Abstract
Background
Only a few reports discuss long-term functional outcomes and changes observed in patients over several years following a distal gastrectomy. We investigated long-term functional outcomes and changes after laparoscopic distal gastrectomy based on the analysis of postoperative conditions and endoscopic findings observed in patients.
Methods
The study group comprised 159 patients who underwent Roux-en-Y reconstruction following laparoscopic distal gastrectomy (R-Y group) between December 2008 and November 2012 and 78 patients who underwent Billroth I reconstruction (B-I group) between January 2002 and November 2012. To minimize bias between the two groups, propensity scores were calculated using a logistic regression model. The groups were compared with respect to postoperative conditions and endoscopic findings at 1, 3, and 5 years postoperatively.
Results
The B-I group demonstrated more frequent heartburn than the R-Y group at 3 and 5 years postoperatively. No significant differences were found in terms of loss of body weight and food intake. Endoscopic findings showed significantly lesser residual food and remnant gastritis in the R-Y group at each annual postoperative follow-up. The incidence of bile reflux and reflux esophagitis in the B-I group gradually increased over the years and showed a significant difference at the culmination of the 5-year postoperative follow-up, compared to the R-Y group.
Conclusions
Roux-en-Y reconstruction was superior to Billroth I reconstruction in terms of frequency of occurrence of residual food, bile reflux, remnant gastritis, and reflux esophagitis in the long term. Differences between the two methods became more evident as the follow-up period lengthened.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Billroth I (B-I), Billroth II (B-II), and Roux-en-Y (R-Y) are reconstruction methods commonly used after distal gastrectomy (DG); however, the selection of a reconstruction method after DG remains controversial [1, 2].
In Japan, B-II reconstruction is rarely used due to the associated risk of afferent loop syndrome and the likelihood of bile reflux, which could result in inflammation in the remnant stomach [3]. B-I reconstruction allows food to pass directly through the stomach into the duodenum [4]; however, duodenogastric reflux has been recognized after B-I reconstruction. Roux stasis syndrome or delayed gastric emptying may occur after R-Y reconstruction, which influences the patient’s postoperative quality of life (QOL) [5].
Some randomized controlled trials and meta-analyses have compared B-I and R-Y reconstruction and concluded that B-I and R-Y reconstruction were generally equivalent in terms of surgical outcomes and postoperative QOL [6,7,8]. Reportedly, the incidence of remnant gastritis and reflux esophagitis is higher after B-I reconstruction than after R-Y reconstruction [7,8,9,10]; however, most studies have only investigated short-term outcomes. Furthermore, no study has evaluated changes occurring over several years.
With a greater than 50% incidence of early gastric cancer in Japan, laparoscopic surgery is popularly being used as a treatment option with a promising prognosis [11]. In this era of minimally invasive surgery, a patient’s QOL is an important consideration. Therefore, it is important to determine whether minimally invasive surgery results in satisfactory long-term outcomes.
In 2008, we launched β-shaped total intracorporeal R-Y reconstruction after laparoscopic distal gastrectomy (LDG) [12]. In this study, we compare R-Y (β-shaped reconstruction) and B-I reconstruction after LDG in terms of long-term functional outcomes and changes occurring in these outcomes over the years, by analyzing postoperative patients’ conditions and endoscopic findings.
Materials and methods
Patients
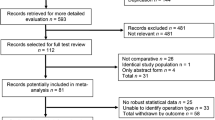
We retrospectively obtained data of 159 patients who underwent β-shaped R-Y reconstruction after LDG (R-Y group) between December 2008 and November 2012 and compared these data to that of 78 patients who underwent B-I reconstruction after laparoscopy-assisted distal gastrectomy (LADG) (B-I group) between January 2002 and November 2012. We excluded 14 patients from the R-Y group (12 patients who died within 5 years and two patients who underwent total gastrectomy for remnant gastric cancer). We also excluded five patients from the B-I group (four patients who died within 5 years and one patient who underwent a total gastrectomy for remnant gastric cancer).
As the short-term functional outcomes of the R-Y reconstruction were superior to those of the B-I reconstruction at our institute [10], we changed our reconstruction method from B-I to R-Y during the study period; therefore, patients belonging to the B-I group were relatively older than those in the R-Y group. We performed propensity-score matching to minimize bias between the two groups of patients. Propensity scores were calculated using a logistic regression model and included the following variables: sex, age, body mass index (BMI), the American Society of Anesthesiologists physical status (ASA ps) class, and the Japanese Classification of Gastric Carcinoma (JCGS) stage [13]. Patients were individually matched between the R-Y and B-I groups using the nearest-neighbor matching method. This method consists of randomly ordering the case and control subjects, selecting the first case subject, and then finding the control subject with the closest propensity score. Finally, 94 patients (47 of whom underwent R-Y reconstruction and 47 of whom underwent B-I reconstruction) were matched using this method.
This study was conducted according to the Declaration of Helsinki principles and was approved by the Institutional Review Board of Tokyo Medical and Dental University (M2017-072).
Surgical procedures
In December 2008, we launched the β-shaped reconstruction [12] (Fig. 1) as an intracorporeal R-Y procedure after an LDG. An isoperistaltic gastrojejunostomy was performed by constructing a side-to-side anastomosis using a 60-mm endoscopic linear stapler (Echelon Flex 60 with a 60/3.6 mm blue cartridge; Ethicon, Cincinnati, OH, USA). The common entry hole of the gastrojejunostomy and the jejunum was closely approximated using a 60-mm endoscopic linear stapler (Echelon Flex 60 with a 60/3.6 mm blue cartridge; Ethicon, Cincinnati, OH, USA). We maintained a 25 cm distance between the gastrojejunostomy and the jejunojejunostomy.
B-I reconstruction involves the creation of a gastroduodenal anastomosis using a circular stapler or a hand-sewn suture through a small midline incision. As β-shaped reconstruction has been launched, it has been used more frequently in our hospital than the B-I reconstruction.
Long-term postoperative outcomes
We retrospectively obtained data pertaining to loss of body weight, compared to the preoperative status, and the use of proton pump inhibitors and/or camostat mesilate at 1, 3, and 5 years postoperatively. The quantity of postoperative food intake compared to the preoperative quantity, symptoms of heartburn, and dumping syndrome were estimated using a medical chart. Postoperative endoscopic findings at 1, 3, and 5 years were classified based on the residue, gastritis, and bile (RGB) classification [14]. We defined reflux esophagitis grade A or higher of the Los Angeles classification [15] as “1.” No reflux esophagitis and grade M of the classification were defined as “0.”
Statistical analysis
All P values were two-sided, and a P value ≤ 0.05 was considered statistically significant. All statistical analyses were performed using Easy R (EZR) software [16], which is a graphical user interface for R (the R Foundation for Statistical Computing, Vienna, Austria, version 2.13.0). More precisely, it is a modified version of R commander designed to add statistical functions frequently used in biostatistics.
Results
Patient characteristics are shown in Table 1. No significant intergroup differences were found in patient characteristics after propensity matching. Intra- and postoperative outcomes are shown in Table 2. Operative time was significantly longer in the R-Y group than in the B-I group (P < 0.001). Soft diet initiation and postoperative hospital stay were significantly shorter in the R-Y group than in the B-I group; however, there were no significant differences in blood loss volume and the incidence rate of postoperative complications corresponding to grade III or higher of the Clavien–Dindo classification [17].
Long-term outcomes pertaining to the postoperative condition of patients are shown in Fig. 2. Those belonging to the B-I group demonstrated significant heartburn more frequently than the R-Y group at 1 and 3 years postoperatively (P = 0.004 and P = 0.001, respectively) (Fig. 2A). Additionally, the incidence of heartburn in patients belonging to the B-I group was observed to have gradually increased until their 5-year postoperative follow-up.
Patients’ symptom, nutritional status, and medication at 1, 3, and 5 years postoperatively (R-Y group vs. B-I group). A Symptom of heartburn. B Symptom of dumping syndrome. C Body weight loss. D Amount of food intake. E Postoperative use of proton pump inhibitor. F Postoperative use of camostat mesilate
No significant differences were found in the incidence of patients who demonstrated the dumping syndrome at each postoperative year (Fig. 2B). Patients belonging to both groups lost approximately 10% body weight, and their food intake decreased by < 20%, indicating no significant differences between both groups (Fig. 2C, D). With regard to postoperative medication use, no significant difference was observed in the incidence of proton pump inhibitor intake and camostat mesilate (Fig. 2E, F).
Regarding endoscopic findings based on the RGB classification [14], the percentage rating of score 1 and more at 1, 3, and 5 years postoperatively is shown in Fig. 3. Residual food was found to be significantly lesser in the R-Y group than in the B-I group at each postoperative year (P = 0.019, P = 0.037, and P = 0.006, respectively) (Fig. 3A), and a gradual decrease is shown in both groups. The degree and extent of remnant gastritis was significantly lower in the R-Y group than in the B-I group at each postoperative year (P = 0.013, P < 0.001, and P < 0.001, respectively) (Fig. 3B). Both the degree and extent of remnant gastritis in the R-Y group gradually decreased, although those of the B-I group were observed to gradually increase. No significant differences were found between the two groups in terms of the incidence of bile reflux at the 1- and 3-year postoperative follow-up (P = 1.000 and P = 0.052, respectively) (Fig. 3C). However, this was found to gradually increase in the B-I group. Thus, the incidence of bile reflux at the 5-year postoperative follow-up was significantly lower in the R-Y group than in the B-I group (P < 0.001). The differences in the incidence of reflux esophagitis were similar to those of bile reflux (Fig. 3D). The incidence gradually decreased in the R-Y group but gradually increased in the B-I group. Thus, the incidence of reflux esophagitis at the 3- and 5-year postoperative follow-up was significantly lower in the R-Y group than in the B-I group (P = 0.007 and P = 0.004, respectively). In addition, two patients in the R-Y group (4.3%) demonstrated marginal ulcers in the 5-year postoperative follow-up; however, no significant differences were found between the R-Y and B-I groups (4.3 vs 0.0%, P = 0.495).
Discussion
The β-shaped R-Y reconstruction is an isoperistaltic anastomosis. We used a 60-mm endoscopic linear stapler to create a wide gastrojejunostomy aimed at preventing delayed gastric emptying. According to the Roux limb, the previous study investigated a short Roux limb (≤ 25 cm) was superior for patient outcomes compared with a long Roux limb (≥ 35 cm) [18]. Thus, we ensured that we maintained a 25-cm distance between the gastrojejunostomy and the jejunojejunostomy to prevent reflux of intestinal fluid and occurrence of the Roux stasis syndrome.
This study revealed that the R-Y group showed better results compared to the B-I group with respect to the incidence of residual food, bile reflux, remnant gastritis, and reflux esophagitis at the 5-year postoperative follow-up in comparison to the 1- and 3-year postoperative follow-up. Moreover, patients belonging to the R-Y group demonstrated a lower incidence of heartburn; however, parameters of nutritional status, such as body weight and the need for proton pump inhibitors and camostat mesilate, were similar between both groups.
Previous studies investigating functional outcomes at the 1-year follow-up post DG [1, 6,7,8,9,10] have shown that the R-Y group demonstrated lesser or equivalent incidence of residual food, bile reflux, remnant gastritis, and reflux esophagitis in terms of endoscopic findings, although the nutritional status was found to be similar between both groups. Evaluation at the 5-year postoperative follow-up [19, 20] has shown that the R-Y group demonstrated lesser incidence of residual food, bile reflux, remnant gastritis, and reflux esophagitis in terms of endoscopic findings and lesser reflux symptoms.
The primary difference in comparison to previous studies [1, 6,7,8,9,10, 19, 20] was that we studied changes in patients’ conditions and endoscopic findings over several years. Most previous studies have compared these groups at the end of 1 year, such as at the 1- or 5-year postoperative follow-up. To the best of our knowledge, there were very few studies, if any, which have compared the groups and studied changes occurring over multiple years like we did in our study wherein we also focused on changes in outcomes 5 years postoperatively.
Another unique feature of our study is that we investigated the long-term functional outcomes following a total intracorporeal R-Y reconstruction. Although benefits of short-term outcomes associated with minimally invasive surgery (laparoscopy and robot-assisted procedures) are well known and proven, their long-term efficacy is yet to be investigated. A total intracorporeal reconstruction following a gastrectomy is a technically challenging procedure. Determining an acceptable morbidity rate and satisfactory long-term functional outcomes are essential for the standardization of intracorporeal reconstruction. We reckon that our findings can provide newer insights into this complex issue.
Although gastric acid secretion decreases after gastrectomy, remnant gastritis and reflux esophagitis are known to occur in relation to the duodenogastric reflux following a DG procedure [21]. This study showed that the incidence rate of remnant gastritis, bile reflux, and reflux esophagitis was lower in the R-Y group than in the B-I group. This may be clinically plausible because duodenogastric reflux was observed to be less prominent in the R-Y group [21]. Furthermore, this study showed that the R-Y group was superior to the B-I group in terms of endoscopic findings at the 5-year postoperative follow-up in comparison to the 1- and 3-year follow-up, suggesting worsening of the duodenogastric reflux in the B-I group, which may be related to the recovery of the temporarily decreased bile secretion after gastrectomy [22].
The disadvantages of R-Y reconstruction in comparison to B-I reconstruction are as follows: a longer operation time, a higher incidence of Roux stasis syndrome, and the impossibility of performing endoscopic visualization of the ampulla of Vater or endoscopic retrograde cholangiopancreatography after the operation. Roux stasis syndrome is characterized by symptoms of upper gastrointestinal tract stasis after R-Y reconstruction and is presumably caused by an ectopic pacemaker in the Roux limb [23]. Roux stasis syndrome was not diagnosed in any of our patients even 5 years after the operation. Roux stasis syndrome is commonly observed when the length of a Roux limb exceeds 40 cm [24]. Thus, we ensured the Roux limb in our patients measured 25 cm (< 30 cm in length).
The limitations to our study are as follows: (1) It was a retrospective study, although data collection was performed in a prospective manner. (2) Patients belonging to the B-I group were relatively older than those in the R-Y group due to changes in our reconstruction methods during the study period, so it cannot be denied that technical and theoretical progress might influence the results of our study. Thus, we performed propensity-score matching to minimize bias between the two groups of patients. In addition, although the present study provides valuable informative data, a prospective randomized controlled trial would be needed to establish conclusive results.
In conclusion, R-Y reconstruction was found to be superior to B-I reconstruction in terms of frequency of the incidence of residual food, bile reflux, remnant gastritis, and reflux esophagitis at 1, 3, and 5 years postoperatively, and the differences between the two procedures became more evident/prominent as the follow-up period lengthened. Thus, we propose that our novel β-shaped R-Y reconstruction is a useful total intracorporeal reconstruction method demonstrating satisfactory long-term functional outcomes.
Abbreviations
- BMI:
-
Body mass index
- B-I:
-
Billroth I
- B-II:
-
Billroth II
- R-Y:
-
Roux-en-Y
- DG:
-
Distal gastrectomy
- LADG:
-
Laparoscopic-assisted distal gastrectomy
- LDG:
-
Laparoscopic distal gastrectomy
- QOL:
-
Quality of life
- SD:
-
Standard deviation
References
Kim CH, Song KY, Park CH, Seo YJ, Park SM, Kim JJ (2015) A comparison of outcomes of three reconstruction methods after laparoscopic distal gastrectomy. J Gastric Cancer 15:46–52
Lee MS, Ahn SH, Lee JH, Park DJ, Lee HJ, Kim HH, Yang HK, Kim N, Lee WW (2012) What is the best reconstruction method after distal gastrectomy for gastric cancer? Surg Endosc 26:1539–1547
Katai H, Nunobe S, Saka M, Fukagawa T, Sano T (2008) Reconstruction after distal gastrectomy. J Jpn Surg Soc 109:264–268
Yoshino K (2000) History of gastric cancer surgery. J Jpn Surg Soc 101:855–860
Hirao M, Fujitani K, Tsujinaka T (2005) Delayed gastric emptying after distal gastrectomy for gastric cancer. Hepatogastroenterology 52:305–309
Takiguchi S, Yamamoto K, Hirao M, Imamura H, Fujita J, Yano M, Kobayashi K, Kimura Y, Kurokawa Y, Mori M, Doki Y (2012) A comparison of postoperative quality of life and dysfunction after Billroth I and Roux-en-Y reconstruction following distal gastrectomy for gastric cancer: results from a multi-institutional RCT. Gastric Cancer 15:198–205
Hirao M, Takiguchi S, Imamura H, Yamamoto K, Kurokawa Y, Fujita J, Kobayashi K, Kimura Y, Mori M, Doki Y (2013) Comparison of Billroth I and Roux-en-Y reconstruction after distal gastrectomy for gastric cancer: one-year postoperative effects assessed by a multi-institutional RCT. Ann Surg Oncol 20:1591–1597
Xiong JJ, Altaf K, Javed MA, Nunes QM, Huang W, Mai G, Tan CL, Mukherjee R, Sutton R, Hu WM, Liu XB (2013) Roux-en-Y versus Billroth I reconstruction after distal gastrectomy for gastric cancer: a meta-analysis. World J Gastroenterol 19:1124–1134
Kitagami H, Morimoto M, Nozawa M, Nakamura K, Tanimura S, Murakawa K, Murakami Y, Kikuchi K, Ushigome H, Sato L, Yamamoto M, Shimizu Y, Hayakawa T, Tanaka M, Hirano S (2014) Evaluation of the delta-shaped anastomosis in laparoscopic distal gastrectomy: midterm results of a comparison with Roux-en-Y anastomosis. Surg Endosc 28:2137–2144
Kojima K, Yamada H, Inokuchi M, Kawano T, Sugihara K (2008) A comparison of Roux-en-Y and Billroth-I reconstruction after laparoscopy-assisted distal gastrectomy. Ann Surg 247:962–967
Nashimoto A, Akazawa K, Isobe Y, Miyashiro I, Katai H, Kodera Y, Tsujitani S, Seto Y, Furukawa H, Oda I, Ono H, Tanabe S, Kaminishi M (2013) Gastric cancer treated in 2002 in Japan: 2009 annual report of the JGCA nationwide registry. Gastric Cancer 16:1–27
Motoyama K, Kojima K, Hayashi M, Kato K, Inokuchi M, Sugihara K (2014) β-shaped intracorporeal Roux-en-Y reconstruction after totally laparoscopic distal gastrectomy. Gastric Cancer 17:588–593
Japanese Gastric Cancer Association (2011) Japanese classification of gastric carcinoma: 3rd English edition. Gastric Cancer 14:101–112
Kubo M, Sasako M, Gotoda T, Ono H, Fujishiro M, Saito D, Sano T, Katai H (2002) Endoscopic evaluation of the remnant stomach after gastrectomy: proposal for a new classification. Gastric Cancer 5:83–89
Miwa H, Yokoyama T, Hori K, Sakagami T, Oshima T, Tomita T, Fujikawa Y, Saita H, Itou T, Ogawa H, Nakamura Y, Kishi K, Murayama Y, Hayashi E, Kobayashi K, Tano N, Matsushita K, Kawamoto H, Sawada Y, Ohkawa A, Arai E, Nagao K, Hamamoto N, Sugiyasu Y, Sugimoto K, Hara H, Tanimura M, Honda Y, Isozaki K, Noda S, Kubota S, Himeno S (2008) Interobserver agreement in endoscopic evaluation of reflux esophagitis using a modified Los Angeles classification incorporating grades N and M: a validation study in a cohort of Japanese endoscopists. Dis Esophagus 21:355–363
Kanda Y (2013) Investigation of the freely available easy-to-use software ‘EZR’ for medical statistics. Bone Marrow Transplant 48:452–458
Dindo D, Demartines N, Clavien PA (2004) Classification of surgical complications: a new proposal with evaluation in a cohort of 6336 patients and results of a survey. Ann Surg 240:205–213
Kawahira H, Kodera Y, Hiki N, Takahashi M, Itoh S, Mitsumori N, Kawashima Y, Namikawa T, Inada T, Nakada K (2015) Optimal Roux‑en‑Y reconstruction after distal gastrectomy for early gastric cancer as assessed using the newly developed PGSAS‑45 scale. Surg Today 45:1307–1316
Nunobe S, Okaro A, Sasako M, Saka M, Fukagawa T, Katai H, Sano T (2007) Billroth 1 versus Roux-en-Y reconstructions: a quality-of-life survey at 5 years. Int J Clin Oncol 12:433–439
Inokuchi M, Kojima K, Yamada H, Kato K, Hayashi M, Motoyama K, Sugihara K (2013) Long-term outcomes of Roux-en-Y and Billroth-I reconstruction after laparoscopic distal gastrectomy. Gastric Cancer 16:67–73
Fukuhara K, Osugi H, Takada N, Takemura M, Higashino M, Kinoshita H (2002) Reconstructive procedure after distal gastrectomy for gastric cancer that best prevents duodenogastroesophageal reflux. World J Surg 26:1452–1457
Inoue K, Fuchigami A, Higashide S, Sumi S, Kogire M, Suzuki T, Tobe T (1992) Gallbladder sludge and stone formation in relation to contractile function after gastrectomy. A prospective study. Ann Surg 32:591–601
van der Mijle HC, Kleibeuker JH, Limburg AJ, Bleichrodt RP, Beekhuis H, van Schilfgaarde R (1993) Manometric and scintigraphic studies of the relation between motility disturbances in the Roux limb and the Roux-en-Y syndrome. Am J Surg 166:11–17
Gustavsson S, Ilstrup DM, Morrison P, Kelly KA (1988) Roux-Y stasis syndrome after gastrectomy. Am J Surg 155:490–494
Funding
The authors have not received Grant support or other forms of assistance.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Disclosures
Keisuke Okuno, MD, Masatoshi Nakagawa, MD, PhD, Kazuyuki Kojima, MD, PhD, Emi Kanemoto, MD, Kentaro Gokita, MD, Toshiro Tanioka, MD, and Mikito Inokuchi, MD, PhD have no financial conflicts of interest to disclose.
Rights and permissions
About this article
Cite this article
Okuno, K., Nakagawa, M., Kojima, K. et al. Long-term functional outcomes of Roux-en-Y versus Billroth I reconstructions after laparoscopic distal gastrectomy for gastric cancer: a propensity-score matching analysis. Surg Endosc 32, 4465–4471 (2018). https://doi.org/10.1007/s00464-018-6192-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00464-018-6192-2