Abstract
Introduction
Diagnostic laparoscopy (DL) is an increasingly used modality when approaching penetrating abdominal trauma (PAT). Trauma surgeons can utilize this minimally invasive technique to quickly assess for injury in hemodynamically stable patients. DL with a confirmed injury can be repaired through therapeutic laparoscopy (TL) or conversion to exploratory laparotomy (EL). This study analyzes the use of laparoscopy as a first-line therapy for hemodynamically stable patients with PAT.
Methods
Data were reviewed of patients presenting with PAT between December 2006 and September 2016. A retrospective analysis was conducted to analyze demographics, baseline presentations, treatment protocols and outcomes.
Results
A total of 56 patients with PAT were initially treated with laparoscopy. Injuries included stab wounds (n = 48) and gunshot wounds (n = 8). Patients were divided into three groups: DL, DL to TL, and DL to EL. Ten patients (17.9%) required conversion to laparotomy (DL to EL). Of the 46 patients who did not require conversion, 33 patients (71.7%) underwent DL, while 13 patients (28.3%) required TL (DL to TL). There were no differences in postoperative complication rates between the groups (p = 0.565). The mean lengths of hospital stay for DL, DL to TL, and DL to EL were 3.1, 2.7, and 8.1 days, respectively (p = 0.038). No missed injuries or mortalities occurred in any of the groups.
Conclusion
Laparoscopy can be utilized for hemodynamically stable patients with PAT. DL can be converted to TL in the hands of a skilled laparoscopist. In this study, we analyze the use of DL over a 10-year period in patients who presented to our level 1 trauma center with PAT. We also provide a comprehensive review of literature to create clear definitions, and to clarify a systematic stepwise approach of how to effectively perform DL and TL. This study adds to the body of literature supporting the role of laparoscopy in PAT, and advances the discussion regarding management.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
The evaluation and management of penetrating abdominal trauma (PAT) has greatly improved over the past several decades. Exploratory laparotomy (EL) has been traditionally viewed as the gold standard for evaluating PAT. However, as laparoscopy has become the standard of care in other surgical fields, its utility in trauma has been increasingly investigated.
In the 1960s, Shaftan first challenged the idea of mandated laparotomies for abdominal trauma with his term of ‘selective conservatism,’ as half of his patients with PAT did not require operative repair [1]. In recent review, surgical exploration in the setting of PAT has been associated with non-therapeutic laparotomy rates of up to 61% [2]. When approaching patients with PAT, laparoscopy has therefore been explored as a means of screening, diagnosis, and therapy. Laparoscopy in trauma was initially criticized due to the increased risk of missed injuries, particularly hollow viscus injuries. As both laparoscopic experience and surgical technology have advanced, missed injury rates have decreased from 13% to as low as 0.12%, a rate which does not differ from its open counterpart [3,4,5]. In a recent meta-analysis, the use of laparoscopy in trauma has led to an avoidance of non-therapeutic laparotomy in 45.6% of patients [2]. This prevents patients from being exposed to the unnecessary 33.3% morbidity rate and 5% mortality rate associated with non-therapeutic laparotomy [2, 6,7,8].
In addition to being accurate in screening peritoneal violation and diagnosing intra-abdominal injury, laparoscopy in trauma has proven to be efficacious in conversion to therapeutic laparoscopy (TL) [4, 5, 7, 9,10,11,12,13]. A clear definition of TL has not been well established in current literature. Certain studies reference what they consider to be a therapeutic maneuver, while other studies omit this information. We agree to define TL as cited by Koto et al. as “laparoscopic management of intra-abdominal injuries (more than observation or hemostatic agent application).” [5] Furthermore, certain studies describe therapeutic procedures as being performed fully laparoscopically (fully TL—FTL), while others utilize an laparoscopic assisted approach (LAA) [3, 9, 10, 14, 15]. The fully laparoscopic intervention is performed completely intracorporeally, whereas the LAA employs a therapeutic maneuver that is performed extracorporeally. As such, we recommend future studies utilize the above definition of TL and clarify the distinction between FTL and LAA.
In this study, we aim to analyze the safety and efficacy of diagnostic laparoscopy (DL) utilized over a 10-year period in patients who presented to our Level 1 trauma center with PAT. We also provide a comprehensive review of literature to create clear definitions, and to clarify a systematic stepwise approach of how to effectively perform DL and TL.
Materials and methods
This is a retrospective study of patients who presented to an inner city level 1 trauma center. Data were reviewed from all adult patients who presented between December 2006 and September 2016 with PAT. This project was submitted to the Institutional Review Board, and upon evaluation was granted exemption, as this was a retrospective chart review.
Our chart review included 333 patients with PAT. Cases of patients who were hemodynamically unstable, patients under 12 years of age, patients with organ evisceration on presentation, or patients who underwent immediate laparotomy were excluded. Fifty-six patients met criteria and underwent initial laparoscopic evaluation.
Patients in this study were divided into three groups: DL, DL with conversion to TL (DL to TL), or DL with conversion to EL (DL to EL). DL was defined as a non-therapeutic procedure wherein no injuries were identified or the identified injuries did not require repair. TL was defined as laparoscopic repair of intra-abdominal injury, more than simple evacuation of blood clot, mobilization of viscera, or application of hemostatic agent.
Analysis was performed to interpret patient demographics, baseline presentations, treatment protocols and outcomes which included postoperative complications, missed injuries, need for return to the operating room (OR), mortality rates, and length of hospital stay (LOS).
Demographics and baseline characteristics were summarized descriptively by mean and by percentage calculations for categorical variables. The Kruskal–Wallis test and Fischer’s exact test were used for comparisons. P values < 0.05 were considered statistically significant.
Results
A total of 56 patients with PAT underwent initial laparoscopic evaluation in the OR (Fig. 1). The mean age of our patient population was 40 years (range 16–66 years). The mean body mass index (BMI) was 26.7 (range 17–38). The mean Glascow Coma Score (GCS) upon presentation was 14.6 (range 8–15). All of the patients included in this study were hemodynamically stable upon initial evaluation (Table 1). Stab wounds to the abdomen accounted for 48 patients (85.7%). Gunshot wounds to the abdomen accounted for the remaining eight patients (14.3%) (Table 2).
Out of the 56 patients, 10 patients (17.9%) required conversion to laparotomy (DL to EL). Of the 46 patients who did not require conversion, 33 patients (71.7%) underwent DL. TL (DL to TL) was performed in 13 patients (28.3%). All TL was performed fully laparoscopically. No interventions were performed with an LAA. A non-therapeutic laparotomy was avoided in 58.9% of our patients. This was calculated as described by Hajibandeh et al. [2], by dividing the number of negative laparoscopies (n = 33) by the total number of laparoscopies (n = 56).
The Injury Severity Score (ISS) and the Penetrating Abdominal Trauma Index (PATI) were systems used to compare groups in our study. The ISS and PATI scores were lowest in the DL group (ISS mean 7.0, PATI mean 1.1). The ISS and PATI scores were higher in both groups requiring therapeutic interventions—the DL to TL group (ISS mean 11.0, PATI mean 2.7) and DL to EL group (ISS mean 13.3, PATI mean 3.8).
The most common reason for conversion from DL to EL was complexity of visceral injury. Other reasons for conversion included extensive bleeding, which could not be controlled laparoscopically, and poor visibility of the injury. In the DL to TL group, therapeutic maneuvers were performed to repair injuries to the liver, spleen, diaphragm, colon, small bowel, and mesentery. The DL to EL group included repairs to the liver, bladder, kidney, diaphragm, colon, and small bowel (Table 3).
There were no mortalities in any of the three groups, and no missed injuries occurred. Three patients suffered from postoperative complications, one of which required take back to the OR (Table 4). One patient in the DL group developed a postoperative ileus requiring an extended period of nothing by mouth. Another patient in the DL group developed hospital-acquired pneumonia requiring prolonged intravenous antibiotic therapy. In the EL group, one patient developed a postoperative intra-abdominal abscess. This required take back to the OR, where an anastomotic leak was found at the site of colon resection.
The mean LOS was significantly shorter in the groups managed without laparotomy. The DL group mean LOS was 3.1 days, while the DL to TL group mean LOS was 2.7 days. The mean LOS was greatest for the DL to EL group at 8.1 days (Table 4). All patients were discharged home.
Discussion
Since its first description in the 1920s by Dr. A. Rendle Short, laparoscopy in trauma has become an increasingly utilized technique when approaching both blunt and penetrating abdominal injury [16]. As both surgeon experience and surgical technology have evolved with time, so has the type of laparoscopy performed. Laparoscopy outside of trauma has become standard of care in many common surgical procedures. As such, the modern day trauma surgeon has been exposed to a vast array and breadth of laparoscopy during their general surgical training. With its original use intended as a screening modality, practice has now transformed laparoscopy into both a diagnostic and therapeutic modality. These procedures must be able to be carried out in a systematic fashion in order to prevent missed injuries.
Definitions
In order to clarify misinterpretation of these terms, standardized definitions must be employed. Screening laparoscopy is the assessment for peritoneal violation.
Once peritoneal violation has been confirmed, a systematic inspection of the peritoneal cavity, and retroperitoneal organs when necessary, must be performed. DL is therefore defined as a non-therapeutic procedure where no injuries are identified, or identified injuries do not require repair. TL is when an advanced maneuver is performed to repair an identified injury. Simple maneuvers such as organ mobilization, clot evacuation, or hemostatic agent application should not be considered TL [3, 4, 9, 11].
Diagnostic and TL in PAT
When examining the use of laparoscopy for PAT, there have been an increasing amount of publications supporting its use. We previously described the Veress needle insufflation technique as an adjunct to screening laparoscopy to increase the sensitivity of DL [17]. As a whole, laparoscopy for PAT has been widely accepted as a safe and accurate screening and diagnostic tool [2, 4, 5, 7,8,9,10, 12, 13, 18,19,20,21,22,23,24,25,26]. In specific settings, laparoscopy has even been adopted into the recommended treatment protocols from two major trauma organizations, both the Western Trauma Association and Eastern Association for the Surgery of Trauma [27, 28].
However, controversy still remains around the efficacy of TL. In recent literature, the rate of TL has been reported as low as 13.8% to as high as 83% [7, 9, 10, 15]. The variability in these reported rates may be attributed to individual surgeon experience with laparoscopy. In comparison to our experience, we witnessed a TL rate of 28.3%.
Out of the 56 diagnostic laparoscopic procedures performed in our study, 41 (74.2%) of the cases were performed by surgeons who completed fellowship training in advanced laparoscopy. The surgeons who performed DL with advanced training were less likely to convert to EL. Not surprisingly, a majority of the surgeons who performed TL, 11 out of 13 cases (84.6%), also fell into the category of having advanced laparoscopic training during fellowship.
The conversion rate from DL to EL in our study was 17.9%. This correlates with the rates documented in previous literature, which ranges from 7 to 37%. Common reasons for conversion include hemodynamic instability, extensive bleeding, complexity of injuries, poor visibility, and failure of equipment [2, 5, 9].
Factors to improve results of laparoscopy in trauma
It is our belief that several criteria exist which improve the success rates of DL and TL (Fig. 2). Our surgeons considered these factors when deciding to utilize laparoscopy in our trauma population.
The first aspect is laparoscopic skill set. Advanced laparoscopic maneuvers must be employed to inspect all spaces and repair all potential intra-abdominal organs. Fellowship training in laparoscopy helps provide the foundation for the technical skills to perform these maneuvers. These include, but are not limited to, the ability to run bowel, mobilize the retroperitoneum, and securely suture hollow viscous organs. If the trauma surgeon does not feel comfortable performing these techniques laparoscopically, laparotomy should be favored. In our experience, surgeons with advanced fellowship training in laparoscopy were more likely to perform DL (74.2%) and TL (84.6%).
The next aspect to consider is the mechanism of injury. Pertinent details include injury location, trajectory patterns, and velocity forces. Penetrating trauma in the anterior abdomen and thoracoabdomen, with identifiable trajectory patterns, and low- to medium-velocity injuries make DL and TL more practical. These aspects are especially important when dealing with gunshot wounds, as these injuries can be less predictable. If upon DL, the trajectory of the injury is unclear, or if the trauma is due to a high velocity force, consideration should be made for laparotomy. In our experience, surgeons analyzed these elements when deciding to proceed with laparoscopy for PAT, which helped prevent missed injuries during exploration.
Lastly, even in the hands of a skilled laparoscopist, certain injuries may be better evaluated and repaired via an open approach. Injuries that we feel may warrant this consideration include small bowel and retroperitoneal injuries. The inherent difficulty in assessing and treating these injuries laparoscopically, as well as the potential for missing a concomitant injury, may favor conversion to laparotomy.
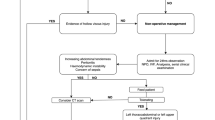
Treatment algorithm
To encourage more high-level studies in the future, treatment algorithms and systematic surgical approaches must be standardized. We propose the treatment algorithm as listed in Fig. 3 when approaching patients with PAT.
The first criterion to assess when considering DL in PAT is hemodynamic stability. Hemodynamic stability can be defined as maintaining systolic blood pressure > 100 mmHg, diastolic blood pressure > 60 mmHg, and heart rate < 110 bpm [3, 7, 15]. It has been universally accepted that hemodynamic instability mandates EL [27, 28]. To date, there has only been one study which examined the use of DL in hemodynamically unstable patients, conducted by Cherkasov et al. [29]. In this retrospective review of 2695 patients, which included both penetrating and blunt abdominal trauma, the authors concluded that DL can be confidently used in cases of hemodynamically unstable patients. However, there is insufficient high-level data to support this claim. As such, we recommend that DL only be considered in patients who are hemodynamically stable, based on the above parameters. It is important to remember that if the patient becomes clinically unstable at any point during the DL algorithm, they should undergo EL without delay.
After patients present with PAT and are identified as hemodynamically stable, further assessment of the injury must be performed. We suggest routine local wound exploration in the emergency room by probing the wound and assessing for fascial violation. If question still remains, further evaluation should be performed using imaging—through the use of ultrasonography (focused assessment with sonography for trauma—FAST) or CT scan. These imaging modalities help identify areas of injury and guide operative exploration. If any of these steps demonstrate intraperitoneal violation, or if the results are equivocal but there is high suspicion for intra-abdominal injury, the patient should be taken for DL.
Contraindications to laparoscopy in trauma
Several contraindications exist that preclude patients from undergoing DL. These include both anatomic limitations (e.g., patients with extensive previous abdominal surgeries, patients with a gravid uterus—especially during the 3rd trimester) and physiologic limitations (e.g., patients with uncorrectable coagulopathy, patients unable to tolerate pneumoperitoneum, patients with head trauma) [16, 30]. Another commonly cited contraindication for DL in PAT is organ evisceration. These patients have historically mandated EL. There has been one study conducted by Matsevych et al. who retrospectively examined the feasibility of DL and TL in stable PAT patients with organ evisceration. In their evaluation of 25 patients, 16 patients (64%) underwent successful therapeutic procedures (conducted as both LAA and FTL). They concluded “laparoscopic management is feasible, has a high accuracy in identifying intra-abdominal injuries, provides all benefits of minimal invasive surgery, and avoids non-therapeutic laparotomy” in this patient population [11].
Procedure
A stepwise approach for DL was first introduced by Kawahara et al. [12]. However, since that time, a standardization for the operative steps has not been clearly defined or utilized. A recent publication by Koto et al. clarified this issue by identifying these steps [4]. We agree with Koto et al.’s systematic abdominal examination; however, we offer a variation for the approach of port placement. We start with a camera port in the supra-umbilical area, and insufflate with carbon dioxide pneumoperitoneum to 12–15 mmHg. Our first two working ports are placed in the left and right mid-clavicular line several sonometers below the costal margins. Additional ports may be placed lower in the mid-clavicular line in the left and right iliac fossae positions as required for further diagnosis and treatment.
The main steps of the procedure, as outlined by Koto et al., are as follows: (1) port placement and accessing the abdominal cavity, (2) quick control of intra-abdominal bleeding sources, (3) stepwise examination of intraperitoneal and retroperitoneal organs, and (4) decision for therapeutic interventions—either fully laparoscopic, laparoscopic assisted, or through conversion to laparotomy. We suggest referencing Koto et al.’s paper for full detailed description [4]. By clarifying the details of the procedure, we aim to guide future studies to perform DL and TL in this same standardized fashion.
Study limitations
The current study has some limitations. Our study population is small. A larger study sample in each arm is required to determine statistical significance in other parameters. Another limitation is that this is an observational, retrospective study.
Literature is limited in comparing outcomes of laparoscopy and laparotomy for the management of PAT. In a 2016 systematic review and meta-analysis published by Hajibandeh et al. [2], only one randomized control trial (RCT) [31] was identified which makes such comparisons. The rest of relevant literature was observational in nature. Hajibandeh et al.’s analysis concluded that in hemodynamically stable patients with PAT, DL was a safe procedure that can improve avoidance of non-therapeutic laparotomies, reduce postoperative complications, and decrease hospital length of stay. However, they could not draw any conclusions regarding the role of TL [2]. The lack of high-level evidence supports the need for future prospective, multicenter, RCTs to evaluate TL compared to EL in PAT.
Conclusions
Our study adds to the body of literature that shows that laparoscopy can be utilized in the management of PAT for hemodynamically stable patients. Furthermore, we propose safe criteria under which laparoscopy can be optimally employed. Eighty-two percent of our patients were managed with laparoscopy alone and did not require conversion to laparotomy. A non-therapeutic laparotomy was avoided in 58.9% of our patients. No injuries were missed during procedures performed laparoscopically. Twenty-eight percent of our patients were treated with TL without any associated complications. The use of laparoscopy allowed for shorter hospital lengths of stay, which may be attributed to less postoperative pain and improved recovery time. Overall, a trauma surgeon with advanced laparoscopic skills can utilize laparoscopy as both a diagnostic and therapeutic maneuver in stable patients with PAT.
References
Shaftan GW (1969) Selective conservatism in penetrating abdominal trauma. J Trauma 9:1026–1027
Hajibandeh S, Hajibandeh S, Gumbar AO, Wong CS (2016) Laparoscopy versus laparotomy for the management of penetrating abdominal trauma: a systematic review and meta-analysis. Int J Surg 34:127–136
Matsevych O, Koto M, Balabyeki M, Aldous C (2017) Trauma laparoscopy: when to start and when to convert? Surg Endosc 32:1344–1352
Koto MZ, Matesevych OY, Aldous C (2018) Diagnostic laparoscopy for trauma: how not to miss injuries. J Laparoendosc Adv Surg Tech A. https://doi.org/10.1089/lap.2017.0562
Koto MZ, Matsevych OY, Motilall SR (2015) The role of laparoscopy in penetrating abdominal trauma: our initial experience. J Laparoendosc Adv Surg Tech A 25:730–736
Trejo-Ávila ME, Valenzuela-Salazar C, Betancourt-Ferreyra J, Fernández-Enríquez E, Romero-Loera S, Moreno-Portillo M (2017) Laparoscopic versus open surgery for abdominal trauma: a case-matched study. J Laparoendosc Adv Surg Tech A 27:383–387
O’Malley E, Boyle E, O’Callaghan A, Coffey JC, Walsh SR (2012) Role of laparoscopy in penetrating abdominal trauma: a systematic review. World J Surg 34:113–122
Uranues S, Popa DE, Diaconescu B, Schrittwieser R (2015) Laparoscopy in penetrating abdominal trauma. World J Surg 39:1381–1388
Matsevych OY, Koto MZ, Aldous C (2017) Laparoscopic-assisted approach for penetrating abdominal trauma: a solution for multiple bowel injuries. Int J Surg 44:94–98
Koto MZ, Matsevych OY, Aldous C (2017) Laparoscopic-assisted approach for penetrating abdominal trauma: an underutilized technique. J Laparoendosc Adv Surg Tech A 27:1065–1068
Matsevych OY, Koto MZ, Motilall SR, Kumar N (2016) The role of laparoscopy in management of stable patients with penetrating abdominal trauma and organevisceration. J Trauma Acute Care Surg 81:307–311
Kawahara NT, Alster C, Fujimura I, Poggetti RS, Birolini D (2009) Standardexamination system for laparoscopy in penetrating abdominal trauma. J Trauma 67:589–595
Zantut LF, Ivatury RR, Smith RS, Kawahara NT, Porter JM, Fry WR, Poggetti R, Birolini D, Organ CH Jr (1997) Diagnostic and therapeutic laparoscopy for penetrating abdominal trauma: a multicenter experience. J Trauma 42:825–831
Lim KH, Chung BS, Kim JY, Kim SS (2015) Laparoscopic surgery in abdominal trauma: a single center review of a 7-year experience. World J Emerg Surg. https://doi.org/10.1186/s13017-015-0007-8
Chol YB, Lim KS (2003) Therapeutic laparoscopy for abdominal trauma. Surg Endosc 17:421–427
Coleman L, Gilna G, Portenier D, Auyang E, Khan U, Grabo D, Wilson A, Szoka N (2017) Trauma laparoscopy from 1925 to 2017: publication history and study demographics of an evolving modality. J Trauma Acute Care Surg. https://doi.org/10.1097/TA.0000000000001780
Meytes V, Amaturo M, Price E, Ferzli G, Timoney M (2017) Intra-abdominal insufflation as a diagnostic modality for penetrating anterior abdominal wall trauma in a busy urban center: a retrospective case-series. Ann Laparosc Endosc Surg 2:49
Chestovich PJ, Browder TD, Morrissey SL, Fraser DR, Ingalls NK, Fildes JJ (2015) Minimally invasive is maximally effective: diagnostic and therapeutic laparoscopy for penetrating abdominal injuries. J Trauma Acute Care Surg 78:1076–1085
Shah M, Galante JM, Scherer LA, Utter GH (2014) The utility of laparoscopicevaluation of the parietal peritoneum in the management of anterior abdominalstab wounds. Injury 45:128–133
Karateke F, Özdoğan M, Özyazıcı S, Daş K, Menekşe E, Gülnerman YC, Bali I, Önel S, Gökler C (2013) The management of penetrating abdominal trauma by diagnostic laparoscopy: a prospective non-randomized study. Ulus Travma Acil Cerrahi Derg 19:53–57
Ahmed N, Whelan J, Brownlee J, Chari V, Chung R (2005) The contribution oflaparoscopy in evaluation of penetrating abdominal wounds. J Am Coll Surg 201:213–216
Miles EJ, Dunn E, Howard D, Mangram A (2004) The role of laparoscopy in penetrating abdominal trauma. JSLS 8:304–309
Ditmars ML, Bongard F (1996) Laparoscopy for triage of penetrating trauma: thedecision to explore. J Laparoendosc Surg 6:285–291
Ivatury RR, Simon RJ, Stahl WM (1992) A critical evaluation of laparoscopy inpenetrating abdominal trauma. J Trauma 34:822–828
Fabian TC, Croce MA, Stewart RM, Pritchard FE, Minard G, Kudsk KA (1993) A prospective analysis of diagnostic laparoscopy in trauma. Ann Surg 217:557–565
Lin HF, Wu JM, Tu CC, Chen HA, Shih HC (2010) Value of diagnostic and therapeutic laparoscopy for abdominal stab wounds. World J Surg 34:1653–1662
Como JJ, Bokhari F, Chiu WC, Duane TM, Holevar MR, Tandoh MA, Ivatury RR, Scalea TM (2010) Practice management guidelines for selective nonoperative management of penetrating abdominal trauma. J Trauma 68:721–733
Martin M (2018) Abdominal gunshot wounds. http://westerntrauma.org/documents/2018AlgorithmPresentations/2018AlgorithmAbdominalGSW.pdf. Accessed 30 Mar 2018
Cherkasov M, Sitnikov V, Sarkisyan B, Degtirev O, Turbin M, Yakuba A (2008) Laparoscopy versus laparotomy in management of abdominal trauma. Surg Endosc 22:228–231
Bowers SP, Hunter JG (2006) Contraindications to laparoscopy. In: Whelan RL, Fleshman JW, Fowler DL (eds) The SAGES manual. Perioperative care in minimally invasive surgery. Springer, New York, pp 25–32
Leppäniemi A, Haapiainen R (2003) Diagnostic laparoscopy in abdominal stab wounds: a prospective, randomized study. J Trauma 55:636–645
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Disclosures
Kevin Bain, Vadim Meytes, Grace C. Chang, and Michael F. Timoney have no conflicts of interest or financial ties to disclose.
Rights and permissions
About this article
Cite this article
Bain, K., Meytes, V., Chang, G.C. et al. Laparoscopy in penetrating abdominal trauma is a safe and effective alternative to laparotomy. Surg Endosc 33, 1618–1625 (2019). https://doi.org/10.1007/s00464-018-6436-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00464-018-6436-1