rates [28,29,30], (ii) discrepancy between pancreatic parenchyma thickness and stapler cartridge, which may be behind parenchyma crush and pancreatic juice leak and consequently (iii) a correct staple cartridge choice in mitigating the risk of CR-POPF [31, 32]. Our clinical practice is consistent with such data: among patients with pancreas thickness higher than 16 mm, the rate of use of high volume cartridge was higher (86%) than among patients with a pancreatic thickness ≤ 16 mm (50%); similarly, vascular and intestinal cartridges were used less frequently among patients with a thicker pancreas (0% and 14%, respectively), compared to patients with a thinner pancreas (12.5%, and 37.5%, respectively; p = 0.156, data not shown), indicating that the choice of the cartridge size was modulated according to pancreatic size in our series.
Our study, using a peculiar approach based on retrospective video-review analysis which is allowed by the availability of video-recorded surgeries, expands on above data, showing for the first time that the occurrence of PCD close to staple line, even more if concomitant to SLB, may be an intraoperatively detectable indicator of severe pancreatic traumatism during pancreatic transection. Patients with PCD and SLB had significantly higher rates of CR-POPF (both 87.5%), compared to those without (26.7% and 40%, respectively; p = 0.003 and 0.042, respectively), suggesting that PCD and SLB may be indicators of pancreatic traumatism due to stapled transection and precursors of CR-POPF. We also found that a combination of PCD and SLB (Video 1), observed in 9 patients, was the best predictor of both CR-POPF and major complication (p < 0.001 for both comparisons) and may better surrogate the pancreatic traumatism preceding an unfavorable outcome while among 16 patients with SLB not associated to PCD (n = 10) or with PCD not associated with SLB (n = 6), no CR-POPF was observed and only three patients had a biochemical pancreatic leak (Video 2). We believe that these findings should lead to undertake particular attention in postoperative management of patients with PCD/SLB, like (i) delaying retraction/removal of surgical drain eventually after CT scan exclusion of abdominal collection, (ii) anticipating radiologic interventional replacement of surgical drain even without sign of surgical drain obstruction, (iii) continuing intraoperative antibiotic profilaxis in the postoperative period even in the absence of drain infection, (iv) continuing Octreotide analogue administration after postoperative day three, even in case of amylase serum activity normalization. When looking for factors associated with PCD and SLB occurrence, we found that pancreatic thickness at pancreatic transection site was significantly higher among patients with PCD (19 mm) compared to non-PCD patients (13 mm, p < 0.001). However, differences in cartridge size, with higher rates of high volume cartridges used for patients with PCD, seem indicating that the weighted choice of the stapler cartridge according to pancreatic thickness could not mitigate the risk of PCD among patients with thicker pancreas, because of the absence of an adequate cartridge for thick pancreas. Of 15 patients with PCD, 9 had a pancreatic thickness higher than 17 mm and remaining 6 had a median pancreatic thickness of 15 mm: this data support the results (strong agreement concerning the Statement 12–1) of the recent expert consensus guidelines by the ISGPS on Pancreatic Transection Plane management following DP [33], suggesting that a stapled transection may not be indicated for patients with a thick pancreas undergoing DP. In the meantime, the relatively high incidence of PCD in the current study may account for the high rate of CR-POPF and of major complication in our experience: almost 1/3 of study patients had a major complication, however, this may be partially related to our extensive use of interventional radiology drain replacement in case of protracted pancreatic leak or of drain liquid infection. In addition, while 83% of patients with a major complication could be managed by interventional radiology, only 17% (2 out of 12 patients) required a reoperation.
This study has some limitations: first of all the small number of patients included, which undoubtedly reduced the validity of our results and precluded from the assessment of PCD and SLB in multivariate analysis of factors independently associated with CR-POPF and major complications. However, only patients operated with a laparoscopic approach, using tri-rows stapler for pancreatic transection following prefiring compression (median time of 75 s in the overall study group) were included in this study, making our research actual, given that L-DP is not only superior to an open approach for benign and low-grade malignant tumors [34] but is also increasingly considered feasible, safe, and oncologically equivalent to open DP for pancreatic ductal adenocarcinoma (PDAC) even in case of advanced disease requiring vascular resection, when performed at experienced centers [6, 7, 35]. Further limitations of this study are its retrospective nature and the unusual and not validated use of video-review to detect intraoperative factors associated with postoperative outcome, methodology which may be responsible for missing important un-investigated factors potentially affecting postoperative outcomes, however, data assessed in the current analyses were prospectively collected and both preoperative CT scan assessment for pancreatic measures and video-review for intraoperative findings were performed by one radiologist and two surgeons with extensive experience in the field of pancreatic radiology and surgery and blinded for postoperative outcomes, increasing reliability of results and reducing impact of selection bias.
Finally, while acknowledging that pancreatic texture/consistency may represent an important factor to take into account when investigating results of DP, due to the fact that pancreatic consistency was not specified in the majority of operative reports of our study patients, we could not include such characteristic in the analysis of factors associated with postoperative outcomes. However, from video reviews performed during preparation of the current manuscript, we had the impression that a dichotomous separation of patients based on pancreatic texture (“hard” versus “soft”) may lack precision when investigating stapled DP. Contrarily to pancreatoduodenectomy, where in the majority of available anastomotic techniques the pancreatic stump needs to be connected to the jejunum or to the stomach with a suture, highlighting the importance of pancreatic hardness for the anastomotic tightness, we believe that, during stapled DP, flexibility and elasticity of pancreas in toto and of pancreatic capsule in particular, more than pancreatic hardness, may reduce the risk of PCD/SBL during stapled transection.
In conclusion, this is the first study to associate intraoperative indicators of pancreatic traumatism detected by retrospective video-review of pancreatic transection step of L-DP with postoperative unfavorable outcomes. Patients with PCD, even more when this was concomitant to SBL, had increased rates of CR-POPF and postoperative major complication and may benefit from a stricter postoperative monitoring. Patients with a thicker pancreas are expected to have a higher risk of severe pancreatic traumatism during stapled transection, independently of the adequate choice of cartridge size according to pancreatic thickness, indicating that, for patients with a thicker pancreas, alternative techniques to stapled pancreatic transection should be warranted [33]. However, larger studies are needed for validation of our findings.
References
Callery MP, PrattWB KTS, Chaikof EL, Vollmer CM Jr (2013) A prospectively validated clinical risk score accurately predicts pancreatic fistula after pancreatoduodenectomy. J Am Coll Surg 216:1–14
Addeo P, Delpero JR, Paye F, Oussoultzoglou E, Fuchshuber PR, Sauvanet A, Sa Cunha A, Le Treut YP, Adham M, Mabrut JY, Chiche L, Bachellier P, Association FS, (AFC). (2014) Pancreatic fistula after a pancreaticoduodenectomy for ductal adenocarcinoma and its association with morbidity: a multicentre study of the French Surgical Association. HPB (Oxford) 16:46–55
Fernández-del Castillo C, Morales-Oyarvide V, McGrath D, Wargo JA, Ferrone CR, Thayer SP, Lillemoe KD, Warshaw AL (2012) Evolution of the Whipple procedure at the Massachusetts General Hospital. Surgery 152(Suppl 1):S56–S63
Sato N, Tamura T, Minagawa N, Hirata K (2016) Preoperative body mass index-to-prognostic nutritional index ratio predicts pancreatic fistula after pancreaticoduodenectomy. Hepatobiliary Surg Nutr 5:256–262
Ecker BL, McMillan MT, Allegrini V, Bassi C, Beane JD, Beckman RM, Behrman SW, Dickson EJ, Callery MP, Christein JD, Drebin JA, Hollis RH, House MG, Jamieson NB, Javed AA, Kent TS, Kluger MD, Kowalsky SJ, Maggino L, Malleo G, Valero V 3rd, Velu LKP, Watkins AA, Wolfgang CL, Zureikat AH, Vollmer CM Jr (2019) Risk factors and mitigation strategies for pancreatic fistula after distal pancreatectomy: analysis of 2026 resections from the international, multi-institutional distal pancreatectomy study group. Ann Surg 269(1):143–149
Zimmitti G, Manzoni A, Garatti M, Rosso E (2020) ASO author reflections: pushing the limits of resection for left pancreatic cancer: from conventional distal pancreatosplenectomy, to laparoscopic radical antegrade modular pancreatosplenectomy, until vein resection for vascular tumor involvement. Ann Surg Oncol 27(8):2904–2905. https://doi.org/10.1245/s10434-020-08343-7
Rosso E, Frey S, Zimmitti G, Manzoni A, Garatti M, Iannelli A (2020) Laparoscopic radical antegrade modular pancreatosplenectomy with vascular resection for pancreatic cancer: tips and tricks. J Gastrointest Surg. https://doi.org/10.1007/s11605-020-04695-3
Zimmitti G, Manzoni A, Garatti M, Sega V, Rosso E (2018) Technique of “mini-invasive radical antegrade modular pancreatosplenectomy” for pancreatic cancer. Dig Med Res 1:21. https://doi.org/10.21037/dmr.2018.09.06
Sugimoto M, Gotohda N, Kato Y, Takahashi S, Kinoshita T, Shibasaki H, Nomura S, Konishi M, Kaneko H (2013) Risk factor analysis and prevention of postoperative pancreatic fistula after distal pancreatectomy with stapler use. J Hepatobiliary Pancreat Sci 20:538–544
Bassi C, Marchegiani G, Dervenis C, Sarr M, Abu Hilal M, Adham M, Allen P, Andersson R, Asbun HJ, Besselink MG, Conlon K, Del Chiaro M, Falconi M, Fernandez-Cruz L, Fernandez-Del Castillo C, Fingerhut A, Friess H, Gouma DJ, Hackert T, Izbicki J, Lillemoe KD, Neoptolemos JP, Olah A, Schulick R, Shrikhande SV, Takada T, Takaori K, Traverso W, Vollmer CR, Wolfgang CL, Yeo CJ, Salvia R, Buchler M (2017) International study Group on pancreatic surgery (ISGPS). The 2016 update of the international study Group (ISGPS) definition and grading of postoperative pancreatic fistula: 11 Years after. Surgery 161:584–591
Dindo D, Demartines N, Clavien P-A (2004) Classification of surgical complications: a new proposal with evaluation in a cohort of 6336 patients and results of a survey. Ann Surg 240(2):205–213
Kleeff J, Diener MK, Zgraggen K, Hinz U, Wagner M, Bachmann J, Zehetner J, Müller MW, Friess H, Büchler MW (2007) Distal pancreatectomy: risk factors for surgical failure in 302 consecutive cases. Ann Surg 245:573–582
Ferrone CR, Warshaw AL, Rattner DW, Berger D, Zheng H, Rawal B, Rodriguez R, Thayer SP, Fernandez-del CC (2008) Pancreatic fistula rates after 462 distal pancreatectomies: staplers do not decrease fistula rates. J Gastrointest Surg 12(10):1691–1697
Goh BK, Tan YM, Chung YF, Cheow PC, Ong HS, Chan WH, Chow PK, Soo KC, Wong WK, Ooi LL (2008) Critical appraisal of 232 consecutive distal pancreatectomies with emphasis on risk factors, outcome, and management of the postoperative pancreatic fistula: a 21-year experience at a single institution. Arch Surg 143:956–965
Sierzega M, Niekowal B, Kulig J, Popiela T (2007) Nutritional status affects the rate of pancreatic fistula after distal pancreatectomy: a multivariate analysis of 132 patients. J Am Coll Surg 205:52–59
Hashimoto Y, Traverso LW (2012) After distal pancreatectomy pancreatic leakage from the stump of the pancreas may be due to drain failure or pancreatic ductal back pressure. J Gastrointest Surg 16:993–1003
Hackert T, Klaiber U, Hinz U, Kehayova T, Probst P, Knebel P, Diener MK, Schneider L, Strobel O, Michalski CW, Ulrich A, Sauer P, Büchler MW (2017) Sphincter of Oddi botulinum toxin injection to prevent pancreatic fistula after distal pancreatectomy. Surgery 161:1444–1450
Eguchi H, Nagano H, Tanemura M, Takeda Y, Marubashi S, Kobayashi S, Wada H, Umeshita K, Mori M, Doki Y (2011) A thick pancreas is a risk factor for pancreatic fistula after a distal pancreatectomy: selection of the closure technique according to the thickness. Dig Surg 28:50–56
Mendoza AS 3rd, Han HS, Ahn S, Yoon YS, Cho JY, Choi Y (2016) Predictive factors associated with postoperative pancreatic fistula after laparoscopic distal pancreatectomy: a 10-year single-institution experience. Surg Endosc 30:649–656
Okano K, Oshima M, Kakinoki K, Yamamoto N, Akamoto S, Yachida S, Hagiike M, Kamada H, Masaki T, Suzuki Y (2013) Pancreatic thickness as a predictive factor for postoperative pancreatic fistula after distal pancreatectomy using an endopath stapler. Surg Today 43:141–147
Kawai M, Tani M, Okada K, Hirono S, Miyazawa M, Shimizu A, Kitahata Y, Yamaue H (2013) Stump closure of a thick pancreas using stapler closure increases pancreatic fistula after distal pancreatectomy. Am J Surg 206:352–359
Nakamura M, Shindo K, Ideno N, Ueda J, Takahata S, Nakashima H, Ohtsuka T, Shimizu S, Oda Y, Tanaka M (2014) Prediction of pancreatic fistula by preoperatively assessable factors; retrospective review of unified operations by single surgeon. Hepatogastroenterology 61:834–837
Miyasaka Y, Mori Y, Nakata K, Ohtsuka T, Nakamura M (2017) Attempts to prevent postoperative pancreatic fistula after distal pancreatectomy. Surg Today 47:416–424
Diener MK, Seiler CM, Rossion I, Kleeff J, Glanemann M, Butturini G, Tomazic A, Bruns CJ, Busch OR, Farkas S, Belyaev O, Neoptolemos JP, Halloran C, Keck T, Niedergethmann M, Gellert K, Witzigmann H, Kollmar O, Langer P, Steger U, Neudecker J, Berrevoet F, Ganzera S, Heiss MM, Luntz SP, Bruckner T, Kieser M, Büchler MW (2011) Efficacy of stapler versus hand-sewn closure after distal pancreatectomy (DISPACT): a randomised, controlled multicentre trial. Lancet 377:1514–1522
Carter TI, Fong ZV, Hyslop T, Lavu H, Tan WP, Hardacre J, Sauter PK, Kennedy EP, Yeo CJ, Rosato EL (2013) A dual-institution randomized controlled trial of remnant closure after distal pancreatectomy: does the addition of a falciform patch and fibrin glue improve outcomes? J Gastrointest Surg 17:102–109
Johnston FM, Cavataio A, Strasberg SM, Hamilton NA, Simon PO Jr, Trinkaus K, Doyle MB, Mathews BD, Porembka MR, Linehan DC, Hawkins WG (2009) The effect of mesh reinforcement of a stapled transection line on the rate of pancreatic occlusion failure after distal pancreatectomy: review of a single institution’s experience. HPB (Oxford) 11:25–31
Ceppa EP, McCurdy RM, Becerra DC, Kilbane EM, Zyromski NJ, Nakeeb A, Schmidt CM, Lillemoe KD, Pitt HA, House MG (2015) Does pancreatic stump closure method influence distal pancreatectomy outcomes? J Gastrointest Surg 19:1449–1456
Nakamura M, Ueda J, Kohno H, Aly MY, Takahata S, Shimizu S, Tanaka M (2011) Prolonged peri-firing compression with a linear stapler prevents pancreatic fistula in laparoscopic distal pancreatectomy. Surg Endosc 25:867–871
Okano K, Kakinoki K, Suto H, Oshima M, Maeda N, Kashiwagi H, Yamamoto N, Akamoto S, Fujiwara M, Takama H, Hagiike M, Usuki H, Suzuki Y (2010) Slow parenchymal flattening technique for distal pancreatectomy using an endopath stapler: simple and safe technical management. Hepatogastroenterology 57:1309–1313
Hirashita T, Ohta M, Yada K, Tada K, Saga K, Takayama H, Endo Y, Uchida H, Iwashita Y, Inomata M (2018) Effect of pre-firing compression on the prevention of pancreatic fistula in distal pancreatectomy. Am J Surg 216(3):506–510
Nishikawa M, Yamamoto J, Hoshikawa M, Einama T, Noro T, Aosasa S, Tsujimoto H, Ueno H, Kishi Y (2019) Stapler sizes optimized for pancreatic thickness can reduce pancreatic fistula incidence after distal pancreatectomy. Surg Today. https://doi.org/10.1007/s00595-019-01929-z
Sugimoto M, Kendrick ML, Farnell MB, Nomura S, Takahashi N, Kobayashi T, Kobayashi S, Takahashi S, Konishi M, Gotohda N (2019) Relationship between pancreatic thickness and staple height is relevant to the occurrence of pancreatic fistula after distal pancreatectomy. HPB (Oxford). https://doi.org/10.1016/j.hpb.2019.07.010
Miao Y, Lu Z, Yeo CJ, Vollmer CM Jr, Fernandez-Del Castillo C, Ghaneh P, Halloran CM, Kleeff J, de Rooij T, Werner J, Falconi M, Friess H, Zeh HJ, Izbicki JR, He J, Laukkarinen J, Dejong CH, Lillemoe KD, Conlon K, Takaori K, Gianotti L, Besselink MG, Del Chiaro M, Montorsi M, Tanaka M, Bockhorn M, Adham M, Oláh A, Salvia R, Shrikhande SV, Hackert T, Shimosegawa T, Zureikat AH, Ceyhan GO, Peng Y, Wang G, Huang X, Dervenis C, Bassi C, Neoptolemos JP, Büchler MW, International Study Group of Pancreatic Surgery (ISGPS) (2020) Management of the pancreatic transection plane after left (distal) pancreatectomy: expert consensus guidelines by the International Study Group of Pancreatic Surgery (ISGPS). Surgery 168(1):72–84. https://doi.org/10.1016/j.surg.2020.02.018
Asbun HJ, Moekotte AL, Vissers FL, Kunzler F, Cipriani F, Alseidi A, D'Angelica MI, Balduzzi A, Bassi C, Björnsson B, Boggi U, Callery MP, Del Chiaro M, Coimbra FJ, Conrad C, Cook A, Coppola A, Dervenis C, Dokmak S, Edil BH, Edwin B, Giulianotti PC, Han HS, Hansen PD, van der Heijde N, van Hilst J, Hester CA, Hogg ME, Jarufe N, Jeyarajah DR, Keck T, Kim SC, Khatkov IE, Kokudo N, Kooby DA, Korrel M, de Leon FJ, Lluis N, Lof S, Machado MA, Demartines N, Martinie JB, Merchant NB, Molenaar IQ, Moravek C, Mou YP, Nakamura M, Nealon WH, Palanivelu C, Pessaux P, Pitt HA, Polanco PM, Primrose JN, Rawashdeh A, Sanford DE, Senthilnathan P, Shrikhande SV, Stauffer JA, Takaori K, Talamonti MS, Tang CN, Vollmer CM, Wakabayashi G, Walsh RM, Wang SE, Zinner MJ, Wolfgang CL, Zureikat AH, Zwart MJ, Conlon KC, Kendrick ML, Zeh HJ, Hilal MA, Besselink MG, International Study Group on Minimally Invasive Pancreas Surgery (I-MIPS) (2020) The Miami international evidence-based guidelines on minimally invasive pancreas resection. Ann Surg 271(1):1–14
Rosso E, Manzoni A, Zimmitti G et al (2020) Laparoscopic radical antegrade modular pancreatosplenectomy with venous tangential resection. Focus on periadventitial dissection of the superior mesenteric artery for obtaining negative margin and a safe vascular resection. Ann Surg Oncol 27(8):2902–2903. https://doi.org/10.1245/s10434-020-08271-6
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Disclosures
Drs. Giuseppe Zimmitti, Roberta La Mendola, Alberto Manzoni, Valentina Sega, Valentina Malerba, Elio Treppiedi, Claudio Codignola, Lorenzo Monfardini, Marco Garatti, Edoardo Rosso have no conflicts of interest or financial ties to disclose.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Supplementary file1 (WMV 75988 kb)
Supplementary file2 (WMV 79248 kb)
Rights and permissions
About this article
Cite this article
Zimmitti, G., La Mendola, R., Manzoni, A. et al. Investigation of intraoperative factors associated with postoperative pancreatic fistula following laparoscopic left pancreatectomy with stapled closure: a video review-based analysis. Surg Endosc 35, 941–954 (2021). https://doi.org/10.1007/s00464-020-07912-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00464-020-07912-x