Abstract
Objective
A meta-analysis was performed to assess risks of intraoperative and postoperative urologic complications in laparoscopic radical hysterectomy (LRH) and abdominal radical hysterectomy (ARH).
Methods
We searched Pubmed, EMBASE, and Cochrane library for studies published up to December, 2018. Manual searches of related articles and relevant bibliographies of published studies were also performed. Two researchers independently performed data extraction. Inclusion criteria of studies were: (1) had information of perioperative complications, and (2) had at least ten patients per group.
Results
A total of 38 eligible clinical trials were collected. Intraoperative and postoperative urologic complications were reported by 34 studies and 35 studies, respectively. When all studies were pooled, odd ratios (OR) of LRH for the risk of intraoperative urologic complications compared to abdominal radical hysterectomy (ARH) was 1.40 [95% confidence interval (CI) 1.05–1.87]. The OR of LRH for postoperative complication risk compared to ARH was 1.35 [95% CI 1.01–1.80]. However, significant adverse effects of intraoperative urologic complications in LRH were not observed among articles published after 2012 (OR 1.12, 95% CI 0.77–1.62) in cumulative meta-analysis or subgroup analysis. The incidence of bladder injury was statistically higher than that of ureter injury (p = 0.001). In subgroup analysis, obesity and laparoscopic type (laparoscopic assisted vaginal radical hysterectomy) were associated with intraoperative urologic complications.
Conclusion
LRH is associated with significantly higher risk of intraoperative and postoperative urologic complications than abdominal radical hysterectomy.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Radical hysterectomy with bilateral pelvic lymph node dissection is the standard treatment for early uterine cervical cancer. Most of urologic complications that developed during surgery were associated with gynecologic field. The incidence of perioperative urologic complication is relatively higher in radical hysterectomy than that in other gynecologic surgeries. Intraoperative injuries of the bladder and the ureter as well as vesicovaginal and ureterovaginal fistulas in the postoperative period are important complications of radical hysterectomy [1]. Bladder injuries can occur during bladder dissection to obtain adequate vaginal resection margin. Bladder injuries are frequent urologic complications in radical hysterectomy. Incidence of bladder injuries during radical hysterectomy ranges from 0.4 to 3.7% [2]. Clinically, ureter injury is more important because of its general tendency to be unrecognized. On the other hand, bladder injuries can be easily recognized and repaired immediately. Ureter injuries occur between uterine arteries and bladder. Changes in surgical techniques that limit extreme dissection of ureter injury have reduced ureteral injuries for many years. However, ureteral injury is still a major complication of radical hysterectomy.
Radical hysterectomy can be performed using laparoscopic radical hysterectomy (LRH) or abdominal radical hysterectomy (ARH). LRH is an alternative to ARH because laparoscopic surgery is associated with less postoperative pain, shorter length of hospital stay, better cosmetic outcome, and faster recovery of bowel function compared to open surgery [3]. Although LRS has many advantages, it has not been widely used by gynecologic oncologists due to technical difficulties, long learning curve, and concerns of surgical complications.
Many studies have compared perioperative complications including urologic complications of patients treated by LRH with those of patients treated by ARH. Most of these studies have reported that there is no statistical significance in surgical complications including urologic complications between the two groups. Several studies have reported that LRH is associated with a low rate of perioperative complications [4,5,6,7]. However, the population examined was usually too small to definitively evaluate perioperative complications. A few meta-analysis [8, 9] have evaluated oncologic safety and effectiveness of LRH compared to those of LRH. However, they did not focus on urologic complications. The important step of technical skill in radical hysterectomy is unroofing of ureteral tunnel and wide dissection of periureteral tissue and bladder which is associated with perioperative urologic complication.
Thus, the objective of this study was to determine the risk of intraoperative and postoperative urologic complications in LRH compared to that in ARH through a meta-analysis.
Methods
Literature search
A comprehensive, systemic search for published studies was conducted using Pubmed, EMBASE, and Cochrane library up to December 2018. Predefined keywords used for the search were ‘laparoscopic radical hysterectomy’, ‘abdominal radical hysterectomy’ in combination with ‘urologic complication’, and ‘uterine cervical cancer or carcinoma’. We also scanned bibliographies of relevant articles to locate additional publications. Only articles written in English were included.
Selection criteria
We included comparative studies designed to assess intraoperative and postoperative complications of LRH and ARH in uterine cervical cancer. We also included laparoscopic radical parametrectomy [10] and laparoscopic radical trachelectomy [11] in addition to LRH. Robotic radical laparoscopy (RRH) was excluded. Review, editorials, letters, and meeting abstracts were excluded. Publications including fewer than 10 patients were also excluded. Three randomized controlled studies have been reported. Two of them were excluded since their patient numbers were less than ten. We excluded those studies without available data for perioperative complications. If data were duplicated, the larger study was selected in meta-analysis.
Data extraction
Two researchers independently evaluated the eligibility of all studies retrieved from the database based on predetermined criteria. Disagreements between evaluators were resolved by discussion. Of articles found in the three databases, duplicate articles and those that did not meet the selection criteria were excluded. We extracted the following data from the remaining studies: first author, journal name, year of publication, year enrolled, country where research was conducted, study design, study population, operation type, body mass index, and intraoperative and postoperative urologic complications. Intraoperative urologic complications included bladder injury, ureteral injury while postoperative urologic complications included ureterovaginal fistula, vesicovaginal fistula, ureteral stenosis, and urinary tract infection. Postoperative urinary retention and urinary incontinence were excluded.
Main and subgroup analyses
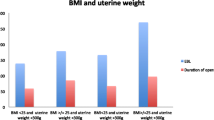
We investigated the association between laparoscopic radical hysterectomy and risk of urologic complication as a main analysis. We also performed subgroup analyses for published year, quality of study design, body mass index (BMI, kg/m2), country, and operation method [laparoscopic assisted radical vaginal hysterectomy (LARVH) vs. total laparoscopic radical hysterectomy (TLRH)]. Published years of articles were divided into two groups: before 2012 and after 2012. Matched, prospective cohort studies were categorized as high quality while retrospective studies were categorized as low quality in the current meta-analysis. We considered BMI > 24 as obese group and BMI < 24 as standard group. Countries were categorized as Asia, America, and Europe. LARVH involved opening the paravesical and pararectal space, resecting a vaginal cuff, ligating the cardinal ligament and the uterosacral ligament, and unroofing of the ureter.
Statistical analyses
Data for dichotomous variables were analyzed using odds ratio (OR). To compute pooled odds ratio with 95% CI, we used adjusted OR and 95% CI reported in each article whenever possible. We also carried out subgroup meta-regression analysis to assess the effect of subgroups and covariates such as published year, quality of study methodology, BMI, country, and operation method. We evaluated the possible heterogeneity in results across studies using Higgins I [12] to measure the percentage of total variation across studies. We considered an I2 value > 30% as indicative of substantial heterogeneity. We estimated a pooled OR with 95% CI using both fixed-effects [13] and random-effects models [14]. Fixed-effects model was utilized in the absence of significant heterogeneity while a random-effect model was used in the presence of significant heterogeneity. We evaluated publication bias of studies included in the final analysis using Begg’s funnel plot and Egger’s test. Meat-analyses were conducted using Stata MP version 15.0 software package (StatCorp, College Station, TX, USA).
Results
Literature search
We identified a total of 38 relevant studies published between 2001 and 2018 in the final analysis. Figure 1 shows a flow diagram of the process used to identify relevant studies. A total of 2705 articles were searched. We identified 322 articles from the three databases and bibliographies of relevant articles. After exclusion of 132 duplicate articles, the remaining 190 articles were screened by review according to their titles, abstracts, and publication types. Of these articles, 111 articles that did not meet the selection criteria were excluded. After reviewing the full text for the remaining 79 articles, we included 38 articles in the final analysis. The main reason for excluding 41 studies from the final review was due to no available data for urologic complication (N = 27). Other reasons included less than 10 patients (N = 4), comparison between robotic radical hysterectomy (RRH) vs. LRH or comparison between RRH and ARH (N = 5). Five articles were published in the same institution (N = 5). The largest study was selected for meta-analysis.
Intraoperative and postoperative complications were not described in four [6, 7, 11, 15] and three articles [4, 16, 17], respectively. Intraoperative and postoperative urologic complications were analyzed in 34 studies and 35 studies, respectively. We excluded one article in postoperative urinary complication due to publication bias and heterogeneity (I-squared 35.9%, p = 0.02) during meta-analysis.
Characteristics of the 38 studies included in the final analysis
Table 1 shows main characteristics of the 38 studies [4,5,6,7, 10, 11, 15,16,17,18,19,20,21,22,23,24,25,26,27,28,29,30,31,32,33,34,35,36,37,38,39,40,41,42,43,44,45,46] included in the final analysis. Their study design types were retrospective study (n = 25), matched case–control study (n = 10), prospective cohort study (n = 2), and RCT (n = 1). Locations of these studies were America (n = 9), Europe (n = 12), and Asia (n = 13). The enrollment period (year) of participants across studies ranged from 1991 to 2016.
We identified 2720 patients in LRH and 4084 patients in ARH (2582 patients in LRH vs. 3989 patients in ARH in intraoperative analysis, 2398 patients in LRH vs. 2367 patients in ARH in postoperative analysis). LARVH and TLRH were performed in 7 and 26 studies, respectively. Median or mean BMI was described in 24 studies. If BMD was greater than 24, the group was classified as obese (n = 10). If BMD was less than 24, then the group was classified as standard (n = 10). BMI was reported in 14 studies.
LRH and risk of urologic complications
Figures 2 and 3 show the effect of LRH on the risk of intraoperative and postoperative urologic complications in meta-analysis of 34 studies, respectively. Intraoperative complications were detected in 98 of 2,582 patients (bladder injury, n = 65; ureter injury, n = 33) who underwent LRH. The incidence of bladder injury was significantly higher than that of ureter injury (p = 0.001). In a fixed-effects meta-analysis of 34 studies including intraoperative urologic complications, the overall risk was increased in the laparoscopic group (OR 1.40; 95% CI 1.05–1.87, p = 0.022). In a fixed-effects meta-analysis of 34 studies including postoperative urologic complications, overall risk was increased (OR: 1.35; 95% CI 1.01–1.80, p = 0.039). There was no heterogeneity among studies of intraoperative urologic complications (I2 = 0.0%, p = 0.850) or among studies of postoperative complications (I2 = 0.0%, p = 0.763). No publication bias was observed in these selected studies. Results of assessment of publication bias showed symmetric distribution. All scattered hollow round points were symmetrical on both sides, indicating that the bias of data applied in this study was small (Fig. 4). Cumulative meta-analysis for intraoperative urologic complication of laparoscopic radical hysterectomy was performed. As shown in the cumulative meta-analysis plot (Fig. 5), the summary estimate for intraoperative complications began to be significantly higher in the laparoscopy group than that in the laparotomy group after inclusion of the study (2001) reported by Malur et al. [18]. The OR remained significantly higher in the laparoscopy group up to the study reported by Van De Lande et al. [33] in 2012. As time went on, the OR tended to decrease. The OR remained statistically insignificant after the study reported by Wright et al. [17] in 2012. The meta-regression showed a strong evidence of an association between published year and intraoperative urologic complication (p = 0.036, coefficient: − 0.084).
Intraoperative urologic complications of laparoscopic radical hysterectomy compared to abdominal radical hysterectomy in a fixed effect model of case–control studies. Forest plot showed intraoperative complication in 34 studies. No significant between-study heterogeneity was detected (I2 = 0%, p = 0.850) (OR 1.40; 95% CI 1.05–1.87, p = 0.022)
Postoperative urologic complications of laparoscopic radical hysterectomy compared to abdominal radical hysterectomy in a fixed effect model of case–control studies. Forest plot showed intraoperative complication in 34 studies. No significant between-study heterogeneity was detected (I2 = 0%, p = 0.763) (OR 1.35; 95% CI 1.01–1.80, p = 0.039)
Subgroup meta-analysis
Table 2 shows the effect of laparoscopy on intraoperative urologic complication in subgroup meta-analyses by published year, quality of study, BMI, country, and laparoscopic type. Significant harmful effects of intraoperative urologic complications in LRH were observed among articles published before 2012 (OR 2.0, 95% CI 1.24–3.23), but not in articles published after 2012 (OR 1.12, 95% CI 0.77–1.62) (Fig. 6). There was no significant association between postoperative urologic complications and published year (articles before 2012: OR 1.35; 95% CI 0.829–1.352; articles after 2012: OR 1.352; 95% CI 0.948–1.928).
There was no evidence for an association between the quality of study design and intraoperative urologic complications. Intraoperative urologic complications in LRH showed significant association with obese patients (OR 2.12, 95% CI 1.14–3.96), but not with patients having standard BMI (OR 1.08, 95% CI 0.61–1.92). In a fixed-effects meta-analysis of 26 studies including TLRH, the overall risk of intraoperative urologic complications was not increased (OR 1.28, 95% CI 0.90–1.83). However, the overall risk of intraoperative urologic complications was increased in 7 studies including LARVH (OR 1.67, 95% CI 1.01–2.77). Subgroup meta-analysis of 13 Asian studies (OR 1.12, 95% CI 0.72–1.74) and 9 American studies (OR 1.39, 95% CI 0.83–2.33) showed that the overall risk of intraoperative urologic complications was not increased. However, the overall risk of intraoperative urologic complications was increased in a subgroup meta-analysis of 12 European studies (OR 2.05, 95% CI 1.13–3.69). No significant association was observed for study quality, BMI, country, or laparoscopic type in a meta-regression analysis.
Discussion
LRH is thought to be associated with better recovery, smaller scar, and faster back to normal life than ARH [3]. Many comparative studies have reported that survival outcome and perioperative complications after LRH are comparable to those after ARH in patients with uterine cervical cancer. Most of these studies comparing LRH with ARH were retrospective studies or small sized RCT with limited data. Recently published large-scale RCT (LACC trial) [47] showed that minimally invasive radical hysterectomy including LRH was associated with lower rates of overall survival and disease-free survival compared to ARH. Unfortunately, perioperative complications were not described in LACC trial. The incidence of urologic complications during LRH is thought to be higher than that of any other gynecologic surgical procedure due to wide dissection of periureteral tissue and bladder, unroofing the ureter in the cardinal ligament, and the distorted pelvic anatomy caused by mass such as cervical cancer. Most of previous comparative studies revealed no statistical significance in urologic complications between LRH and ARH.
In 2012, we performed a meta-analysis of perioperative urologic complications related to LRH and reported that the risk of intraoperative urologic complications was higher in LRH group than that in ARH group based on data released through 2011 [48]. Although the incidence of intraoperative urologic complications was significantly higher in LRH, studies analyzed were performed at different time. The risk of intraoperative urologic complications in LRH had a tendency to decrease as time went by in cumulative meta-analysis. Laparoscopy continue to evolve. It could reduce complications due to technical changes and the development of instruments. The learning curve over time could also affect complication rate. The accumulation of surgical experience, the improvement of surgical skill, and the development of laparoscopic instruments such as advanced bipolar devices, Endo-GIA staplers, and Endo-Clips could reduce complications, thus affecting surgical outcomes as time went by. Thus, we performed meta-analysis again by including data released between 2012 and 2017. Our results showed that there was still an association between LRH and risk for intraoperative urologic complications. However, subgroup analysis showed that LRH among published articles after 2012 (OR 1.12, 95% CI 0.77–1.62) was not associated with a significant increased risk of intraoperative complications. There was a strong evidence for an association between published year and intraoperative urologic complications in meta-regression. Postoperative urologic complications were also higher in the LRH group, inconsistent with our previous study [48]. In subgroup analysis by published year, articles published after 2012 or before 2012 were not associated with high incidence of postoperative urologic complication in LRH. Difference became evident as the number of studies and patients included in the meta-analysis became larger.
There were two large comparative studies [49, 50] of perioperative complications about LRH versus ARH. Uppal et al. [49] reported perioperative complications of LRH and robotic radical hysterectomy (RRH) compared with ARH for 7180 cases of uterine cervical cancer from 2012 to 2015 using the National Inpatient Sample (NIS) from the Healthcare Cost and Utilization Project in USA. Perioperative complications were significantly lower for LRH and RRH. However, intraoperative urologic complication including ureter and bladder injury was higher in LRH and RRH than that in ARH (p = 0.027). Ratios of LRH and RRH in all study groups were 17.2% and 82.2%, respectively. They did not distinguish LRH from RRH. Thus, we excluded that study from the meta-analysis. Kim et al. [50] have reported that intraoperative complications of LRH have lower (OR 0.73; 95% CI 0.63–0.86) than ARH for 6,335 cases of uterine cervical cancer from 2011 to 2014 using the Korea Health Insurance Review and Assessment Service database. Intraoperative complications included vascular and intestinal injury in addition to ureter and bladder injury. Unfortunately, accurate assessment of urologic complications was difficult because the article [50] did not describe urinary complications that could be distinguished from other intraoperative complications.
Risks of bladder injuries are statistically higher than those of ureter injuries. In radical hysterectomy, ureter injuries usually occur during dissection of periureteral tissue to confirm ureter passage and find the uterine artery. The process of unroofing the ureter in the cardinal ligament, an important step in radical hysterectomy, plays a crucial role in inducing ureteral injury.
In the subgroup meta-analysis by country, results of European studies showed that the risk of urinary complications during surgery was significantly higher, although there was no significant difference between results of Asian and American studies. It is not easy to predict basic laparoscopic surgery technique. The habit of using chopsticks for Asian people and different surgical education systems in different countries might affect the outcome [51]. With regard to surgical approach, the incidence of intraoperative urologic complication rate was increased during LARVH. Vaginal route allows a precise dissection of vaginal cuff. In LARVH, after the uterine ligament was cut, the bladder and ureter are seen by traction of the uterus through vaginal route. This provides a theoretical background in which complications may be different due to differences in surgical methods. Obesity is a predisposing factor of perioperative urinary track complications in patients undergoing cancer surgery through laparoscopy [52, 53]. The current meta-analysis showed that intraoperative urologic complications were higher in patients who were relative overweight with LARVH, consistent with our previous study [48]. Our meta-analysis has several limitations. First, most studies involved were retrospective. They failed to provide the highest level of evidence. As a result, selective deflection and missing data could degrade the quality of study. A randomized clinical trial comparing LRH with ARH in patients with early stage uterine cervical cancer is needed. Results of such study will help determine the risk of perioperative urologic complications in LRH. Recently, RRH has been replacing LRH. One meta-analysis showed that RRH was superior to LRH in perioperative complication [54]. However, it focused on all intraoperative and postoperative complications related to surgery, not urologic complications. In the future, a study is needed to assess the risk of perioperative urologic complications of RRH and LRH. Second, we included only English language articles which might be a bias of our study. Exclusion of studies written in language other than English might have affected our outcomes. However, there have been few studies on this topic written in non-English languages. Third, we did not classify the incidence of urologic complications according to the type of radical hysterectomy. Although most patients underwent type III radical hysterectomy, some patients underwent type II radical hysterectomy. The incidence of urologic complications might be higher in advanced uterine cervical cancer and type III radical hysterectomy. Bladder dysfunction and urinary incontinence were excluded from the analysis of postoperative complication because many articles did not describe them as it was uncommon to evaluate these complications objectively in postoperative care. This might have led to biased results in analysis of postoperative urologic complications. Stage of the disease and diabetes that could act as a predisposing factor of the urinary track injury during radical hysterectomy [55] was not evaluated either.
Despite these limitations, our meta-analysis demonstrated that there was an association between LRH and risk for intraoperative and postoperative urologic complications. We also confirmed that intraoperative urologic complication decreased after 2012 in subgroup analysis and meta-regression. Of the 38 studies included in this meta-analysis, two studies [21, 38] reported that intraoperative urologic complications were significantly higher in the LRH group. Thus, publication bias is minimal. It was confirmed by funnel plot. Although this meta-analysis was based on results of retrospective studies, it included more than 4,000 patients with a comprehensive review of the available literature. Our findings should be verified by large-scale prospective cohort studies or randomized controlled trials in the future.
References
Hwang JH, Lim MC, Joung JY, Seo SS, Kang S, Seo HK et al (2012) Urologic complications of laparoscopic radical hysterectomy and lymphadenectomy. Int Urogynecol J 23(11):1605–1611
Limon Luque LM, Alva Trujillo HN, Delgado UJ (1995) Urologic lesions in gynecologic and uro-gynecologic surgery. Two years of hospital experience. Ginecol Obstet Mex 63:410–413
Summitt RL Jr, Stovall TG, Steege JF, Lipscomb GH (1998) A multicenter randomized comparison of laparoscopically assisted vaginal hysterectomy and abdominal hysterectomy in abdominal hysterectomy candidates. Obstet Gynecol 92(3):321–326
Pahisa J, Martinez-Roman S, Torne A, Fuste P, Alonso I, Lejarcegui JA et al (2010) Comparative study of laparoscopically assisted radical vaginal hysterectomy and open Wertheim-Meigs in patients with early-stage cervical cancer: eleven years of experience. Int J Gynecol Cancer 20(1):173–178
Lee EJ, Kang H, Kim DH (2011) A comparative study of laparoscopic radical hysterectomy with radical abdominal hysterectomy for early-stage cervical cancer: a long-term follow-up study. Eur J Obstet Gynecol Reprod Biol 156(1):83–86
Sharma R, Bailey J, Anderson R, Murdoch J (2006) Laparoscopically assisted radical vaginal hysterectomy (Coelio-Schauta): a comparison with open Wertheim/Meigs hysterectomy. Int J Gynecol Cancer 16(5):1927–1932
Darai E, Ballester M, Chereau E, Coutant C, Rouzier R, Wafo E (2010) Laparoscopic versus laparotomic radical en bloc hysterectomy and colorectal resection for endometriosis. Surg Endosc 24(12):3060–3067
Zhao Y, Hang B, Xiong GW, Zhang XW (2017) Laparoscopic radical hysterectomy in early stage cervical cancer: a systematic review and meta-analysis. J Laparoendosc Adv Surg Technol A 27(11):1132–1144
Park DA, Yun JE, Kim SW, Lee SH (2017) Surgical and clinical safety and effectiveness of robot-assisted laparoscopic hysterectomy compared to conventional laparoscopy and laparotomy for cervical cancer: a systematic review and meta-analysis. Eur J Surg Oncol 43(6):994–1002
Jiang H, Qu L, Liu X, Hua K, Xu H, Guo SW (2013) A comparison of laparoscopic and abdominal radical parametrectomy for cervical or vaginal apex carcinoma and stage II endometrial cancer after hysterectomy. JSLS 17(2):249–262
Vieira MA, Rendon GJ, Munsell M, Echeverri L, Frumovitz M, Schmeler KM et al (2015) Radical trachelectomy in early-stage cervical cancer: a comparison of laparotomy and minimally invasive surgery. Gynecol Oncol 138(3):585–589
Higgins JP, Thompson SG (2002) Quantifying heterogeneity in a meta-analysis. Stat Med 21(11):1539–1558
Woolf B (1955) On estimating the relation between blood group and disease. Ann Hum Genet 19(4):251–253
DerSimonian R, Laird N (1986) Meta-analysis in clinical trials. Control Clin Trials 7(3):177–188
Bogani G, Cromi A, Serati M, Di Naro E, Uccella S, Donadello N et al (2014) Predictors of postoperative morbidity after laparoscopic versus open radical hysterectomy plus external beam radiotherapy: a propensity-matched comparison. J Surg Oncol 110(7):893–898
Sobiczewski P, Bidzinski M, Derlatka P, Panek G, Danska-Bidzinska A, Gmyrek L et al (2009) Early cervical cancer managed by laparoscopy and conventional surgery: comparison of treatment results. Int J Gynecol Cancer 19(8):1390–1395
Wright JD, Herzog TJ, Neugut AI, Burke WM, Lu YS, Lewin SN et al (2012) Comparative effectiveness of minimally invasive and abdominal radical hysterectomy for cervical cancer. Gynecol Oncol 127(1):11–17
Malur S, Possover M, Schneider A (2001) Laparoscopically assisted radical vaginal vs radical abdominal hysterectomy type II in patients with cervical cancer. Surg Endosc 15(3):289–292
Lee C (2002) Comparison of laparoscopic and conventional surgery in the treatment of early cervical cancer. J Am Assoc Gynecol Laparosc 9(4):481–487
Abu-Rustum NR, Gemignani ML, Moore K, Sonoda Y, Venkatraman E, Brown C et al (2003) Total laparoscopic radical hysterectomy with pelvic lymphadenectomy using the argon-beam coagulator: pilot data and comparison to laparotomy. Gynecol Oncol 91(2):402–409
Steed H, Rosen B, Murphy J, Laframboise S, De Petrillo D, Covens A (2004) A comparison of laparascopic-assisted radical vaginal hysterectomy and radical abdominal hysterectomy in the treatment of cervical cancer. Gynecol Oncol 93(3):588–593
Jackson KS, Das N, Naik R, Lopes AD, Godfrey KA, Hatem MH et al (2004) Laparoscopically assisted radical vaginal hysterectomy vs radical abdominal hysterectomy for cervical cancer: a match controlled study. Gynecol Oncol 95(3):655–661
Zakashansky K, Chuang L, Gretz H, Nagarsheth NP, Rahaman J, Nezhat FR (2007) A case-controlled study of total laparoscopic radical hysterectomy with pelvic lymphadenectomy versus radical abdominal hysterectomy in a fellowship training program. Int J Gynecol Cancer 17(5):1075–1082
Uccella S, Laterza R, Ciravolo G, Volpi E, Franchi M, Zefiro F et al (2007) A comparison of urinary complications following total laparoscopic radical hysterectomy and laparoscopic pelvic lymphadenectomy to open abdominal surgery. Gynecol Oncol 107(1 Suppl 1):S147–S149
Li G, Yan X, Shang H, Wang G, Chen L, Han Y (2007) A comparison of laparoscopic radical hysterectomy and pelvic lymphadenectomy and laparotomy in the treatment of Ib-IIa cervical cancer. Gynecol Oncol 105(1):176–180
Ghezzi F, Cromi A, Ciravolo G, Volpi E, Uccella S, Rampinelli F et al (2007) Surgicopathologic outcome of laparoscopic versus open radical hysterectomy. Gynecol Oncol 106(3):502–506
Frumovitz M, dos Reis R, Sun CC, Milam MR, Bevers MW, Brown J et al (2007) Comparison of total laparoscopic and abdominal radical hysterectomy for patients with early-stage cervical cancer. Obstet Gynecol 110(1):96–102
Malzoni M, Tinelli R, Cosentino F, Fusco A, Malzoni C (2009) Total laparoscopic radical hysterectomy versus abdominal radical hysterectomy with lymphadenectomy in patients with early cervical cancer: our experience. Ann Surg Oncol 16(5):1316–1323
Estape R, Lambrou N, Diaz R, Estape E, Dunkin N, Rivera A (2009) A case matched analysis of robotic radical hysterectomy with lymphadenectomy compared with laparoscopy and laparotomy. Gynecol Oncol 113(3):357–361
Papacharalabous E, Tailor A, Madhuri T, Giannopoulos T, Butler-Manuel S (2008) Early experience of laparoscopically assisted radical vaginal hysterectomy (Coelio-Schauta) versus abdominal radical hysterectomy for early stage cervical cancer. Gynecol Surg 6(2):113–117
Soliman PT, Frumovitz M, Sun CC, Dos Reis R, Schmeler KM, Nick AM et al (2011) Radical hysterectomy: a comparison of surgical approaches after adoption of robotic surgery in gynecologic oncology. Gynecol Oncol 123(2):333–336
Nam JH, Park JY, Kim DY, Kim JH, Kim YM, Kim YT (2012) Laparoscopic versus open radical hysterectomy in early-stage cervical cancer: long-term survival outcomes in a matched cohort study. Ann Oncol 23(4):903–911
van de Lande J, von Mensdorff-Pouilly S, Lettinga RG, Piek JM, Verheijen RH (2012) Open versus laparoscopic pelvic lymph node dissection in early stage cervical cancer: no difference in surgical or disease outcome. Int J Gynecol Cancer 22(1):107–114
Campos LS, Limberger LF, Stein AT, Kalil AN (2013) Postoperative pain and perioperative outcomes after laparoscopic radical hysterectomy and abdominal radical hysterectomy in patients with early cervical cancer: a randomised controlled trial. Trials 14:293
Ditto A, Martinelli F, Bogani G, Gasparri ML, Di Donato V, Zanaboni F et al (2015) Implementation of laparoscopic approach for type B radical hysterectomy: a comparison with open surgical operations. Eur J Surg Oncol 41(1):34–39
Laterza RM, Salvatore S, Ghezzi F, Serati M, Umek W, Koelbl H (2015) Urinary and anal dysfunction after laparoscopic versus laparotomic radical hysterectomy. Eur J Obstet Gynecol Reprod Biol 194:11–16
Lu Q, Zhang Z, Liu C (2015) Urologic complications after laparoscopic radical hysterectomy and abdominal radical hysterectomy in patients with early cervical cancer: a prospective randomized study. J Minim Invasive Gynecol 22(6S):S88
Suh DH, Cho HY, Kim K, No JH, Kim YB (2015) Matched-case comparisons in a single institution to determine critical points for inexperienced surgeons' successful performances of laparoscopic radical hysterectomy versus abdominal radical hysterectomy in stage IA2-IIA cervical cancer. PLoS ONE 10(6):e0131170
Cai J, Yang L, Dong W, Wang H, Xiong Z, Wang Z (2016) Retrospective comparison of laparoscopic versus open radical hysterectomy after neoadjuvant chemotherapy for locally advanced cervical cancer. Int J Gynaecol Obstet 132(1):29–33
Mendivil AA, Rettenmaier MA, Abaid LN, Brown JV 3rd, Micha JP, Lopez KL et al (2016) Survival rate comparisons amongst cervical cancer patients treated with an open, robotic-assisted or laparoscopic radical hysterectomy: a five year experience. Surg Oncol 25(1):66–71
Zhang S, Ma L, Meng QW, Zhou D, Moyiding T (2017) Comparison of laparoscopic-assisted radical vaginal hysterectomy and abdominal radical hysterectomy in patients with early stage cervical cancer: a retrospective study. Medicine (Baltimore) 96(36):e8005
Corrado G, Vizza E, Legge F, Pedone Anchora L, Sperduti I, Fagotti A et al (2018) Comparison of different surgical approaches for stage IB1 cervical cancer patients: a multi-institution study and a review of the literature. Int J Gynecol Cancer 28(5):1020–1028
Guo J, Yang L, Cai J, Xu L, Min J, Shen Y et al (2018) Laparoscopic procedure compared with open radical hysterectomy with pelvic lymphadenectomy in early cervical cancer: a retrospective study. Onco Targets Ther 11:5903–5908
Kong TW, Chang SJ, Lee J, Paek J, Ryu HS (2014) Comparison of laparoscopic versus abdominal radical hysterectomy for FIGO stage IB and IIA cervical cancer with tumor diameter of 3 cm or greater. Int J Gynecol Cancer 24(2):280–288
Wang W, Chu HJ, Shang CL, Gong X, Liu TY, Zhao YH et al (2016) Long-term oncological outcomes after laparoscopic versus abdominal radical hysterectomy in stage IA2 to IIA2 cervical cancer: a matched cohort study. Int J Gynecol Cancer 26(7):1264–1273
Zhu T, Chen X, Zhu J, Chen Y, Yu A, Chen L et al (2017) Surgical and pathological outcomes of laparoscopic versus abdominal radical hysterectomy with pelvic lymphadenectomy and/or para-aortic lymph node sampling for bulky early-stage cervical cancer. Int J Gynecol Cancer 27(6):1222–1227
Ramirez PT, Frumovitz M, Pareja R, Lopez A, Vieira M, Ribeiro R et al (2018) Minimally invasive versus abdominal radical hysterectomy for cervical cancer. N Engl J Med 379(20):1895–1904
Hwang JH (2012) Urologic complication in laparoscopic radical hysterectomy: meta-analysis of 20 studies. Eur J Cancer 48(17):3177–3185
Uppal S, Rebecca Liu J, Kevin Reynolds R, Rice LW, Spencer RJ (2019) Trends and comparative effectiveness of inpatient radical hysterectomy for cervical cancer in the United States (2012–2015). Gynecol Oncol 152(1):133–138
Kim JH, Kim K, Park SJ, Lee JY, Kim K, Lim MC et al (2018) Comparative effectiveness of abdominal versus laparoscopic radical hysterectomy for cervical cancer in the postdissemination era. Cancer Res Treat. 51:788
Madan AK, Frantzides CT, Park WC, Tebbit CL, Kumari NV, O'Leary PJ (2005) Predicting baseline laparoscopic surgery skills. Surg Endosc 19(1):101–104
Kim MG, Yook JH, Kim KC, Kim TH, Kim HS, Kim BS (2011) Influence of obesity on early surgical outcomes of laparoscopic-assisted gastrectomy in gastric cancer. Surg Laparosc Endosc Percutan Technol 21(3):151–154
Karahasanoglu T, Hamzaoglu I, Baca B, Aytac E, Kirbiyik E (2011) Impact of increased body mass index on laparoscopic surgery for rectal cancer. Eur Surg Res 46(2):87–93
Jin YM, Liu SS, Chen J, Chen YN, Ren CC (2018) Robotic radical hysterectomy is superior to laparoscopic radical hysterectomy and open radical hysterectomy in the treatment of cervical cancer. PLoS ONE 13(3):e0193033
Likic IS, Kadija S, Ladjevic NG, Stefanovic A, Jeremic K, Petkovic S et al (2008) Analysis of urologic complications after radical hysterectomy. Am J Obstet Gynecol 199(6):644
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Disclosures
Jong Ha Hwang and Bo Wook Kim have no conflicts of interest or financial ties to disclose.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Hwang, J.H., Kim, B.W. Laparoscopic radical hysterectomy has higher risk of perioperative urologic complication than abdominal radical hysterectomy: a meta-analysis of 38 studies. Surg Endosc 34, 1509–1521 (2020). https://doi.org/10.1007/s00464-020-07366-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00464-020-07366-1