Abstract
Background
Previous observational studies have demonstrated the safety of discharging patients after laparoscopic appendectomy within the same day without hospitalization. The application of Enhanced Recovery After Surgery (ERAS) guidelines has resulted in shorter length of stay, fewer complications, and reduction in medical costs. The aim of this study was to investigate if ERAS protocol implementation in patients with acute uncomplicated appendicitis decreases the length of stay enough to allow for ambulatory laparoscopic appendectomy.
Methods
In this prospective, randomized controlled clinical trial, 108 patients were randomized into two groups: laparoscopic appendectomy with ERAS (LA-E) or laparoscopic appendectomy with conventional care (LA-C). The primary endpoint was postoperative length of stay. The secondary end points were time to resume diet, postoperative pain, postoperative complications, re-admission rate, and reoperation rate.
Results
From January 2016 through May 2017, 50 patients in the LA-E group and 58 in the LA-C were analyzed. There were no significant differences in preoperative data. Regarding the primary end point of the study, the ERAS protocol significantly reduced the postoperative length of stay with a mean of 9.7 h (SD: 3.1) versus 23.2 h (SD: 6.8) in the conventional group (p < 0.001). The ERAS protocol allowed ambulatory management in 90% of the patients included in this group. There was a significant reduction in time to resume diet (110 vs. 360 min, p < 0.001) and less moderate–severe postoperative pain (28 vs. 62.1%, p < 0.001) in the LA-E versus LA-C group. The rate of complications, readmissions, and reoperations were comparable in both groups (p = 0.772).
Conclusions
ERAS implementation was associated with a significantly shorter length of stay, allowing for the ambulatory management of this group of patients. Ambulatory laparoscopic appendectomy is safe and feasible with similar rates of morbidity and readmissions compared with conventional care.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Acute appendicitis is a common gastrointestinal disease affecting 5.7–57/per 100.000 individuals each year [1]. Laparoscopic appendectomy (LA) with admission to the hospital and next-day discharge is the standard of care treatment for non-perforated acute appendicitis [2].
The reported length of hospital stay for LA is 1.8–2.2 days and for open appendectomy is 2.88 days [3,4,5,6]. Observational studies have demonstrated the safety of discharging adults and children after LA within the same day without hospitalization [2, 7,8,9,10,11,12].
The use of postoperative recovery management protocols such as Enhanced Recovery After Surgery (ERAS) and fast-track programs are spreading worldwide with good outcomes in elective surgery. The implementation of ERAS guidelines has resulted in a shorter length of stay (LOS), fewer complications, fewer readmissions, and reduction in total medical cost [13]. Perioperative care in the acute care setting, for example, in patients with acute appendicitis still continues to use traditional principles. The implementation of ERAS protocols in an emergency setting remains challenging [10, 13]. Although observational studies exist, there are no randomized controlled trials to be found in the literature that address ERAS protocol versus conventional care for LA.
The aim of this study was to investigate if ERAS protocol implementation in patients with acute uncomplicated appendicitis decreases the postoperative LOS enough to allow for ambulatory LA.
Materials and methods
Study design
We conducted a prospective, open-labeled, single-center, randomized controlled trial. The study was performed at Hospital General “Dr. Manuel Gea González” in Mexico City from January 1, 2016 to May 30, 2017. This study was approved by the institutional research and ethical board of our hospital. The study was conducted according to the CONSORT statement. The study was registered at http://www.researchregistry.com (researchregistry3050).
Eligibility criteria for participants
Patients were enrolled in the emergency department after the diagnosis of acute appendicitis was made by a staff-surgeon. The diagnosis of appendicitis was based on clinical, biochemical, and imaging criteria. Inclusion criteria were patients of both sexes, aged between 18 and 70 years, with an American Society of Anesthesiologist (ASA) grade of I or II, and those who accepted and signed the informed consent form. Exclusion criteria were pregnant women, patients taking oral anticoagulants, patients with intraoperative findings of complicated acute appendicitis (gangrenous, perforated or with generalized peritonitis), patients with other concomitant pathology (gynecologic, urologic or other gastrointestinal disease) that required additional surgical procedures and patients who required open conversion.
Randomization
Consenting patients who fulfilled the inclusion criteria were assigned to one of two groups: LA with ERAS protocol (LA-E) or LA with conventional care (LA-C). All patients provided written informed consent before participation.
The randomization was performed by computer-generated numbers (EpiData Software version 2.0, Odense, Denmark) after the patients were assessed for eligibility. Treatment allocation was not masked to patients, physicians, or researchers at any timepoint.
Laparoscopic appendectomy with ERAS protocol
Preoperative care
We adapted previously published ERAS and outpatient protocols to patients with acute appendicitis [10, 13,14,15]. Patients and their caregivers were informed about the principles of the ERAS protocol. Patients received preoperative treatment with crystalloid isotonic solution (calculated according their requirements), antibiotics (ceftriaxone 1 g IV and metronidazole 500 mg IV), standard gastric prophylaxis (omeprazole 40 mg IV), and opioid-sparing analgesia (e.g., ketorolac 30 mg IV with acetaminophen 1 g IV). All patients received a thorough preoperative evaluation by the anesthesiology group. We asked patients to micturate before entering the operating room, thus avoiding the use of a bladder catheter.
Intraoperative care
All patients received balanced general anesthesia, and strict control of fluid therapy, prevention of hypothermia, analgesia, and hemodynamic changes were implemented to reduce the metabolic stress response. We infiltrated all port sites before incision with 0.5% bupivacaine. Anti-emesis prophylaxis was achieved with dexamethasone (4 mg IV) and ondansetron (8 mg IV). No nasogastric tubes or drains were inserted.
Postoperative care
After surgery, all patients were admitted to the recovery room. Patients were monitored in this area, and recordings of their vital signs and pain using the Visual Analogue Scale (VAS) every hour were obtained. Pain scores with VAS were classified as mild, moderate or severe (0–2, 3–7, and 8–10, respectively). Opioid-sparing multimodal analgesia was administered (ketorolac 30 mg IV with acetaminophen 1 g IV); antiemetics were employed if patients experienced nausea or vomiting (ondansetron 8 mg). Antibiotics were suspended after surgery. Early ambulation was promoted, and oral feeding with clear liquids was resumed when the patients were fully awakened.
Discharge
Patients were discharged once they had fulfilled the following criteria: ability to take oral feeding, full consciousness recovered, able to ambulate alone, pain adequately controlled with oral analgesics (VAS < 2), hemodynamic stability, capable of micturation, and absence of nausea and vomiting. The decision to discharge was made by an attending surgeon; patients were discharged home from the recovery room. Admission to the hospital was based on attending surgeon discretion or failure of patients to fulfill the above criteria.
Patients received the following instructions for home: advance their diet at home, avoid heavy weight lifting, and care for the wound daily. Patients were advised to return to the hospital if they had any of the following symptoms: abdominal pain, distention, wound dehiscence, vomiting or fever.
Laparoscopic appendectomy with conventional care
Preoperative care
Patients included in this group received standard care with IV fluids (liberal protocol), antibiotics (ceftriaxone 1 g IV q12 h and metronidazole 500 mg IV q8 h), opioid analgesics if needed (tramadol 50 mg IV), and a bladder catheter. Antiemetics were administered preoperatively only if patients presented nausea or vomiting.
Intraoperative care
No infiltration of the port sites was performed.
Postoperative care
After surgery, patients were admitted to the recovery room. Vitals and pain were recorded. Pain was controlled with opioid analgesia if it was severe (VAS = 8–10). Patients started oral feeding once bowel function was completely restored, defined by the presence of normal peristalsis, passage of flatus or depositions. Patients were admitted to the hospital if more than 12 h in the recovery room was anticipated.
Discharge
Patients were discharged home once a full normal diet was tolerated, ambulation was achieved, and pain was adequately controlled with oral analgesics (VAS < 2).
Surgical technique in both groups
LA was performed with the same standard surgical technique in all patients. Pneumoperitoneum was created by a closed technique using a Veress needle set at a 12 mmHg pressure. A standard three-port technique was employed with two 12-mm ports and one 5-mm port. The appendix and the appendicular artery were ligated with a simple extracorporeal sliding knot using a non-absorbable monofilament suture (0 polypropylene). The appendix was retrieved within a bag. The 12-mm port fascial defect was closed with absorbable sutures; skin was approximated with simple sutures. All procedures were performed by a surgical resident with direct supervision of an attending surgeon.
Follow-up
All patients were followed-up with clinical appointments on postoperative days 7 and 30. Postoperative complications, readmissions, and reoperations were recorded if they presented during the 30-day follow-up period.
End points
The primary end point of the study was postoperative LOS. The secondary end points were time to resume diet, postoperative pain, total LOS, 30-day postoperative complications, and readmission and reoperation rates.
Other variables registered and analyzed in the study were age, sex, body mass index kg/m2 (BMI), ASA score, total leukocyte count, C-reactive protein (mg/dL), and operative time (min).
Sample size
A power calculation performed utilized LOS data from a previous study [16], assuming that the mean total LOS of a conventional LA is 49.3 h (SD: 59.4) and that the mean LOS in ambulatory procedures should be less than 12 h [17]. To reduce the mean LOS by 75% from 49.3 h to 12 h, with an α error = 0.05 and 1 − β error = 0.80, the t test required a sample size of 41 in each arm.
Statistical analysis
We summarized the data as the means [standard deviation (SD)], medians [interquartile range (IQR)] or number of patients (percentages). The χ2 test or Fisher’s exact test was used for categorical variables, and Student’s t-test or Mann–Whitney U two-sample tests were used for continuous variables depending on the distribution. A two-sided p value < 0.05 was considered significant. The data were analyzed using SPSS version 18.0 for Windows (SPSS Inc. Chicago, IL, USA).
Results
Patients
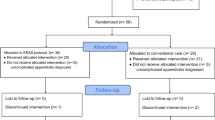
From January 2016 through May 2017, a total of 127 patients with acute appendicitis were assessed for eligibility. Figure 1 shows the study flow chart of patients and the CONSORT diagram. Four of these patients did not meet the inclusion criteria because they declined to participate. The remaining 123 patients were randomly enrolled, 60 were assigned to undergo LA with ERAS protocol and 63 to undergo LA with conventional care. During the surgical procedure, 15 more patients were excluded because of the diagnosis of a perforated appendicitis. Hence, there were 50 patients in the LA-E group and 58 patients in the LA-C for analysis. There was no loss to follow-up during the study period.
The baseline demographic data are shown in Table 1. The baseline characteristics between the two treatment groups did not differ significantly.
Primary end point
Regarding the primary end point of the study, the mean postoperative LOS was 9.7 h (SD: 3.1) in the ERAS protocol group, which was significantly shorter than in the control group receiving conventional care (mean of 23.2 h, SD: 6.8; p < 0.001). The results are summarized in Table 2.
It is important to mention that in the LA-E group, 5 (10%) patients stayed longer than 12 h in the recovery room. These 5 patients were admitted to the hospital. ERAS implementation allowed ambulatory management in 90% of the patients included in this group.
In the LA-C group, 2 (3.4%) patients stayed less than 12 h in the recovery room and were discharged home without needing admission to the hospital.
Secondary end points
Regarding the secondary end points, patients in the LA-E group resumed liquid diet earlier than patients in the LA-C group (110 vs. 360 min, p < 0.001).
In terms of postoperative pain control, patients in the LA-E group reported significantly less moderate-to-severe pain (n = 14) than patients in the control group (n = 36; p < 0.001).
The total LOS was significantly shorter in the LA-E group (16.2 h) than in the LA-C group (28.8 h; p < 0.001).
There were no differences between the two groups in terms of total complications, readmissions or reoperations. Including readmissions and reoperations, the overall success of ambulatory management (in LA-E group) was 86%.
No complications arose from the intervention (ERAS protocol implementation).
Discussion
Appendectomy is still considered to be the gold standard for uncomplicated appendicitis, with LA being the preferred approach. Benefits of LA in meta-analyses are as follows: reduced incidence of SSI, shorter hospital stay, diagnostic value, less pain, earlier return to work, earlier start of oral intake, improved scar and body satisfaction, and fewer incisional hernias [1, 18]. After LA, patients may rest 1–2 days in the hospital and lose 1–3 weeks of work or school [1, 19].
Few evidence-based interventions that optimize recovery after appendectomy have been published. Some of these interventions include fast-track protocols, needlescopic surgery, single-incision laparoscopic surgery, and transversus abdominis plane block. The results are still inconclusive, and randomized controlled trials are needed [19].
The ERAS concept, described in 1997 by Kehlet [20], is a multimodal, evidence-based, multidisciplinary approach to the care of the surgical patient [21]. The elements of the ERAS protocol are based on the reduction of surgical stress by reducing the neurohormonal response to the operation and retaining anabolic homeostasis, consequently resulting in less organ dysfunction and lower complication rates [22, 23].
ERAS programs are now widely accepted in laparoscopic colorectal surgery because of faster recovery and less perioperative complications [13, 21]. ERAS pathways are mostly used in elective surgeries, with a minimal number of publications adapting ERAS programs to emergency surgery [24,25,26]. Recent publications in the acute care setting are searching for methods to reduce LOS and hospital costs while maintaining a high quality of care and patient satisfaction [3].
The ERAS Society published a series of guidelines with procedure-specific recommendations [21, 27]. The major challenge of this study was the adaptation of recommendations that are planned for elective surgery to patients who need emergency surgery. For example, the ERAS guidelines recommended preoperative optimization (increase exercise preoperatively and cease smoking and alcohol use) and preoperative carbohydrate treatment, procedures that are effective in elective surgery but very difficult to implement in the acute care setting [13].
Pediatric surgeons have implemented and published protocols aiming to reduce LOS and demonstrated that LA may be safely performed as fast-track or same-day surgery in select children without a perforated appendicitis [12]. In a prospective study of 158 children, Alkhoury et al. [9] reported similar complication rates compared with the control group, with a success rate of 80% and a satisfaction rate of 87% regarding same-day discharge after LA.
Several observational studies debate the safety and feasibility of fast-track protocols for adult patients with appendicitis. In a retrospective study, Cross et al. [7] found that there was no significant difference in complications or readmission between patients discharged in less than 24 h and those who stayed longer.
Cash et al. [10] reported prospective data that included more than 100 patients and compared them with historical controls; they showed no difference in morbidity and mortality.
Scott et al. [2] recently published a large retrospective study comparing same-day discharge (n = 6710) and hospitalized groups (n = 5993), and they concluded that adult patients with acute non-perforated appendicitis can be discharged safely on the day of surgery without higher rates of postoperative complication or readmission rates.
Finally, Frazee et al. [5] described a prospective protocol for outpatient LA, where patients were dismissed from the post-anesthesia recovery room if they met certain predefined criteria. They reported no mortalities or reoperations, 1.2% readmissions, 6.7% morbidity, and 85% overall success with outpatient management. Furthermore, the same authors recently published the application of this protocol in seven institutions and described low morbidity (5%) and low readmission rates (3%), concluding that the application of this practice could reduce LOS and decrease overall health care costs for acute appendicitis [28].
The incidence of postoperative complications after appendectomy ranges from 3.0 to 28.7% [1]. We did not consider that the readmission and complication rates found in our study could be attributed to the treatment protocol because intra-abdominal abscesses and hematomas are well described complications of LA.
Ambulatory surgery corresponds to a surgical procedure performed in the safety of an operating room environment, under a variable form of anesthesia, during a hospital stay of less than 12 h [16, 17]. Laparoscopic surgery allows elective procedures to be performed on an outpatient or ambulatory basis [27]. The trend toward ambulatory laparoscopic procedures includes cholecystectomy, gastric bypass, hernia repair, and hysterectomy [10]. Various authors have suggested that patients with appendicitis could be selectively treated on an outpatient basis with no increase in morbidity or mortality [10, 16]. Because LA is an emergency procedure, one of the concerns with outpatient management is patient acceptance and satisfaction [5]. As suggested in previous studies, we addressed this subject with the preoperative counseling of patients and families, providing extensive information about the disease, treatment and benefits of an early discharge.
Lefrancois et al. [16] established a simple validated predictive score of early discharge that allowed them to select patients who were eligible for ambulatory surgery with a success rate of 97%. They named it the Saint-Antoine Score; it includes BMI < 28 kg/m2, total leukocyte count < 15,000, C-reactive protein < 30 mg/L, no radiological signs of perforation and appendix diameter < 10 mm. Although we did not calculate this score in our study, we found that our patients had a mean BMI of 25.1 (± 2.8), total leukocyte count of 15.06 (± 3.8), C-reactive protein of 3.17 (± 3.1), and patients with signs of perforation were excluded.
The primary outcome of this study was LOS following LA performed within an ERAS protocol. We demonstrated a reduction in LOS in 90% of the patients, enough to allow for ambulatory management of these patients (discharge from the recovery room in less than 12 h after surgery). Although ambulatory LA is a common practice that has been adopted gradually, randomized controlled trials are lacking to support this practice.
Even though this is a randomized controlled trial, a major limitation of our study was the lack of masking and subsequent risk of performance bias. This limitation has been reported in multiple previous randomized trials comparing ERAS protocol implementation versus conventional care [24, 28, 29]. Another issue is that our sample size was calculated with a LOS of 49.3 h (SD: 59.4) [16], and this LOS may appear obsolete to many centers that perform outpatient appendectomy. We chose this LOS because of the fact that our control group was conventional or traditional care. Other limitations of our study were that we did not evaluate the economic impact of decreasing the LOS or the overall patient satisfaction of being discharged home without hospitalization.
Conclusions
ERAS implementation was associated with a significantly shorter length of hospital stay compared with conventional care, allowing for the ambulatory management of this group of patients. Although not widely adopted, ambulatory LA is safe and feasible in adult patients with non-complicated appendicitis with similar rates of readmissions and morbidity compared with conventional care.
References
Gorter RR, Eker HH, Gorter-Stam MA, Abis GS, Acharya A, Ankersmit M, Antoniou SA, Arolfo S, Babic B, Boni L, Bruntink M, van Dam DA, Defoort B, Deijen CL, DeLacy FB, Go PM, Harmsen AM, van den Helder RS, Iordache F, Ket JC, Muysoms FE, Ozmen MM, Papoulas M, Rhodes M, Straatman J, Tenhagen M, Turrado V, Vereczkei A, Vilallonga R, Deelder JD, Bonjer J (2016) Diagnosis and management of acute appendicitis. EAES consensus development conference 2015. Surg Endosc 30(11):4668–4690
Scott A, Shekherdimian S, Rouch JD, Sacks GD, Dawes AJ, Lui WY, Bridges L, Heisler T, Crain SR, Cheung MKW, Aboulian A (2017) Same-day discharge in laparoscopic acute non-perforated appendectomy. J Am Coll Surg 224(1):43–48
Trevino CM, Katchko KM, Verhaalen AL, Bruce ML, Webb TP (2015) Cost effectiveness of a fast-track protocol for urgent laparoscopic cholecystectomies and appendectomies. World J Surg 40(4):856–862
Gilliam AD, Anand R, Horgan LF, Attwood SE (2008) Day case emergency laparoscopic appendectomy. Surg Endosc 22(2):483–486
Frazee RC, Abernathy SW, Isbell CL, Isbell T, Regner JL, Smith RD (2016) Outpatient laparoscopic appendectomy: is it time to end the discussion? J Am Coll Surg 222(4):473–477
Ingraham AM, Cohen ME, Bilimoria KY, Ko CY, Hall BL, Russell TR, Nathens AB (2010) Effect of delay of operation on outcomes in adults with acute appendicitis. Arch Surg 145(9):886–892
Cross W, Chandru Kowdley G (2013) Laparoscopic appendectomy for acute appendicitis: a safe same-day surgery procedure? Am Surg 79(8):802–805
Akkoyun I (2013) Outpatient laparoscopic appendectomy in children: a single center experience with 92 cases. Surg Laparosc Endosc Percutan Tech 23(1):49–50
Alkhoury F, Burnweit C, Malvezzi L, Knight C, Diana J, Pasaron R, Mora J, Nazarey P, Aserlind A, Stylianos S (2012) A prospective study of safety and satisfaction with same-day discharge after laparoscopic appendectomy for acute appendicitis. J Pediatr Surg 47(2):313–316
Cash CL, Frazee RC, Abernathy SW, Childs EW, Davis ML, Hendricks JC, Smith RW (2012) A prospective treatment protocol for outpatient laparoscopic appendectomy for acute appendicitis. J Am Coll Surg 215(1):101–105
Jain A, Mercado PD, Grafton KP, Dorazio RA (1995) Outpatient laparoscopic appendectomy. Surg Endosc 9(4):424–425
Grewal H, Sweat J, Vazquez D (2004) Laparoscopic appendectomy in children can be done as a fast-track or same-day surgery. JSLS 8(2):151–154
Gustafsson UO, Scott MJ, Schwenk W, Demartines N, Roulin D, Francis N, McNaught CE, MacFie J, Liberman AS, Soop M, Hill A, Kennedy RH, Lobo DN, Fearon K, Ljungqvist O (2013) Guidelines for perioperative care in elective colonic surgery: enhanced recovery after surgery (ERAS) society recommendations. World J Surg 37(2):259–284
Dubois L, Vogt KN, Davies W, Schlachta CM (2010) Impact of an outpatient appendectomy protocol on clinical outcomes and cost: a case-control study. J Am Coll Surg 211(6):731–737
Lasso-Betancor CE, Ruiz-Hierro C, Vargas-Cruz V, Orti-Rodriguez RJ, Vazquez-Rueda F, Paredes-Esteban RM (2013) Implementation of “fast-track” treatment in paediatric complicated appendicitis. Cir Pediatr 26(2):63–68
Lefrancois M, Lefevre JH, Chafai N, Pitel S, Kerger L, Agostini J, Canard G, Tiret E (2014) Managemet of acute appendicitis in ambulatory surgery. is it possible? How to select patients? Ann Surg 261(6):1167–1172
Kraft K, Mariette C, Sauvanet A, Balon JM, Douard R, Fabre A, Guidat A, Huten N, Johanet H, Laurent A, Muscari F, Pessaux P, Pierme JP, Piessen G, Raucoules-Aime M, Rault A, Vons C (2011) Indications for ambulatory gastrointestinal and endocrine surgery in adults. J Visc Surg 148(1):69–74
Sauerland S, Jaschinski T, Neugebauer EA (2010) Laparoscopic versus open surgery for suspected appendicitis. Cochrane Database Syst Rev. https://doi.org/10.1002/14651858.CD001546
Hamill JK, Rahiri JL, Gunaratna G, Hill AG (2016) Interventions to optimize recovery after laparoscopic appendectomy: a scoping review. Surg Endosc 31(6):2357–2365
Kehlet H (1997) Multimodal approach to control postoperative pathophysiology and rehabilitation. Br J Anaesth 78(5):606–617
Ljungqvist O, Scott M, Fearon KC (2017) Enhanced recovery after surgery: a review. JAMA Surg 152(3):292–298
Garulli G, Lucchi A, Berti P, Gabbianelli C, Siani LM (2016) “Ultra” E.R.A.S. in laparoscopic colectomy for cancer: discharge after the first flatus? A prospective, randomized trial. Surg Endosc 31(4):1806–1813
Kehlet H (2006) Surgical stress and postoperative outcome from here to where? Reg Anesth Pain Med 31:47–52
Mohsina S, Shanmugam D, Sureshkumar S, Kundra P, Mahalakshmy T, Kate V (2017) Adapted ERAS pathway vs. standard care in patients with perforated duodenal ulcer: a randomized controlled trial. J Gastrointest Surg. https://doi.org/10.1007/s11605-017-3474-2
Lohsiriwat V (2014) Enhanced recovery after surgery vs. conventional care in emergenc y colorectal surgery. World J Gastroenterol 20(38):13950–13955
Gonenc M, Dural AC, Celik F, Akarsu C, Kocatas A, Kalayci MU, Dogan Y, Alis H (2014) Enhanced postoperative recovery pathways in emergency surgery: a randomized controlled clinical trial. Am J Surg 207(6):807–814
Frazee R, Burlew CC, Regner J, McIntyre R, Peltz E, Cribari C, Dunn J, Butler L, Reckard P, Dissanaike S, Karimi K, Behnfield C, Melo N, Margulies D (2017) Outpatient laparoscopic appendectomy can be successfully performed for uncomplicated appendicitis: a Southwestern Surgical Congress Multicenter Trial. Am J Surg. https://doi.org/10.1016/j.amjsurg.2017.08.029
Lemanu DP, Singh PP, Berridge K, Burr M, Birch C, Babor R, MacCormick AD, Arroll B, Hill AG (2013) Randomized clinical trial of enhanced recovery versus standard care after laparoscopic sleeve gastrectomy. Br J Surg 100:482–489
Spanjersberg WR, Reurings J, Keus F, van Laarhoven CJ (2011) Fast track surgery versus conventional recovery strategies for colorectal surgery. Cochrane Database Syst Rev 2:CD007635
Acknowledgements
We would like to thank Violeta Díaz-Fermin MD, for helping us in collecting data.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Disclosures
Mario E. Trejo-Ávila, Sujey Romero-Loera, Eduardo Cárdenas-Lailson, Miguel Blas-Franco, Roberto Delano-Alonso, Carlos Valenzuela-Salazar, and Mucio Moreno-Portillo have no conflicts of interest or financial ties to disclose.
Rights and permissions
About this article
Cite this article
Trejo-Ávila, M.E., Romero-Loera, S., Cárdenas-Lailson, E. et al. Enhanced recovery after surgery protocol allows ambulatory laparoscopic appendectomy in uncomplicated acute appendicitis: a prospective, randomized trial. Surg Endosc 33, 429–436 (2019). https://doi.org/10.1007/s00464-018-6315-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00464-018-6315-9