Abstract
Background
Approximately, 22.6% of colorectal cancer surgeries were performed on patients aged 80 or over. The present study aimed to evaluate the use of laparoscopic resection and its short-term surgical outcomes in patients who were aged 80 and older and diagnosed with colon cancer or rectal cancer in parallel.
Methods
In this retrospective population-based study, colon and rectal cancer patients ≥ 80 years undergoing laparoscopic resection or open resection were identified from the United States National Inpatient Sample (2005–2014). Primary outcomes were postoperative complication and in-hospital mortality. Logistic regression analyses were performed to assess the short-term effectiveness of laparoscopic and open resection.
Results
In this study, 40,451 colon cancer patients and 1117 rectal cancer patients were included. Multivariate analysis revealed that laparoscopic resection was significantly associated with lower risks for developing postoperative complications (aOR = 0.67; 95%, CI 0.64–0.71) and in-hospital mortality (aOR = 0.37; 95% CI 0.32–0.43) compared to open resection in colon cancer patients. For rectal cancer patients, multivariate analysis indicated that laparoscopic resection was significantly associated with a lower risk of developing postoperative complications (aOR = 0.41; 95% CI 0.32–0.52) but was not associated with in-hospital mortality.
Conclusion
Compared to open resection, laparoscopic resection has better or similar short-term surgical outcomes in colon and rectal cancer patients ≥ 80 years.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Improvement in life expectancy has increased the number of elderly individuals, resulting in aging of the world population. According to the World Health Organization, people over 60 accounted for around 12% of world population in 2015, which was expected to increase to 22% in 2050 [1]. Particularly, people aged 80 years and older are the most rapidly growing age group worldwide [2]. On the other hand, colorectal cancer (CRC) is one of the most common causes of cancer-related deaths worldwide [3,4,5], and the global burden of CRC is except to rise in the near future [6]. An analysis of the United States (US) National Inpatient Sample (NIS) found that 63.8% of CRC surgeries were performed on patients aged 65 or over, and 22.6% on patients aged 80 or over [3]. In addition, it was estimated that CRC caused 187,140 deaths in the US in 2014, and more than one-third deaths from CRC occurred in patients aged 80 and older [7]. Elderly patients aged 80 and older are often regarded as high-risk surgical candidates and are potentially associated with higher rates of severe postoperative complications and direct operative mortality [8, 9]; therefore, selecting appropriate surgical treatment strategies for elderly patients with CRC is critical in clinical practice.
Laparoscopic resection and open resection are the two most commonly used surgical treatments of CRC. Two randomized trials found that laparoscopic and open surgeries achieve similar short-term outcomes in CRC patients, although laparoscopic resection is associated with prolonged operating time [10, 11]. As a minimally invasive surgery, laparoscopic surgery is associated with lower blood loss during surgery, less wound complications, and short hospital stay in CRC patients, as compared to open surgery [8, 12]. As a result, the utilization of laparoscopic surgery for CRC is increasing [13]. Although laparoscopic resection was assumed to be preferable for elderly patients with CRC [9], controversial results on the utilization of laparoscopic resection in CRC patients aged 80 or over have been reported. No significant differences in postoperative complications between laparoscopic and open surgeries were observed in Japanese CRC patients aged 80 and older [14], while Korean CRC patients aged 80 and older have an elevated risk of postoperative morbidity after laparoscopic resection [15]. Several lines of evidence demonstrated beneficial effects of laparoscopic resection in elderly patients with CRC [16,17,18], but most studies did not exclusively investigate CRC patients aged 80 or over.
CRC develops from the colon or rectum. However, since colon cancer and rectal cancer have different molecular developmental mechanisms and metastatic patterns [19, 20], they are indeed two separate tumor entities requiring distinct treatment approaches [21, 22]. Colon cancer and rectal cancer should therefore be considered independently while evaluating effectiveness of laparoscopic resection. Hence, the purposes of the present population-based study were to gain an overview about the use of laparoscopic resection in patients aged 80 and older diagnosed with colon cancer or rectal cancer in parallel, and to evaluate short-term surgical outcomes (postoperative complications and in-hospital mortality) of laparoscopic resection, compared to open resection, in elderly colon and rectal cancer patients.
Materials and methods
Data source
The present population-based analysis was performed using data from the NIS between 2005 and 2014. The NIS, part of the Healthcare Cost and Utilization Project (HCUP) under the Agency for Healthcare Research and Quality (AHRQ), is the largest inpatient health care database in the US. The NIS contains clinical and non-clinical information on all participating hospitalized patients, including patient demographics, primary and secondary diagnoses, primary and secondary procedures, admission and discharge status, length of stay, and hospital characteristics.
To conduct this data analysis, we had obtained certificate (number HCUP-5VW28M94I) from the Healthcare Cost and Utilization Project and conformed to the Data Use Agreement for the NIS from HCUP. Due to deidentification of the NIS, our study was exempt from hospital/university review board approval and the need for informed consent was waived.
Study population
We used diagnostic and procedural codes specified by the International Classification of Diseases, 9th Revision, Clinical Modification (ICD-9-CM) to identify all patients aged 80 or over who underwent laparoscopic resection or open resection for the treatment of colon cancer or rectal cancer from the NIS between 2005 and 2014. Elderly patients admitted with the diagnosis of colon cancer (codes 153.0–153.9, 209.12–209.16, and 230.3) were sampled. Subsequently, colon cancer patients undergoing laparoscopic resection (codes 17.31–17.39, 45.42, 45.43, and 45.81) or open resection (codes 45.41, 45.71–45.79, and 45.82) were selected. On the other hand, elderly patients admitted with the diagnosis of rectal cancer (codes 154.0, 154.1, 209.17, and 230.4) were identified. Later, rectal cancer patients undergoing laparoscopic resection (codes 48.36, 48.42, and 48.51) or open resection (codes 48.43 and 48.52) were identified.
Study variables and primary outcomes
Covariates, such as patient demographics (age, sex and race), admission type, hospital status, and region of hospital, were extracted from the NIS. Patients’ preoperative comorbidities were quantified using validated Elixhauser coding algorithms available for ICD-9-CM codes [23].
Primary endpoints of this study were postoperative complication and in-hospital mortality. Postoperative complications included anastomotic leak (code 997.49), intra-abdominal abscess (code 567.22), urinary tract infection (code 599.0), acute renal failure (code 584.9), cardiovascular complications (codes 410.0–410.9, 997.1, and 998.0), ileus/bowel obstruction (codes 560.1 and 560.9), postoperative infection (codes 998.51, 998.59, and 999.3), respiratory complications (codes 415.1 and 997.3), and complications of hematomas (codes 998.11–998.13).
Statistical analysis
Descriptive statistics of the patients were presented as n (%), unweighted number (n) and weighted percentage (%). Since the NIS database covers 20% samples of the USA annual inpatient admissions, weighted samples (DISCWT), stratum (NIS_STRATUM), and cluster (HOSPID) were used to produce national estimates for all analyses. Differences between laparoscopic and open resections were compared using the PROC SURVEYFREQ and PROC SURVEYMEANS for categorical and continuous variables, respectively. The univariate logistic regression analysis via PROC SURVEYLOGISTIC was performed to determine the association between binary outcome variables (having any postoperative complication and in-hospital mortality) and surgery types, along with patients’ demographics, admission type, and Elixhauser comorbidity score. All covariates examined in the univariate regression model were then adjusted for in the multivariate logistic regression analysis to evaluate the association between short-term surgical outcomes and surgery types. Statistical significance was set at p < 0.05 and all reported p values were two-tailed. Data were analyzed using the SAS statistical software package, version 9.4 (SAS Institute Inc., Cary, NC, USA).
Results
Demographic and clinical characteristics
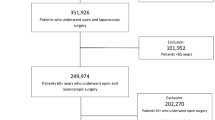
In the present retrospective study, 110,032 patients who were aged ≥ 80 and diagnosed with either colon cancer or rectal cancer were identified from the NIS database (2005 to 2014) (Fig. 1). After excluding patients with missing values of covariates (n = 2306) and patients with unidentified surgery type (n = 66,157 patients), the final analytic samples consisted of 40,451 colon cancer patients and 1117 rectal cancer patients. Using discharge weights, the analytic sample sizes of colon and rectal cancer patients were equivalent to population-based sample sizes of 200,254 colon cancer patients and 5513 rectal cancer patients, respectively. Of eligible colon cancer patients, 9932 (24.6%) patients underwent laparoscopic resection and 30,519 (75.4%) received open resection. On the other hand, there were 599 (53.6%) rectal cancer patients with laparoscopic resection and 518 (46.4%) with open resection (Fig. 1).
The demographic and clinical characteristics of included colon and rectal cancer patients are summarized in Table 1. Among eligible colon cancer patients, 51.5% of patients were aged between 80 and 84, 61.1% were female, 85.3% were white, 54.4% were admitted electively, 60.5% had Elixhauser comorbidity score of 3, 41.3% had at least one postoperative complication, and 5.0% died in hospital (Table 1). There were significant differences in sex, race, admission type, location/teaching status of hospital, region of hospital, Elixhauser comorbidity score, having any postoperative complication, and in-hospital mortality between two surgery groups (p ≤ 0.0100, Table 1). Among 9932 colon cancer patients undergoing laparoscopic resection, 3404 (34.3%) patients developed postoperative complication(s), and 209 (2.1%) died in hospitals. In contrast, 13,336 (43.7%) out of 30,519 colon cancer patients receiving open resection had postoperative complication(s), and 1836 (6.0%) died in hospitals (Table 1).
On the other hand, 59.1% of eligible rectal cancer patients were aged between 80 and 84. 51.2% were male, 83.0% were white, 65.1% were admitted electively, 54.3% had Elixhauser comorbidity score of 3, 39.8% developed at least one postoperative complication, and 3.2% died in hospital (Table 1). Significant differences in age, sex, admission type, region of hospital, and having any postoperative complication between two surgery groups (p ≤ 0.0079, Table 1). Notably, in-hospital mortality rates were similar between rectal cancer patients undergoing laparoscopic and open resection (p = 0.1872). Of 599 rectal cancer patients receiving laparoscopic resection, 185 (30.7%) patients developed postoperative complication(s), and 16 (2.7%) died in hospitals. In contrast, 261 (50.3%) out of 518 rectal cancer patients with open resection had postoperative complication(s), and 19 (3.8%) died in hospitals (Table 1).
Preoperative comorbidities
The preoperative comorbidities in colon and rectal cancer patients undergoing laparoscopic or open resection are shown in Supplementary Table 1. The top five most common preoperative comorbidities in colon cancer patients aged 80 and older were hypertension (67.2%), anemia (43.6%), fluid and electrolyte disorders (32.4%), metastatic cancer (27.6%), and renal failure (24.2%). Among colon cancer patients, the percentages of anemia, rheumatoid arthritis/collagen vascular disease, depression, diabetes, hypertension, hypothyroidism, other neurological disorders, obesity, peripheral vascular disorders, pulmonary circulation disorders, and renal failure were significantly higher in patients undergoing laparoscopic resection than those with open resection (p ≤ 0.0052, Supplementary Table 1). Nevertheless, colon cancer patients receiving laparoscopic resection had significantly lower percentages of congestive heart failure, fluid and electrolyte disorders, metastatic cancer, and weight loss than those undergoing open resection (p < 0.0001, Supplementary Table 1).
On the contrary, the top five most common preoperative comorbidities in elderly rectal cancer patients were hypertension (67.9%), anemia (33.2%), fluid and electrolyte disorders (30.5%), diabetes (21.1%), and chronic pulmonary disease (18.6%). Of rectal cancer patients, the laparoscopic resection group had significantly higher percentages of congestive heart failure, chronic pulmonary disease, other neurological disorders, and renal failure than the open resection group (p ≤ 0.0053, Supplementary Table 1). However, the percentages of lymphoma, fluid and electrolyte disorders, metastatic cancer, and weight loss were significantly lower in the laparoscopic resection group than those in the open resection group (p ≤ 0.0080, Supplementary Table 1).
Postoperative complications
The postoperative complications in colon and rectal cancer patients receiving laparoscopic or open resection are summarized in Table 2. Notably, regardless of cancer type and surgical approach, the five most common postoperative complications were ileus/bowel obstruction, urinary tract infection, acute renal failure, anastomotic leak, and cardiovascular complication, although the respective complication rates varied between two surgery groups in colon and rectal cancer patients (Table 2).
Colon cancer patients treated by laparoscopic resection were significantly less likely to develop a postoperative complication, compared to those undergoing open resection (34.3% vs. 43.7%, p < 0.0001, Table 2). Compared to open resection, laparoscopic resection resulted in significantly less complication rates in terms of intro-abdominal abscess, urinary tract infection, cardiovascular complications, ileus/bowel obstruction, postoperative infection, respiratory complications, and complication of hematomas (p ≤ 0.00478, Table 2). However, colon cancer patients undergoing laparoscopic resection had a significantly higher percentage of anastomotic leak than those with open resection (p < 0.0001, Table 2).
On the other hand, rectal cancer patients with laparoscopic resection were significantly less likely to have a postoperative complication than those with open resection (30.7% vs. 50.3%, p < 0.0001, Table 2). After laparoscopic resection, the percentages of rectal cancer patients developing anastomotic leak, intro-abdominal abscess, acute renal failure, cardiovascular complications, ileus/bowel obstruction, postoperative infection, or respiratory complications were significantly lower, compared to those of patients undergoing open resection (p ≤ 0.0444, Table 2).
After adjustment for age, sex, admission type, and Elixhauser comorbidity score, multivariate analysis revealed that colon cancer patients undergoing laparoscopic resection had a significantly lower risk of developing postoperative complications than those with open resection [adjusted odds ratio (aOR) = 0.67; 95% confidence interval (CI) 0.64–0.71, p < 0.0001] (Table 3). Moreover, multivariate analysis indicated that female (aOR = 0.81; 95% CI 0.78–0.85, p < 0.0001) was a protective factor for postoperative complication. In contrast, older age (≥ 90 years: aOR = 1.22; 95% CI 1.15–1.30, p < 0.0001; 85–89 years: aOR = 1.12; 95% CI 1.07–1.17, p < 0.0001), non-elective admission (aOR = 1.80; 95% CI 1.72–1.88, p < 0.0001), and higher Elixhauser comorbidity scores (3: aOR = 1.68; 95% CI 1.50–1.88, p < 0.0001; 2: aOR = 1.13; 95% CI 1.01–1.27, p = 0.0339) were significantly associated with higher risks of postoperative complications in colon cancer patients (Table 4).
On the contrary, after adjusting for all covariates examined, multivariate analysis indicated that rectal cancer patients with laparoscopic resection had a significantly lower risk of developing postoperative complications than those with open resection (aOR = 0.41; 95% CI 0.32–0.52, p < 0.0001) (Table 4). In addition, multivariate analysis revealed that higher Elixhauser comorbidity scores (3: aOR = 4.81; 95% CI 2.80–8.27, p < 0.0001; 2: aOR = 2.70; 95% CI 1.54–4.74, p = 0.0006; 1: aOR = 2.16; 95% CI 1.19–3.93, p = 0.0116) were significantly associated with higher risks of postoperative complications in rectal cancer patients (Table 4). However, unlike in colon cancer patients, older age, sex, and admission type were not associated with postoperative complications in rectal cancer patients (Table 4).
In-hospital mortality
After adjustment for age, sex, admission type, Elixhauser comorbidity score, and having any postoperative complication, multivariate analysis revealed that colon cancer patients with laparoscopic resection had a significantly lower risk for in-hospital mortality compared to those with open resection (aOR = 0.37; 95% CI 0.32–0.43, p < 0.0001) (Table 5). In addition, multivariate analysis disclosed that older age (≥ 90 years: aOR = 1.67; 95% CI 1.48–1.89, p < 0.0001; 85–89 years: aOR = 1.23; 95% CI 1.11–1.36, p < 0.0001), non-elective admission (aOR = 2.47; 95% CI 2.23–2.75, p < 0.0001), and having any postoperative complication (aOR = 2.88; 95% CI 2.60–3.19, p < 0.0001) were significantly associated with higher risks of in-hospital mortality in colon cancer patients (Table 5). However, female (aOR = 0.66; 95% CI 0.60–0.72, p < 0.0001) was significantly associated with a lower risk of in-hospital mortality in colon cancer patients (Table 5).
After adjusting for all covariates examined, multivariate analysis indicated that laparoscopic resection and open resection resulted in comparable in-hospital mortality rates in rectal cancer patients (p = 0.4314) (Table 6). Furthermore, multivariate analysis revealed that rectal cancer patients with any postoperative complication had a significantly higher risk for in-hospital mortality than those without complications (aOR = 9.83; 95% CI 6.99–13.83, p < 0.0001) (Table 6). In contrast, aged 85–89 (aOR = 0.23; 95% CI 0.15–0.36, p < 0.0001) and Elixhauser comorbidity score of 3 (aOR = 0.21; 95% CI 0.11–0.41, p < 0.0001) were significantly associated with lower risks for in-hospital mortality in rectal cancer patients (Table 6).
Discussion
The present US population-based study simultaneously evaluated short-term surgical outcomes of laparoscopic resection in patients ≥ 80 years with either colon cancer or rectal cancer. The results indicated that 24.6% of colon cancer patients aged 80 and older underwent laparoscopic resection, while 53.6% of elderly rectal cancer patients received laparoscopic resection. Colon cancer patients with laparoscopic and open resection had total postoperative complication rates of 34.3% and 43.7%, as well as in-hospital mortality rates of 2.1% and 6.0%, respectively. In contrast, rectal cancer patients undergoing laparoscopic and open resection had total postoperative complication rates of 30.7% and 50.3%, as well as in-hospital mortality rates of 2.7% and 3.8%, respectively. Multivariate analyses revealed that compared to open resection, laparoscopic resection was significantly associated with lower risks of developing postoperative complications in both colon and rectal cancer patients. However, laparoscopic resection was significantly associated with a lower risk of in-hospital mortality in colon cancer patients, but not in rectal cancer patients. Overall, laparoscopic resection yielded better short-term surgical outcomes than open resection in colon and rectal cancer patients aged 80 and older.
It was estimated that about 43% of CRC patients were older than 75 years at the time of diagnosis [24]. An analysis of the US NIS reported that 22.6% of CRC surgeries were performed on patients aged 80 or over [3]. Compared to CRC patients younger than 65, CRC patients 80 years and above were more likely to be admitted urgently, to have prolonged hospital stay and higher hospital charge, and to be associated with elevated risks of postoperative morbidity and in-hospital mortality [3]. In addition, patients ≥ 80 years accounted for 29% and 43% of deaths caused by CRC in males and females, respectively, in the US in 2014 [7].
Furthermore, there were 721,988 and 281,253 patients diagnosed with colon cancer and rectal cancer, respectively, in the US from 2001 to 2010 [3]. There were 61,296 colon cancer patients and 34,175 rectal cancer patients in Japan in 2009 [5]. It was projected that there will be around 101,420 new cases of colon cancer and 44,180 new case of rectal cancer in the US in 2019 [25]. According to a US population-based study, approximately 27.0% of colon cancer patients and 14.5% of rectal cancer patients undergoing tumor resection were aged 80 and older [3]. Similarly, a Danish population-based study found that 37.7% of colon cancer patients and 26.4% of rectal cancer patients underwent surgical treatment at age 75 or over [26]. Hence, treatment of colon and rectal cancer patients aged 80 and older is an ongoing clinical task [9, 14, 15].
An analysis of US National Surgical Quality Improvement Program database demonstrated that laparoscopic resection was associated with lower postoperative complications, shorter length of stay, and lower mortality compared with open resection in colon cancer patients 65 years and above [27]. A retrospective Chinese cohort study of colon cancer patients aged 75 or over reported that laparoscopic resection had lower intraoperative blood loss, less analgesic consumption, and shorter hospital stay than open resection [28]. However, laparoscopic and open resection achieved comparable 5-year overall survival (OS) and disease-free survival (DFS) [28]. A multicenter study in Japan also found that laparoscopic resection was associated with fewer postoperative morbidities than open resection in colon cancer patients aged 80 or over; however, there were no significant differences in 3-year OS, DFS, and cancer-specific survival (CSS) between laparoscopic and open resection groups [29]. Nevertheless, a retrospective Italian cohort study of colon cancer patients with median age of 72 years demonstrated better 5-year OS and DFS for patients undergoing laparoscopic resection compared to those with open resection [30]. The present study found that laparoscopic resection had lower postoperative complications and in-hospital mortality than open resection in colon cancer patients 80 years and above, while long-term survival analysis of laparoscopic resection in elderly colon cancer patients is out of the scope of this study.
On the other hand, a retrospective Chinese cohort study of rectal cancer patients aged 70 or over found that laparoscopic resection was associated with longer operating time, less blood loss, a shorter hospital stay, lower overall postoperative complication rate, as well as less need of blood transfusion and surgical intensive care unit after surgery compared to open resection [31]. Nonetheless, there was no significant difference in 3-year OS between two surgery approaches in rectal cancer patients [31]. Similarly, in a Japanese cohort of rectal cancer patients aged 80 or over, there were no significant differences in postoperative morbidities, 3-year OS, DFS, and CSS between laparoscopic resection and open resection [29]. Notably, a German population-based study demonstrated that compared with open resection, laparoscopic resection was associated with a lower risk of 30-day postoperative mortality, but not 5-year DSF, in rectal cancer patients aged 80 and older [32]. The present study suggested that in rectal cancer patients ≥ 80 years, laparoscopic resection yielded lower postoperative complications than open resection but did not affect in-hospital mortality. However, long-term survival benefit of laparoscopic resection in elderly rectal cancer patients remains to be determined.
In the present study, ileus/bowel obstruction, urinary tract infection, acute renal failure, anastomotic leak, and cardiovascular complications were the five most common postoperative complications occurred in included colon and rectal cancer patients after laparoscopic or open resection. The similar findings have been previously reported [33, 34], and preoperative antibiotic prophylaxis was suggested to reduce postoperative complications, such as surgical site infection, anastomotic leak, and ileus, in CRC patients [35]. In the present study, the total complication rates of laparoscopic resection in colon and rectal cancer patients were 34.3% and 30.7%, respectively, which were significantly lower than those of open resection (43.7% and 50.3%, respectively). Furthermore, laparoscopic resection resulted in lower percentages of most respective complications studied regardless of cancer type, except for anastomotic leak in colon cancer.
On the other hand, a prospective multicenter study in Switzerland reported that the rate of bleeding complication was still substantial in laparoscopic surgery, which mainly relied on the surgeon's experience [36]. It was suggested that comorbidities, such as abnormal heart rate and hypertension, were risk factors for postoperative bleeding in colorectal surgery [34]. In the present study, among colon cancer patients undergoing laparoscopic resection, the percentages of patients with preoperative hypertension, congestive heart failure, and valvular disease were 72.3%, 16.7%, and 11.2%, respectively; however, only 2% of colon cancer patients developed complication of hematomas after laparoscopic resection. Similar phenomena, relatively high percentages of preoperative hypertension, congestive heart failure, and valvular disease, but relatively low complication rates of hematomas, were also observed in the other three patient groups (colon cancer patients with open resection, and rectal cancer patients with laparoscopic or open resection). Hence, the relationships between preoperative comorbidities and postoperative complications in elderly colon and rectal cancer patients undergoing laparoscopic or open resection remain to be explored.
It was suggested that the likelihood of admitted urgently is higher for CRC patients aged 80 and older [3]. Furthermore, older age was associated with an elevated risk of emergency admission in CRC patients [37]. The present study found that 45.6% of colon cancer patients and 34.9% of rectal cancer patients were admitted non-electively. In addition, non-elective admission was significantly associated with postoperative complications and in-hospital mortality in elderly colon cancer patients, but not in rectal cancer patients. However, the relationship between admission type and disease severity was not assessed in the present study.
The present study is strengthened by using the NIS database, so the included colon and rectal cancer patients represented 20% of the US elderly population undergoing laparoscopic or open resection during a 10-year period. Since short-term surgical outcomes of laparoscopic resection in elderly patients with colon and rectal cancer were assessed side by side, the current findings provide an overview on the use and effectiveness of laparoscopic resection in elderly colon and rectal patients, which may help clinicians to optimize the treatment strategies for these patients in the future.
Nevertheless, the present study has a few intrinsic limitations. The NIS database did not contain long-term oncological outcomes after discharge, so long-term survival could not be evaluated in the present study. In addition, a small proportion of CRC patients might require to undergo conversion from laparoscopic to open surgery for undisclosed reasons [10, 13, 38], while readmission rates and conversion rates could not be calculated due to the nature of NIS database. The ICD-9 coding system was used to identify cancer types, surgical procedures, preoperative comorbidities, and postoperative complications from the NIS database, while the possibility of coding errors could not be ruled out [39]. In addition, the severity of respective comorbidity was not available in the NIS database, which might bias the results of this study. Because the criteria for deciding on patients for receiving laparoscopic versus open resection were not provided by the NIS database, surgical indications might confound the results. Furthermore, several potential confounders were not collected by the NIS such as caner staging, clinical laboratory data, and lifestyle factors. Notably, clinical outcomes of laparoscopic colon surgery were suggested to be influenced by TNM stage [28] and disease stage [40]. Finally, the findings of this US NIS-based study should be confirmed by large-scale, longitudinal cohort studies of elderly colon and rectal cancer patients from different geographic regions.
Conclusion
For colon cancer patients aged 80 and older, laparoscopic resection had better short-term outcomes in terms of postoperative complication and in-hospital mortality than open resection. However, for rectal cancer patients ≥ 80 years, laparoscopic resection reduced postoperative complication but did not affect in-hospital mortality. Although the long-term survival effect of laparoscopic resection is unclear, laparoscopic resection results in better or similar short-term surgical outcomes in colon and rectal cancer patients aged 80 or over as compared to open resection. Hence, laparoscopic resection is feasible for elderly colon and rectal cancer patients.
References
World Health Organization (WHO) (2015) World report on ageing and health. https://apps.who.int/iris/handle/10665/186463
Lunenfeld B, Stratton P (2013) The clinical consequences of an ageing world and preventive strategies. Best Pract Res Clin Obstet Gynaecol 27:643–659
Jafari MD, Jafari F, Halabi WJ, Nguyen VQ, Pigazzi A, Carmichael JC, Mills SD, Stamos MJ (2014) Colorectal cancer resections in the aging us population: a trend toward decreasing rates and improved outcomes. JAMA Surg 149:557–564
Malvezzi M, Bertuccio P, Levi F, La Vecchia C, Negri E (2014) European cancer mortality predictions for the year 2014. Ann Oncol 25:1650–1656
Hori M, Matsuda T, Shibata A, Katanoda K, Sobue T, Nishimoto H, Japan Cancer Surveillance Research G (2015) Cancer incidence and incidence rates in Japan in 2009: a study of 32 population-based cancer registries for the Monitoring of Cancer Incidence in Japan (MCIJ) project. Jpn J Clin Oncol. 45:884–891
Arnold M, Sierra MS, Laversanne M, Soerjomataram I, Jemal A, Bray F (2017) Global patterns and trends in colorectal cancer incidence and mortality. Gut 66:683–691
Siegel R, Desantis C, Jemal A (2014) Colorectal cancer statistics, 2014. CA Cancer J Clin 64:104–117
Nakamura T, Sato T, Miura H, Ikeda A, Tsutsui A, Naito M, Ogura N, Watanabe M (2014) Feasibility and outcomes of surgical therapy in very elderly patients with colorectal cancer. Surg Laparosc Endosc Percutan Tech 24:85–88
Itatani Y, Kawada K, Sakai Y (2018) Treatment of elderly patients with colorectal cancer. Biomed Res Int 2018:2176056
Guillou PJ, Quirke P, Thorpe H, Walker J, Jayne DG, Smith AM, Heath RM, Brown JM, Group MCt (2005) Short-term endpoints of conventional versus laparoscopic-assisted surgery in patients with colorectal cancer (MRC CLASICC trial): multicentre, randomised controlled trial. Lancet 365:1718–1726
Neudecker J, Klein F, Bittner R, Carus T, Stroux A, Schwenk W, Trialists LI (2009) Short-term outcomes from a prospective randomized trial comparing laparoscopic and open surgery for colorectal cancer. Br J Surg 96:1458–1467
Bates AT, Divino C (2015) Laparoscopic surgery in the elderly: a review of the literature. Aging Dis 6:149–155
Villano AM, Zeymo A, Houlihan BK, Bayasi M, Al-Refaie WB, Chan KS (2019) Minimally Invasive Surgery for Colorectal Cancer: Hospital Type Drives Utilization and Outcomes. J Surg Res. https://doi.org/10.1016/j.jss.2019.07.102
Hatakeyama T, Nakanishi M, Murayama Y, Komatsu S, Shiozaki A, Kuriu Y, Ikoma H, Ichikawa D, Fujiwara H, Okamoto K, Ochiai T, Kokuba Y, Otsuji E (2013) Laparoscopic resection for colorectal cancer improves short-term outcomes in very elderly colorectal cancer patients. Surg Laparosc Endosc Percutan Technol 23:532–535
Kang T, Kim HO, Kim H, Chun HK, Han WK, Jung KU (2015) Age over 80 is a possible risk factor for postoperative morbidity after a laparoscopic resection of colorectal cancer. Ann Coloproctol 31:228–234
Grailey K, Markar SR, Karthikesalingam A, Aboud R, Ziprin P, Faiz O (2013) Laparoscopic versus open colorectal resection in the elderly population. Surg Endosc 27:19–30
Schiphorst AH, Pronk A, Borel Rinkes IH, Hamaker ME (2014) Representation of the elderly in trials of laparoscopic surgery for colorectal cancer. Colorectal Dis 16:976–983
Antoniou SA, Antoniou GA, Koch OO, Pointner R, Granderath FA (2015) Laparoscopic colorectal surgery confers lower mortality in the elderly: a systematic review and meta-analysis of 66,483 patients. Surg Endosc 29:322–333
Kalady MF, Sanchez JA, Manilich E, Hammel J, Casey G, Church JM (2009) Divergent oncogenic changes influence survival differences between colon and rectal adenocarcinomas. Dis Colon Rectum 52:1039–1045
Paschke S, Jafarov S, Staib L, Kreuser ED, Maulbecker-Armstrong C, Roitman M, Holm T, Harris CC, Link KH, Kornmann M (2018) Are colon and rectal cancer two different tumor entities? A proposal to abandon the term colorectal cancer. Int J Mol Sci. https://doi.org/10.3390/ijms19092577
Tamas K, Walenkamp AM, de Vries EG, van Vugt MA, Beets-Tan RG, van Etten B, de Groot DJ, Hospers GA (2015) Rectal and colon cancer: Not just a different anatomic site. Cancer Treat Rev 41:671–679
Doumouras AG, Tsao MW, Saleh F, Hong D (2016) A population-based comparison of 30-day readmission after surgery for colon and rectal cancer: How are they different? J Surg Oncol 114:354–360
Quan H, Sundararajan V, Halfon P, Fong A, Burnand B, Luthi JC, Saunders LD, Beck CA, Feasby TE, Ghali WA (2005) Coding algorithms for defining comorbidities in ICD-9-CM and ICD-10 administrative data. Med Care 43:1130–1139
Millan M, Merino S, Caro A, Feliu F, Escuder J, Francesch T (2015) Treatment of colorectal cancer in the elderly. World J Gastrointest Oncol 7:204–220
Siegel RL, Miller KD, Jemal A (2019) Cancer statistics, 2019. CA Cancer J Clin 69:7–34
Holmes AC, Riis AH, Erichsen R, Fedirko V, Ostenfeld EB, Vyberg M, Thorlacius-Ussing O, Lash TL (2017) Descriptive characteristics of colon and rectal cancer recurrence in a Danish population-based study. Acta Oncol 56:1111–1119
Kannan U, Reddy VS, Mukerji AN, Parithivel VS, Shah AK, Gilchrist BF, Farkas DT (2015) Laparoscopic vs open partial colectomy in elderly patients: Insights from the American College of Surgeons: National Surgical Quality Improvement Program database. World J Gastroenterol 21:12843–12850
Zhou X, Wang L, Shen W (2017) Laparoscopic surgery as a treatment option for elderly patients with colon cancer. J BUON 22:424–430
Hinoi T, Kawaguchi Y, Hattori M, Okajima M, Ohdan H, Yamamoto S, Hasegawa H, Horie H, Murata K, Yamaguchi S, Sugihara K, Watanabe M, Japan Society of Laparoscopic Colorectal S (2015) Laparoscopic versus open surgery for colorectal cancer in elderly patients: a multicenter matched case-control study. Ann Surg Oncol. 22:2040–2050
Ringressi MN, Boni L, Freschi G, Scaringi S, Indennitate G, Bartolini I, Bechi P, Taddei A (2018) Comparing laparoscopic surgery with open surgery for long-term outcomes in patients with stage I to III colon cancer. Surg Oncol 27:115–122
Zeng WG, Zhou ZX, Hou HR, Liang JW, Zhou HT, Wang Z, Zhang XM, Hu JJ (2015) Outcome of laparoscopic versus open resection for rectal cancer in elderly patients. J Surg Res 193:613–618
Volkel V, Draeger T, Schnitzbauer V, Gerken M, Benz S, Klinkhammer-Schalke M, Furst A (2019) Surgical treatment of rectal cancer patients aged 80 years and older: a German nationwide analysis comparing short- and long-term survival after laparoscopic and open tumor resection. Eur J Surg Oncol 45:1607–1612
Grosso G, Biondi A, Marventano S, Mistretta A, Calabrese G, Basile F (2012) Major postoperative complications and survival for colon cancer elderly patients. BMC Surg 12(Suppl 1):S20
Kirchhoff P, Clavien PA, Hahnloser D (2010) Complications in colorectal surgery: risk factors and preventive strategies. Patient Saf Surg 4:5
Kiran RP, Murray AC, Chiuzan C, Estrada D, Forde K (2015) Combined preoperative mechanical bowel preparation with oral antibiotics significantly reduces surgical site infection, anastomotic leak, and ileus after colorectal surgery. Ann Surg. 262:416–425 discussion 423–415
Opitz I, Gantert W, Giger U, Kocher T, Krahenbuhl L (2005) Bleeding remains a major complication during laparoscopic surgery: analysis of the SALTS database. Langenbecks Arch Surg 390:128–133
Wallace D, Walker K, Kuryba A, Finan P, Scott N, van der Meulen J (2014) Identifying patients at risk of emergency admission for colorectal cancer. Br J Cancer 111:577–580
Simorov A, Shaligram A, Shostrom V, Boilesen E, Thompson J, Oleynikov D (2012) Laparoscopic colon resection trends in utilization and rate of conversion to open procedure: a national database review of academic medical centers. Ann Surg 256:462–468
Berthelsen CL (2000) Evaluation of coding data quality of the HCUP National Inpatient Sample. Top Health Inf Manag 21:10–23
Ishii Y, Yahagi M, Ochiai H, Sako H, Amemiya R, Maeda H, Ogiri M, Kamiya N, Watanabe M (2019) Short-term and midterm outcomes of single-incision laparoscopic surgery for right-sided colon cancer. Asian J Endosc Surg 12:275–280
Acknowledgements
The authors would like to thank Convergence CT for English editing assistance of this manuscript.
Funding
None.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
Kuan-Chih Chung, Ko-Chao Lee, Hong-Hwa Chen, Kung-Chuan Cheng, Kuen-Lin Wu, and Ling-Chiao Song have no conflicts of interest to disclose.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Chung, KC., Lee, KC., Chen, HH. et al. Differential short-term outcomes of laparoscopic resection in colon and rectal cancer patients aged 80 and older: an analysis of Nationwide Inpatient Sample. Surg Endosc 35, 872–883 (2021). https://doi.org/10.1007/s00464-020-07459-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00464-020-07459-x