Abstract
Background
There are a variety of surgical approaches for the management of right-sided colonic neoplasms. To date, no method has been shown superior in terms of surgical and perioperative outcomes. This meta-analysis compared open (ORH), laparoscopic-assisted (LRH), total laparoscopic (TLRH), and robotic right hemicolectomy (RRH) to assess surgical outcomes and perioperative morbidity and mortality.
Study design
We conducted an electronic systematic search using PubMed, EMBASE, and Web of Science that compared RRH, TLRH, LRH, and ORH. Forty-eight studies met the inclusion criteria: 5 randomized controlled trials, 25 retrospective, and 18 prospective studies totalling 5652 patients were included.
Results
The overall complication rate was similar between RRH and TLRH (RR 1.0; Crl 0.66–1.5). The anastomotic leak rate was higher in LRH and ORH compared to RRH (RR 1.9; Crl 0.99–3.6 and RR 1.2; Crl 0.55–2.6, respectively), whereas it was lower in TLRH compared to RRH (RR 0.88 Crl 0.41–1.9). The risk of reoperation was significantly higher in ORH compared to TLRH (RR 3.3; Crl 1.3–8.0). Operative time was similar in RRH compared to LRH (RR − 27.0; Crl − 61.0 to 5.9), and to TLRH (RR − 24.0; Crl − 70.0 to 21.0). The hospital stay was significantly longer in LRH compared to RRH (RR 3.7; Crl 0.7–6.7).
Conclusion
The surgical management of right-sided colonic disease is evolving. This network meta-analysis observed that short-term outcomes following RRH and TLRH were superior to standard LRH and ORH. The adoption of more advanced minimally invasive techniques can be costly and have associated learning phases, but will ultimately improve patient outcomes.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Colorectal is the third most common malignancy affecting the population worldwide. Surgery remains the cornerstone of treatment. In contemporary times, the optimal surgical approach for right resections is often debated [1]. Increasingly, there is focus on the incidence of postoperative complications, quality of life, and oncological outcomes [2].
Laparoscopic colonic resection was first introduced in 1991 [3]. Currently, laparoscopy is the most common utilized approach across colorectal surgery, as it is associated with reduced complications, shorter length of hospital stay, due to earlier mobilization, and return to normal bowel function, with comparable oncological outcomes [4]. Nevertheless the standardization of the technique, particularly pertaining to the ileocolic anastomosis (extracorporeal [laparoscopic-assisted right hemicolectomy (LRH)] versus intracorporeal [total laparoscopic hemicolectomy (TLRH)]), has not been internationally agreed [5]. This represents a considerable confounder when comparing operative techniques across the literature [6].
Recent developments, most notably the introduction of the robotic platforms (da Vinci robot Intuitive Surgical Inc, Sunnyvale, CA, USA) [7], have increased focus on minimally invasive approaches to both colonic and rectal dissection and anastomosis. Robotic technology is proposed to overcome ergonomical issues associated with laparoscopic surgery especially regarding intracorporeal anastomosis. However, this assumption has not been supported by strong data in the literature so far [8].
To date, the gold standard for right hemicolectomy in most centers is LRH when feasible [9]. This network meta-analysis aims to compare outcomes between RRH and TLRH and RRH, and ORH. In addition, it also intends to compare ORH to TLRH, which have not been directly compared to date.
Materials and methods
Search strategy
A systematic review was performed according to the guidelines from the preferred reporting items for systematic reviews and meta-analyses checklist (PRISMA-NMA) [10]. Institutional review board approval was not required for this type of study.
We conducted an electronic systematic search using PubMed, EMBASE, and Web of Science. The last date of search was the March 1, 2018. We searched for papers published in English using the following search strategy: (“laparoscopic right hemicolectomy”[tiab] OR “laparoscopic hand-assisted right hemicolectomy”[tiab] OR “laparoscopic colectomy”[tiab]) AND (“robotic right hemicolectomy”[tiab] OR “telerobotic right hemicolectomy “[tiab] OR “robot-assisted right hemicolectomy “[tiab]); (“laparoscopic right hemicolectomy”[tiab] OR “laparoscopic hand-assisted right hemicolectomy”[tiab] OR “laparoscopic colectomy”[tiab]) AND (“laparotomic right hemicolectomy”[tiab] OR “open right hemicolectomy”[tiab] OR “open colectomy”[tiab]); (“laparotomic right hemicolectomy”[tiab] OR “open right hemicolectomy”[tiab] OR “open colectomy”[tiab]) AND (“robotic right hemicolectomy”[tiab] OR “telerobotic right hemicolectomy“[tiab] OR “robot-assisted right hemicolectomy”[tiab]).
All titles were initially evaluated and suitable abstracts were extracted. Besides, each of the eligible publication reference list was also screened for further potential articles. The study protocol was registered at PROSPERO (International prospective register of systematic reviews), accessible at http://www.crd.york.ac.uk/prospero/ (Registration Number: CRD42018091308).
Inclusion/exclusion criteria
As suggested by Stroup et al. [11] only randomized controlled trials (RCTs) or controlled clinical trials (non-RCTs) were considered for this analysis. To be included in the analysis, (a) studies comparing surgical outcomes for either ORH and LRH or TLRH and LRH or RRH and LRH for either malignant or benign diseases; (b) articles written in English. (c) articles have the longest follow-up or the largest sample size when two or more studies were reported by the same institution.
Studies were excluded if (a) they were not written in English; (b) the methodology was not clearly reported; (c) the surgical technique was not clearly reported (e.g., intra or extracorporeal anastomosis).
Data extraction
The following data were retrieved from the selected publications: author, year of publication, country, study design, number of patients, proportion of males and females, age, body mass index (BMI), diagnosis, intraoperative, and early postoperative outcomes. All data were entered independently by two investigators (ER, AA) and compared only at the end of the reviewing process to reduce the selection bias. A third author (LB) eventually reviewed the database. Duplicates were erased and the discrepancies clarified.
Quality assessment
For observational studies, the study quality was assessed by using the Newcastle–Ottawa Scale (NOS), which is a star rating system [12]. Any disagreements on the NOS score of the studies were resolved by discussion between the authors.
The methodological quality of the selected RCTs was appraised by using the Cochrane risk of bias tool [13]. Trials were graded as follows: L = low risk, H = high risk, U = unclear risk. Thus, each RCT graded as having low, moderate, or high risk of bias Disagreements was solved by discussion. The quality of all included studies is depicted in Tables 1, 2, and 3.
Outcomes of interest
The following outcomes were used to assess and compare ORH, LRH, TLRH, and RRH.
Primary outcomes: Early postoperative complications (overall complications, anastomotic leak, surgical site infection, reoperation, and 30-day mortality), and 60-day readmission rates.
Secondary outcomes: Operative and perioperative data (operative time, conversion rate, estimated blood loss, blood transfusion, hospital stay, and lymph node harvest), and RRH cost analysis.
Statistical analysis
In addition to systematic review, we performed fully Bayesian arm-based random effect network meta-analysis, in particular mixed treatment comparison. Briefly, the network meta-analysis simultaneously synthesizes data from all available trials within a consistent network and combines direct evidence (comparison of treatments within head-to-head trials) with indirect evidence (comparison of treatments across trials against a common comparator) [14].
We preferred the Bayesian approach because that takes into account all sources of variation and reflects these variations in the pooled result. Furthermore, the Bayesian approach can provide more accurate estimates for small samples. An ordinary consistency model was adopted with the binomial/log model as likelihood was used. Non-informative priors distribution included in this analysis were normal (0, 1000) for log of relative risk (RR) and relative effects, gamma (0.001, 0.001) distribution for random effect precision. Pairwise comparison was performed using unrelated mean effects model [15]. To provide valid indirect inferences, we considered the transitivity assumption (i.e., studies comparing different sets of interventions needed to be sufficiently similar). To assess transitivity, we generated descriptive statistics and we compared the distributions of baseline participant characteristics across studies and treatment comparisons. We assumed a common heterogeneity parameter across the various treatment comparisons. To evaluate statistical heterogeneity, we calculated between-trial variances and I2-index, assuming a common estimate for the heterogeneity variance across the different comparisons. I2-index value of 25% was defined as low heterogeneity, 50% as moderate heterogeneity, and 75% as high heterogeneity [16]. To assess local inconsistencies, we used the node-splitting method [17].
The inference was performed using mean and relative 95% credible intervals (Crl), based on draws from marginal posterior distribution in Monte Carlo Markov chain, simulating 350,000 iterations after a burn-in period of 30,000 iterations. We consider the estimated parameter significance when its 95% Crl encompasses null hypothesis value. Sensitivity analysis regarding the choice of prior distribution of random effect precision was considered.
Model convergence was assessed by analyzing history, running means density, and Brooks–Gelman–Rubin diagnostic plots In addition, autocorrelation plots were assessed to detect the presence of autocorrelation in the chains [18]. We plotted rank probabilities against the possible ranks for all competing treatments. All statistical analyses were carried out using Jags [18] and R-Cran [19].
Cost analysis was performed using Stata Data Analysis and Statistical Software (Ver. 12 StataCorp LLC USA). Outcome data were reported standardized mean differences (SMD) and 95% Crl were estimated using random effects models. SMD was calculated as SMD = (new treatment improvement − standard treatment improvement)/pooled standard deviation. In our analysis, the new treatment was robotic right hemicolectomy, compared to laparoscopic right hemicolectomy as the standard treatment. An SMD equal to zero denotes equivalent effects between robotic and laparoscopic resection. For continuous data, the mean and standard deviation (SD) were estimated the median, range, and the size of the sample using validated techniques (if needed) [20].
Review of network geometry
We investigated the spectrum of comparisons among the different surgical techniques for right hemicolectomy within the network of published studies. We appraised the geometry of the networks for each outcome separately and provided network graphs with nodes reflecting the competing surgical approaches and two nodes linked together by an edge, if at least one study compared the two corresponding surgical techniques. We analyzed the connection between surgical approaches (i.e., those compared head-to-head in the selected studies and those, which were only connected indirectly by one “common comparators” and the amount of evidence informing each comparison).
Results
Literature search and study characteristics
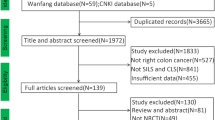
Four thousand three hundred twenty-one publications were found by using the aforementioned search criteria. After removing duplicates, 973 publications were further reviewed. Further screening found that 48 studies [8, 21,22,23,24,25,26,27,28,29,30,31,32,33,34,35,36,37,38,39,40,41,42,43,44,45,46,47,48,49,50,51,52,53,54,55,56,57,58,59,60,61,62,63,64,65,66,67] met the inclusion criteria. The selection process is reported in Fig. 1. Among the included studies, 43 were non-RCTs [8, 21,22,23,24,25,26,27, 30,31,32,33,34,35,36,37,38,39,40,41, 43,44,45, 47,48,49,50,51,52,53,54,55,56,57,58,59,60,61,62,63,64,65,66] (25 were retrospective [8, 24,25,26,27, 30, 32, 34, 37,38,39, 41, 43,44,45, 47,48,49,50, 52, 56,57,58, 62, 66] and 18 prospective [21,22,23, 31, 33, 35, 36, 40, 51, 53,54,55, 59,60,61, 63,64,65]), and 5 RCTs [28, 29, 42, 46, 67]. Forty-seven studies reported the primary outcomes (Fig. 2). Of the 4 studies [30, 39, 63, 67] included in the RRH cost analysis, Park et al. was excluded from the assessment of the other outcomes because the laparoscopic group did not differentiate whether laparoscopic surgery was LRH or TLRH [67]. At this study level, we tried out to ensure transitivity by applying narrow inclusion criteria and making populations as similar as possible within and across treatment comparisons.
Patient characteristics
Five thousand six hundred fifty-two patients were included in the selected studies. Of these, 2847 (50.3%) were treated with LRH, 1324 (23.4%) with TLRH, 1067 (18.8%) with ORH, and 414 (7.5%) with RRH, respectively. The mean age was 66.6 years. The gender was clarified in 5480 patients: 2807 patients (51.2%) were males and 2673 (48.8%) females. Body mass index (BMI) was investigated in 37 studies; the median BMI was 25.5. The vast majority had surgery for malignancy (87.2%). Three thousand nine hundred sixty-three patients were graded according to the American Society Anaesthesiologists (ASA) classification: 2669 patients (67.3%) were classified ASA I–II and 1294 (32.7%) ASA III–IV. Characteristics of all patients according to the surgical treatment are listed in Table 4; notably, the potential measured effect modifiers were distributed similarly across the available direct comparisons. This helps to understand that transitivity assumption should hold.
Primary Outcomes
Overall complication rate
Pooled network analysis showed that the risk of overall complication was similar between RRH and TLRH (RR 1.0; Crl 0.6–1.5), higher in LRH versus RRH, though not statistically significant (RR 1.3; Crl 0.9–1.9), and significantly higher in ORH compared to RRH (RR 1.9; Crl 1.2–2.9). Furthermore, indirect comparison showed that the RR of overall complication was significantly higher in ORH compared to TLRH (RR 1.9; Crl 1.3–2.7) (Fig. 3A). A rank plot illustrating empirical probabilities for overall complication in each surgical approach ranked 1st through 4th (left to right) is depicted in Fig. 4A. The global heterogeneity was low, I2 = 19.8%. Comparing RRH to ORH, the direct inconsistency was 0.3 (Crl 0.0–1.7) and the indirect inconsistency 0.5 (Crl 0.3–0.8) (p value = 0.6). Comparing RRH to TLRH, the direct inconsistency was 0.7 (Crl 0.2–1.9) and the indirect inconsistency 1.1 (Crl 0.6–1.7) (p value = 0.4). League table is depicted in Fig. 5A.
Anastomotic leak
Pooled network analysis did not show any difference regarding the rate of anastomotic leak. The point estimation showed that anastomotic leak rate was higher in LRH and ORH compared to RRH (RR 1.9; Crl 0.99–3.6 and RR 1.2; Crl 0.55–2.6; respectively). In contrast, the point estimation of RR was lower in TLRH compared to RRH (RR 0.88 Crl 0.41–1.9). Furthermore, the indirect comparison showed that the point estimation of RR was higher in ORH compared to TLRH (RR 1.3; Crl 1.3–2.6) (Fig. 3B). A rank plot illustrating empirical probabilities for anastomotic leak in each surgical approach ranked 1st through 4th (left to right) is depicted in Fig. 4B. The global heterogeneity was low, I2 = 0.0%. Comparing RRH to ORH, the direct inconsistency was 0.7 (Crl 0.0–8.9) and the indirect inconsistency 0.8 (Crl 0.3–1.8) (p value = 0.9). Comparing RRH to TLRH, the direct inconsistency was 0.2 (Crl 0.0–2.2) and the indirect inconsistency 1.1 (Crl 0.4–2.9) (p value = 0.2). League table is depicted in Fig. 5B.
Surgical site infection
Pooled network analysis showed that the RR of surgical site infection (SSI) was similar between RRH and LRH (RR 1.9; Crl 0.95–4.1), statistically higher in ORH compared to RRH (RR 2.3; Crl 1.2–5.5), and comparable between RRH and TLRH (RR 1.1; Crl 0.51–2.5). Furthermore, indirect comparison showed that the risk of SSI was significantly higher in ORH compared to TLRH (RR 2.1; Crl 1.2–3.6) (Fig. 3C). A rank plot illustrating empirical probabilities for overall complication in each surgical approach ranked 1st through 4th (left to right) is depicted in Fig. 4C. The global heterogeneity was low, I2 = 11.1%. Comparing RRH to TLRH; the direct inconsistency was 0.3 (Crl 0.0–3.3); and the indirect inconsistency 1.4 (Crl 0.5–3.8) (p value = 0.3). League table is depicted in Fig. 5C.
Reoperation
Pooled network analysis showed that the RR of reoperation was similar between RRH and LRH and between RRH and ORH (RR 0.88; Crl 0.32–2.5 and RR 1.1; Crl 0.31–3.7; respectively). Moreover, the point estimation of reoperation risk was lower in TLRH compared to RRH even though it was not statistically significant (RR 3.3; Crl 0.1–1.0). Last, the indirect comparison showed that the risk of reoperation was significantly higher in ORH compared to TLRH (RR 3.3; Crl 1.3–8.0) (Fig. 3D). A rank plot illustrating empirical probabilities for reoperation in each surgical approach ranked 1st through 4th (left to right) is depicted in Fig. 4D. The global heterogeneity was low, I2 = 0.0%. Comparing RRH to TLRH, the direct inconsistency was 2.1 (Crl 0.0–1.6) and the indirect inconsistency 1.1 (Crl 0.1–9.6) (p value = 0.2). League table is depicted in Fig. 5D.
30-Day mortality
Pooled network analysis did not show any statistically difference in RR when comparing 30-day mortality in RRH versus LRH (RR 1.2; Crl 0.5–2.8), ORH (RR 1.1; Crl 0.4–3.0), and TLRH group (RR − 0.7; Crl 0.3–1.9). Indirect comparison noted that the 30-day mortality rate in TLRH was similar compared to ORH (RR 1.5; Crl 0.7–3.2) (Fig. 3E). A rank plot illustrating empirical probabilities for reoperation in each surgical approach ranked 1st through 4th (left to right) is depicted in Fig. 4E. The global heterogeneity was low, I2 = 2.3%. Comparing RRH to ORH, the direct inconsistency was 0.3 (Crl 0.0–2.4) and the indirect inconsistency 1.3 (Crl 0.6–2.4) (p value = 0.2). Comparing RRH to TLRH, the direct inconsistency was 0.6 (Crl 0.1–2.8) and the indirect inconsistency 1.1 (Crl 0.5–2.1) (p value = 0.5).
60-Day readmission
Pooled network analysis did not show any statistical difference in RR when comparing the 60-day readmission among the all the four surgical procedures. The risk of 60-day readmission reoperation was similar between RRH and LRH (RR 1.2; Crl 0.4–3.4) and between RRH and ORH (RR 0.6; Crl 0.1–2.8). The point estimation of 60-days readmission risk was lower in TLRH compared to RRH but not statistically different (RR 0.5; Crl 0.1–2.0). Indirect comparison showed that the risk of 60-day readmission was comparable between TLRH and ORH (RR 1.2; Crl 0.3–3.8) (Fig. 3F). A rank plot illustrating empirical probabilities for reoperation in each surgical approach ranked 1st through 4th (left to right) is depicted in Fig. 4F. The global heterogeneity was low, I2 = 5.6%. League table is depicted in Fig. 5F.
Secondary outcomes
Operative time
Pooled network analysis did not show any difference comparing the operative time in RRH to LRH (RR − 27.0; Crl − 61.0 to 5.9), ORH (RR − 4.1; Crl − 52.0 to 44.0), and TLRH group (RR − 24.0; Crl − 70.0 to 21.0). Interestingly, indirect comparison observed that the operative time in ORH was longer compare to TLRH though not statistically significant (RR 20.0; Crl − 29.0 to 70.0). The global heterogeneity was high, I2 = 90%.
Conversion rate
Pooled network analysis showed comparable conversion rates between RRH and TLRH (RR 1.7; Crl 0.53–5.9). The global heterogeneity was low, I2 = 23%.
Estimated blood loss and transfusion rates
Pooled network analysis showed that the estimated blood loos (EBL) was significantly lower in RRH compared to ORH (RR 42.0; Crl 10.0–72.0), in contrast it was comparable between RRH and LRH (RR 9.8; Crl − 12.0 to 31.0), and RRH and TLRH (RR 0.4; Crl − 28.0 to 28.0). Last, the indirect comparison showed that the EBL was significantly higher in ORH compared TLRH (RR 41.0; Crl 11.0–72.0). The global heterogeneity was high, I2 = 89%.
There was a statistically higher rates of blood transfusion for LRH patients when compared to RRH group (RR 3.1; Crl 1.1–13.0) and in ORH compared to RRH (RR 3.7; Crl 1.1–16.0). There was no statistical difference between RRH and TLRH group (RR 2.5; Crl 0.7–10.0). Indirect comparison showed that the blood transfusion between TLRH and ORH group was similar (RR 1.5; Crl 0.6–3.8). The global heterogeneity was low, I2 = 0.0%.
Hospital stay
Network analysis noted that hospital stay was significantly longer in LRH compared to RRH (RR 3.7; Crl 0.7–6.7) and in ORH compared to RRH (RR 6.7; Crl 2.9–10.0). Conversely, the hospital stay was similar comparing RRH and TLRH (RR 2.9; Crl − 0.7 to 6.5). Last, the indirect comparison showed that the hospital stay was significantly longer in ORH compared to TLRH (RR 3.8; Crl 0.5–7.0). The global heterogeneity was high, I2 = 80%.
Lymph node harvest
Pooled network analysis did not show any significant difference comparing the harvested lymph nodes in RRH to LRH (RR 1.8; Crl − 5.7 to 2.0), ORH (RR − 2.8; Crl − 7.3 to 1.7), and TLRH group (RR − 2.2; Crl − 6.5 to 2.1) Moreover, the indirect comparison showed that the harvested lymph nodes were similar in TLRH and ORH group (RR − 0.6; Crl − 3.9 to 2.7). The global heterogeneity was high, I2 = 75%.
Cost analysis
Four studies [30, 39, 63, 67] reported total healthcare cost differences between laparoscopic and robotic right hemicolectomy. The median healthcare cost ($) for laparoscopic versus robotic right hemicolectomy was $10,508 and $12,413, respectively. All four studies were included in the pooled analysis. The SMD between laparoscopic and RRH was 0.60 (95% Crl 0.33–0.86; p = 0.001; I2 = 65%) in favor of robotic colectomy (more expensive) (Fig. 6).
Discussion
This review and network meta-analysis compared the four surgical approaches available for right hemicolectomy. Overall, it observed that both RRH and TLRH have considerable benefits regarding perioperative outcomes compared to LRH and ORH. The risk of postoperative complications following TLRH was significantly lower compared to LRH and ORH, and similar to RRH. Interestingly, anastomotic leak rate was lowest in the TLRH group compared to all other surgical approaches. Again, surgical site infection rate was similar between RRH and TLRH, statistically better than compared to ORH. There was no major difference in rates of reoperation, 30-day mortality, or 60-day readmission rates across the surgical approaches.
In recent years, there has been increased enthusiasm for robotic approaches for all colon and rectal surgery. There is growing evidence to show that it has superiority in pelvic surgery, especially for urological and gynecological indications [68]. Xiong et al. noted that robotic resection reduced positivity in circumferential resection margins, and the incidence of erectile dysfunction following rectal surgery [69]. However, there remains issues over cost implications and its widespread availability.
There has also been debate over its routine use in right-sided colonic surgery. Main opponents cite that it is associated with longer operative times, and overall increased healthcare cost, with limited data to date on its superiority. This network meta-analysis observed that RRH has similar length of operative time, but is associated with increased overall hospital costs. However, RRH patients had reduced length of hospital stay, and this may ultimately mitigate some initial expenditures of acquiring a robotic platform. There remains a lack of substantial evidence on its impact on quality of life postoperatively. Potential reasons for RRH having initial longer operative times may relate to learning-curve of adapting to a new operative approach and issues surrounding the efficient setting up (docking) of the robot [70, 71].
D2 lymphadenectomy remains the gold standard in oncological resection of the right colon [72]. Though some have advocated complete mesocolon excision and the need for open resectional surgery to ensure satisfactory clearance, there remains debate over its impact on improved long-term oncological outcomes [73]. This review did not observe any difference in lymph node yields across the four surgical modalities. If extended lymphadenopathy is shown to have survival benefits, improved surgical technology will likely evolve further to ensure minimal invasive approaches are achievable. The superiority of a minimal invasive approach when compared open surgery in terms of blood loss, patient recovery, and return to function is well established and further supported by this study.
We acknowledge that this review does have some limitations relating to possible publication bias due to exclusion of non-English articles, the sample size, and heterogeneity of some of the studies included. In addition, the reason for why each patient had a particular surgical approach is not reported and may represent some selection bias.
No evidence for significant inconsistency was found using the node-splitting, but caution is required given the scarcity of studies for most of the outcomes. According to Cochrane guidance, we did not analyze publication bias because there were less than ten studies for each comparison, thus publication bias cannot be excluded [74]. The imprecision must be considered for most of the primary outcomes because 95% Crl encompasses the null hypothesis value.
The confidence interval crosses null value or includes values favoring either treatment. The inclusion of observational study could be considered a study limitation; however, excluding observational studies in systematic reviews a priori is inappropriate and internally inconsistent with an evidence-based approach [75].
The confidence in the estimates was assessed using CINeMA and emerged to range from moderate to very low primarily due to the quality of the included studies [76]. Regarding the interpretation of the treatment ranking, caution is needed considering the confidence level. In fact, the treatment ranking does not consider the magnitude of differences in effects between treatments and therefore chance may explain any apparent difference between treatments. Therefore, surgeons should choose the most appropriate surgical approach evaluating the treatment ranking, costs, and their own expertise.
There remains a disparity in the current literature when reporting surgical and postoperative outcomes and comparing surgical techniques. In addition, there are limited data on surgical approaches and impact to quality of life and function. This study is the first systematic review and network meta-analysis comparing all four surgical approaches for right hemicolectomy. Using network meta-analytical techniques, we were able to synthesize data from numerous studies reporting different interventions and therefore rank the treatments according to our studied outcomes.
In conclusion, the surgical management of right-sided colonic disease is evolving. This network meta-analysis observed that short-term outcomes following RRH and TLRH were superior to standard LRH and ORH. The adoption of more advanced minimally invasive techniques can be costly and have associated learning phases, but will ultimately improve patient outcomes.
References
Lin JS, Piper MA, Perdue LA et al (2016) Screening for colorectal cancer: updated evidence report and systematic review for the US preventive services task force. JAMA 315:2576–2594
van Oostendorp S, Elfrink A, Borstlap W et al (2017) Intracorporeal versus extracorporeal anastomosis in right hemicolectomy: a systematic review and meta-analysis. Surg Endosc 31:64–77
Fowler DL, White SA (1991) Laparoscopy-assisted sigmoid resection. Surg Laparosc Endosc 1:183–188
Schiphorst AH, Verweij NM, Pronk A et al (2015) Non-surgical complications after laparoscopic and open surgery for colorectal cancer—a systematic review of randomised controlled trials. Eur J Surg Oncol 41:1118–1127
Cirocchi R, Trastulli S, Farinella E et al (2013) Intracorporeal versus extracorporeal anastomosis during laparoscopic right hemicolectomy - systematic review and meta-analysis. Surg Oncol 22:1–13
Arezzo A, Passera R, Ferri V et al (2015) Laparoscopic right colectomy reduces short-term mortality and morbidity. Results of a systematic review and meta-analysis. Int J Colorectal Dis 30:1457–1472
Weber PA, Merola S, Wasielewski A et al (2002) Telerobotic-assisted laparoscopic right and sigmoid colectomies for benign disease. Dis Colon Rectum 45:1689–1694; discussion 1695–1686
Trastulli S, Coratti A, Guarino S et al (2015) Robotic right colectomy with intracorporeal anastomosis compared with laparoscopic right colectomy with extracorporeal and intracorporeal anastomosis: a retrospective multicentre study. Surg Endosc 29:1512–1521
Ohtani H, Tamamori Y, Arimoto Y et al (2012) A meta-analysis of the short- and long-term results of randomized controlled trials that compared laparoscopy-assisted and open colectomy for colon cancer. J Cancer 3:49–57
Liberati A, Altman DG, Tetzlaff J et al (2009) The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate healthcare interventions: explanation and elaboration. BMJ 339:b2700
Stroup DF, Berlin JA, Morton SC et al (2000) Meta-analysis of observational studies in epidemiology: a proposal for reporting. Meta-analysis of Observational Studies in Epidemiology (MOOSE) group. JAMA 283:2008–2012
Wells GA, Shea B, ‘Connell DO, Peterson J, Welch V, Losos M et al (2015) The Newcastle-Ottawa Scale (NOS) for assessing the quality of nonrandomised studies in the meta-analysis. http://www.ohri.ca/programs/clinical_epidemiology/oxford.asp
Higgins JP, Altman DG, Gotzsche PC et al (2011) The Cochrane Collaboration’s tool for assessing risk of bias in randomised trials. BMJ 343:d5928
Mills EJ, Thorlund K, Ioannidis JP (2013) Demystifying trial networks and network meta-analysis. Bmj 346:f2914
Dias S, Sutton AJ, Ades AE et al (2013) Evidence synthesis for decision making 2: a generalized linear modeling framework for pairwise and network meta-analysis of randomized controlled trials. Med Decis Making 33:607–617
Higgins JP, Thompson SG, Deeks JJ et al (2003) Measuring inconsistency in meta-analyses. Bmj 327:557–560
Dias S, Welton NJ, Caldwell DM et al (2010) Checking consistency in mixed treatment comparison meta-analysis. Stat Med 29:932–944
Plummer M (2003) JAGS: a program for analysis of Bayesian graphical models using Gibbs sampling. In: Proceedings of the 3rd international workshop on distributed statistical computing, Vienna, 20–22 March 2003
R Core Team (2018) R: a language and environment for statistical computing. R Foundation for Statistical Computing, Vienna. http://www.R-project.org/. Accessed 5 April 2018
Hozo SP, Djulbegovic B, Hozo I (2005) Estimating the mean and variance from the median, range, and the size of a sample. BMC Med Res Methodol 5:13
Bokey EL, Moore JW, Chapuis PH et al (1996) Morbidity and mortality following laparoscopic-assisted right hemicolectomy for cancer. Dis Colon Rectum 39:S24–S28
Leung KL, Meng WC, Lee JF et al (1999) Laparoscopic-assisted resection of right-sided colonic carcinoma: a case-control study. J Surg Oncol 71:97–100
Lezoche E, Feliciotti F, Paganini AM et al (2002) Laparoscopic vs open hemicolectomy for colon cancer. Surg Endosc 16:596–602
Baker RP, Titu LV, Hartley JE et al (2004) A case-control study of laparoscopic right hemicolectomy vs. open right hemicolectomy. Dis Colon Rectum 47:1675–1679
Zheng MH, Feng B, Lu AG et al (2005) Laparoscopic versus open right hemicolectomy with curative intent for colon carcinoma. World J Gastroenterol 11:323–326
Tong DK, Law WL (2007) Laparoscopic versus open right hemicolectomy for carcinoma of the colon. JSLS 11:76–80
Lohsiriwat V, Lohsiriwat D, Chinswangwatanakul V et al (2007) Comparison of short-term outcomes between laparoscopically-assisted vs. transverse-incision open right hemicolectomy for right-sided colon cancer: a retrospective study. World J Surg Oncol 5:49
Chung CC, Ng DC, Tsang WW et al (2007) Hand-assisted laparoscopic versus open right colectomy: a randomized controlled trial. Ann Surg 246:728–733
Braga M, Frasson M, Vignali A et al (2007) Open right colectomy is still effective compared to laparoscopy: results of a randomized trial. Ann Surg 246:1010–1014; discussion 1014–1015
Rawlings AL, Woodland JH, Vegunta RK et al (2007) Robotic versus laparoscopic colectomy. Surg Endosc 21:1701–1708
Tan WS, Chew MH, Ooi BS et al (2009) Laparoscopic versus open right hemicolectomy: a comparison of short-term outcomes. Int J Colorectal Dis 24:1333–1339
Nakamura T, Onozato W, Mitomi H et al (2009) Retrospective, matched case-control study comparing the oncologic outcomes between laparoscopic surgery and open surgery in patients with right-sided colon cancer. Surg Today 39:1040–1045
Hellan M, Anderson C, Pigazzi A (2009) Extracorporeal versus intracorporeal anastomosis for laparoscopic right hemicolectomy. Jsls 13:312–317
Abdel-Halim MR, Moore HM, Cohen P et al (2010) Impact of laparoscopic right hemicolectomy for colon cancer. Ann R Coll Surg Engl 92:211–217
Vogel JD, Lian L, Kalady MF et al (2011) Hand-assisted laparoscopic right colectomy: how does it compare to conventional laparoscopy? J Am Coll Surg 212:367–372
Scatizzi M, Kroning KC, Borrelli A et al (2010) Extracorporeal versus intracorporeal anastomosis after laparoscopic right colectomy for cancer: a case-control study. World J Surg 34:2902–2908
Chaves JA, Idoate CP, Fons JB et al (2011) A case-control study of extracorporeal versus intracorporeal anastomosis in patients subjected to right laparoscopic hemicolectomy. Cir Esp 89:24–30
Fabozzi M, Allieta R, Brachet Contul R et al (2010) Comparison of short- and medium-term results between laparoscopically assisted and totally laparoscopic right hemicolectomy: a case-control study. Surg Endosc 24:2085–2091
deSouza AL, Prasad LM, Park JJ et al (2010) Robotic assistance in right hemicolectomy: is there a role? Dis Colon Rectum 53:1000–1006
Khan JS, Hemandas AK, Flashman KG et al (2011) Clinical outcome of laparoscopic and open colectomy for right colonic carcinoma. Ann R Coll Surg Engl 93:603–607
Papaconstantinou HT, Sharp N, Thomas JS (2011) Single-incision laparoscopic right colectomy: a case-matched comparison with standard laparoscopic and hand-assisted laparoscopic techniques. J Am Coll Surg 213:72–80; discussion 80–72
Li JC, Leung KL, Ng SS et al (2012) Laparoscopic-assisted versus open resection of right-sided colonic cancer—a prospective randomized controlled trial. Int J Colorectal Dis 27:95–102
Tanis E, van Geloven AA, Bemelman WA et al (2012) A comparison of short-term outcome after laparoscopic, transverse, and midline right-sided colectomy. Int J Colorectal Dis 27:797–802
Kwon JW, Kim BS, Park HC et al (2012) Surgical treatment of complicated right colonic diverticulitis: laparoscopic versus open surgery. Surg Endosc 26:2926–2930
Roscio F, Bertoglio C, De Luca A et al (2012) Totally laparoscopic versus laparoscopic assisted right colectomy for cancer. Int J Surg 10:290–295
Ng LW, Tung LM, Cheung HY et al (2012) Hand-assisted laparoscopic versus total laparoscopic right colectomy: a randomized controlled trial. Colorectal Dis 14:e612–e617
Anania G, Santini M, Scagliarini L et al (2012) A totally mini-invasive approach for colorectal laparoscopic surgery. World J Gastroenterol 18:3869–3874
Erguner I, Aytac E, Baca B et al (2013) Total laparoscopic approach for the treatment of right colon cancer: a technical critique. Asian J Surg 36:58–63
Deutsch GB, Sathyanarayana SA, Gunabushanam V et al (2012) Robotic vs. laparoscopic colorectal surgery: an institutional experience. Surg Endosc 26:956–963
Shin JY (2012) Comparison of short-term surgical outcomes between a robotic colectomy and a laparoscopic colectomy during early experience. J Korean Soc Coloproctol 28:19–26
Marchesi F, Pinna F, Percalli L et al (2013) Totally laparoscopic right colectomy: theoretical and practical advantages over the laparo-assisted approach. J Laparoendosc Adv Surg Tech A 23:418–424
Lee KH, Ho J, Akmal Y et al (2013) Short- and long-term outcomes of intracorporeal versus extracorporeal ileocolic anastomosis in laparoscopic right hemicolectomy for colon cancer. Surg Endosc 27:1986–1990
Magistro C, Lernia SD, Ferrari G et al (2013) Totally laparoscopic versus laparoscopic-assisted right colectomy for colon cancer: is there any advantage in short-term outcomes? A prospective comparative assessment in our center. Surg Endosc 27:2613–2618
Casillas MA Jr, Leichtle SW, Wahl WL et al (2014) Improved perioperative and short-term outcomes of robotic versus conventional laparoscopic colorectal operations. Am J Surg 208:33–40
Morpurgo E, Contardo T, Molaro R et al (2013) Robotic-assisted intracorporeal anastomosis versus extracorporeal anastomosis in laparoscopic right hemicolectomy for cancer: a case control study. J Laparoendosc Adv Surg Tech A 23:414–417
Han DP, Lu AG, Feng H et al (2014) Long-term outcome of laparoscopic-assisted right-hemicolectomy with D3 lymphadenectomy versus open surgery for colon carcinoma. Surg Today 44:868–874
Bae SU, Park JS, Choi YJ et al (2014) The role of hand-assisted laparoscopic surgery in a right hemicolectomy for right-sided colon cancer. Ann Coloproctol 30:11–17
Vergis AS, Steigerwald SN, Bhojani FD et al (2015) Laparoscopic right hemicolectomy with intracorporeal versus extracorporeal anastamosis: a comparison of short-term outcomes. Can J Surg 58:63–68
Milone M, Elmore U, Di Salvo E et al (2015) Intracorporeal versus extracorporeal anastomosis. Results from a multicentre comparative study on 512 right-sided colorectal cancers. Surg Endosc 29:2314–2320
de’Angelis N, Alghamdi S, Renda A et al (2015) Initial experience of robotic versus laparoscopic colectomy for transverse colon cancer: a matched case-control study. World J Surg Oncol 13:295
Shapiro R, Keler U, Segev L et al (2016) Laparoscopic right hemicolectomy with intracorporeal anastomosis: short- and long-term benefits in comparison with extracorporeal anastomosis. Surg Endosc 30:3823–3829
Hanna MH, Hwang GS, Phelan MJ et al (2016) Laparoscopic right hemicolectomy: short- and long-term outcomes of intracorporeal versus extracorporeal anastomosis. Surg Endosc 30:3933–3942
Kang J, Park YA, Baik SH et al (2016) A comparison of open, laparoscopic, and robotic surgery in the treatment of right-sided colon cancer. Surg Laparosc Endosc Percutan Tech 26:497–502
Biondi A, Santocchi P, Pennestri F et al (2017) Totally laparoscopic right colectomy versus laparoscopically assisted right colectomy: a propensity score analysis. Surg Endosc 31:5275–5282
Martinek L, You K, Giuratrabocchetta S et al (2018) Does laparoscopic intracorporeal ileocolic anastomosis decreases surgical site infection rate? A propensity score-matched cohort study. Int J Colorectal Dis 33:291–298
Lujan HJ, Plasencia G, Rivera BX et al (2018) Advantages of robotic right colectomy with intracorporeal anastomosis. Surg Laparosc Endosc Percutan Tech 28:36–41
Park JS, Choi GS, Park SY et al (2012) Randomized clinical trial of robot-assisted versus standard laparoscopic right colectomy. Br J Surg 99:1219–1226
Ahmed K, Khan MS, Vats A et al (2009) Current status of robotic assisted pelvic surgery and future developments. Int J Surg 7:431–440
Xiong B, Ma L, Huang W et al (2015) Robotic versus laparoscopic total mesorectal excision for rectal cancer: a meta-analysis of eight studies. J Gastrointest Surg 19:516–526
Xu H, Li J, Sun Y et al (2014) Robotic versus laparoscopic right colectomy: a meta-analysis. World J Surg Oncol 12:274
Kim HJ, Choi GS, Park JS et al (2014) Multidimensional analysis of the learning curve for robotic total mesorectal excision for rectal cancer: lessons from a single surgeon’s experience. Dis Colon Rectum 57:1066–1074
Vogel JD, Eskicioglu C, Weiser MR et al (2017) The American Society of Colon and Rectal Surgeons Clinical Practice Guidelines for the treatment of colon cancer. Dis Colon Rectum 60:999–1017
Spinoglio G, Marano A, Bianchi PP et al (2016) Robotic right colectomy with modified complete mesocolic excision: long-term oncologic outcomes. Ann Surg Oncol 23:684–691
Higgins JPT, Green S (2011) Cochrane handbook for systematic reviews of interventions version 5.1.0 [updated March 2011]. The Cochrane Collaboration. http://www.cochrane-handbook.org
Shrier I, Boivin JF, Steele RJ et al (2007) Should meta-analyses of interventions include observational studies in addition to randomized controlled trials? A critical examination of underlying principles. Am J Epidemiol 166:1203–1209
Salanti G, Del Giovane C, Chaimani A et al (2014) Evaluating the quality of evidence from a network meta-analysis. PLoS ONE 9:e99682
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Disclosures
Drs. Emanuele Rausa, Michael E. Kelly, Emanuele Asti, Alberto Aiolfi, Gianluca Bonitta, and Luigi Bonavina have no conflicts of interest or financial ties to disclose.
Rights and permissions
About this article
Cite this article
Rausa, E., Kelly, M.E., Asti, E. et al. Right hemicolectomy: a network meta-analysis comparing open, laparoscopic-assisted, total laparoscopic, and robotic approach. Surg Endosc 33, 1020–1032 (2019). https://doi.org/10.1007/s00464-018-6592-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00464-018-6592-3