Abstract
Background
Laparoscopic right hemicolectomy has become an acceptable treatment for right-sided colon cancer. Most centers use multiport laparoscopic right hemicolectomy extracorporeally (MRHE), whereas single-incision laparoscopic right hemicolectomy intracorporeally (SRHI) remains controversial. The aim of this study was to compare these two techniques using propensity score matching analysis.
Methods
We analyzed the data from 111 patients who underwent laparoscopic right hemicolectomy between December 2015 and December 2016. The propensity score was calculated according to age, gender, body mass index, the American Society of Anesthesiologists score, previous abdominal surgery, and D3 lymph node dissection. Postoperative pain was evaluated using a visual analogue scale (VAS) and postoperative analgesic use was an outcome measure.
Results
The length of skin incision in SRHI was significantly shorter than in MRHE [3 (3.5–6) versus 4 (3–6) cm, respectively; P = 0.007]. The VAS score on day 1 and day 2 after surgery was significantly less in SRHI than in MRHE [30 (10–50) versus 50 (20–69) on day 1, P = 0.037; 10 (0–50) versus 30 (0–70) on day 2, P = 0.029]. Significantly fewer patients required analgesia after SRHI on day 1 and day 2 after surgery [1 (0–3) versus 2 (0–4) on day 1, P = 0.024; 1 (0–2) versus 1 (0–4) on day 2, P = 0.035]. There were no significant differences in operative time, intraoperative blood loss, number of lymph nodes removed, and postoperative course between groups.
Conclusions
SRHI appears to be safe and technically feasible. Moreover, SRHI reduces the length of the skin incision and postoperative pain compared with MRHE.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Laparoscopic colectomy is now an acceptable treatment for colon cancer [1,2,3,4,5]. Currently, the safety and feasibility of single-incision laparoscopic colon cancer surgery compared with multiport laparoscopic have been demonstrated in several randomized controlled trials (RCT) [6,7,8] and meta-analyses [9, 10]. However, there is considerable controversy regarding the surgical procedure. For right hemicolectomy, Chen et al. have demonstrated there was no benefit in the short-term outcomes [11]. In contrast, Keshava et al. have shown a shorter extraction wound size and shorter length of hospital stay [12].
Recently, several meta-analyses have described the feasibility and safety of intracorporeal anastomosis after laparoscopic right hemicolectomy [13, 14]. However, the clinical outcomes for intracorporeal resection with single-incision laparoscopic colon cancer surgery have seldom been reported.
In our institution, single-incision laparoscopic colon cancer surgery with intracorporeal resection has been performed since December 2015. The goal of this study was to investigate the clinical outcomes associated with single-incision laparoscopic right hemicolectomy with intracorporeal resection.
Methods
Patients
The first single-incision laparoscopic right hemicolectomy with intracorporeal resection for cancer was performed in 2015. At that time, the procedure was indicated only for early-stage cancer. Gradually, it was expanded to more advanced stages of right-sided cancer. From December 2015 to December 2016, a total of 111 consecutive patients underwent laparoscopic colon cancer surgery for right-sided colon cancer in our institution. Of these, 88 laparoscopic right hemicolectomies with D3 lymphadenectomy were performed for cancers of the cecum as well as ascending and transverse colon, excluding patients undergoing resection combined with cholecystectomy, hepatectomy, hysterectomy, or gastrectomy. Exclusion criteria for laparoscopic surgery included bowel obstruction due to cancer that was not successfully treated preoperatively, invasion of cancer into adjacent organs that could not be resected laparoscopically, and withdrawal of informed consent. In this study, only one surgeon performed the single-incision laparoscopic intracorporeal resections, and three highly experienced laparoscopic surgeons carried out the conventional laparoscopic surgeries during the study period. All patients underwent comprehensive assessment with blood testing, serum carcinoembryonic antigen measurement, colonoscopy, pathologic confirmation, barium or air enema, computed tomography (CT), and chest X-ray before surgery. If tumor localization was unclear, preoperative colonoscopic India-ink tattooing and clipping were performed. Short-term outcomes were recorded. Postoperative pain was evaluated using a visual analogue scale (VAS), and histopathologic tumor node metastasis (TNM) staging (AJCC/UICC) was utilized. Postoperative analgesic use was taken as an outcome measure. Furthermore, the procedure for lymphadenectomy was determined based on the depth of tumor invasion at the time of preoperative diagnosis according to the Japanese Classification of Colorectal Carcinoma [15]. The laparoscopic no-touch isolation technique (i.e., the medial-to-lateral approach) was utilized whenever possible. For T4 cancer with invasion into adjacent structures, laparoscopic en bloc resection with a safe margin around the normal tissue was performed as usual. If technical difficulty was observed, conversion to open surgery was implemented at the discretion of the surgeon. Conversion was defined as any incision of more than 8 cm in length that was needed to complete or facilitate the procedure that could not be accomplished laparoscopically. The study was approved by the institutional ethics committee, and informed consent for the operation describing the details of the procedure and probable complications was obtained before surgery. In order to minimize differences that might be attributable to skin preparation, antibiotic prophylaxis, and surgical technique, standard procedures were followed in all patients. Twenty-four-hour postoperative analgesia was maintained by continuous infusion of 0.3–0.5 µg/kg/h fentanyl. Intravenous infusion of flurbiprofen and oral administration of loxoprofen were employed as additional analgesic.
Statistical analysis
Statistical analysis was performed using JMP 13 for Windows (SAS Institute, Inc., Cary, NC, USA). Student’s t test, Mann–Whitney U test, and the χχ2 test were used to compare continuous and categorical variables as appropriate, with two-sided P < 0.05 indicating statistical significance. One-to-one matching was performed without replacement using a caliper width of 0.2 standard deviation of the logit of the estimated propensity score [16]. Gender, age, body mass index (BMI), cardiovascular disease, cerebrovascular disease, diabetes mellitus, American Society Anesthesiology (ASA) classification, previous abdominal surgery (PAS), tumor max diameter, and D3 lymphadenectomy were selected as covariates. After propensity score matching (PSM), the two matched groups were handled as unpaired independent group. Lastly, multivariate analysis was performed using logistic regression.
Conventional laparoscopic procedures
Each patient was placed in the modified lithotomy position and administered general anesthesia. In conventional laparoscopic right hemicolectomy, a 12-mm subumbilical port was created to introduce the semi-flexible laparoscopic camera (LTFVH, Olympus, Tokyo, Japan), and additional ports were made in the right lower quadrant (5-mm port), suprapubic region (5-mm port), left lower quadrant (5-mm port), and epigastric region (5-mm port). Following mesocolic plane resection, the duodenum and pancreas were sufficiently exposed, and the feeding vessels were identified. Proximal ligation of the ileocecal, right colic (if necessary), and right branch of the root of the middle colic vessels was conducted, and lymphadenectomy was performed simultaneously with central vascular ligation (CVL) and complete mesocolic excision (CME) using medial-to-lateral approach. Mobilization was carried out from the hepatic flexure, and the umbilical port site was expanded to 3 to 5 cm. The bowel loop was delivered under a wound protector through the incision and separated from the marginal vessels. Then, the ileum and colon were resected using a linear stapler extracorporeally. Small holes were made in the walls of the ileum and colon, and another stapler was inserted into these holes to perform the side-to-side anastomosis. Lastly, the holes were resected using a final stapler. We used four cartridges for this functional end-to-end method. The stapled and parts of the double-stapled edges were reinforced with sutures.
Single-incision laparoscopic procedures
Single-incision laparoscopic right hemicolectomy was performed using the conventional laparoscopic instruments through an initial 2 to 2.5 cm incision in the umbilicus. Subsequently, an ALEXIS® wound retractor (Applied Medical, Rancho Santa Margarita, CA, USA) of XS size was installed at the umbilical wound. Then, a non-powdered surgical glove (5.5 inches) was placed on the wound retractor in an air-tight fashion, through which three 5-mm slim trocars were inserted into the tips of the glove’s thumb, middle, and small fingers. A laparoscopic camera was then inserted through the middle finger port. The ileum and transverse colon were resected intracorporeally using linear stapler through the tip of the glove’s ring finger. Suturing of each stump was also performed intracorporeally to prevent twisting of the bowel. After the specimen was extracted through the umbilical incision, anastomosis was performed extracorporeally using the same method (Fig. 1). Conversion was defined as any incision of more than 8 cm in length that was needed to complete or facilitate the procedure that could not be accomplished laparoscopically.
Postoperative follow-up
For follow-up, patients with stage I and II disease were tested for serum carcinoembryonic antigen levels (at 3-month intervals during the first year and at 6-month intervals thereafter), chest and abdomino-pelvic CT (at 6-month intervals), and colonoscopy (at 1-year intervals), in addition to routine outpatient visits. Patients with stage III disease underwent assessment of serum carcinoembryonic antigen levels (at 4-month intervals during the first 2 years and at 6-month intervals thereafter), as well as chest and abdomino-pelvic CT and colonoscopy at the same intervals, in addition to routine outpatient visits. In addition, patients with stage III disease received adjuvant chemotherapy of 5-fluorouracil plus leucovorin according to the standards of care.
Results
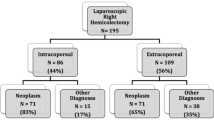
Eighty-eight patients underwent laparoscopic right hemicolectomies with D3 lymphadenectomy for right-sided colon cancer in our institution. In total, 68 patients underwent conventional multiport laparoscopic right hemicolectomy extracorporeally (MRHE) and the remaining 20 patients underwent single-incision laparoscopic right hemicolectomy intracorporeally (SRHI). Characteristics, comorbidities, and risk factors did not differ significantly between the MRHE and SRHI group. Patient backgrounds in both groups were closely balanced by the PSM which resulted in 15 matched pairs (Table 1). Moreover, characteristics regarding the tumor, tumor max diameter, pathological T (pT) category, and tumor classification did not differ significantly between the MRHE and SRHI group after PSM (Table 2).
Data regarding the number of lymph nodes, operative time, blood loss, oral wedge (OW), anal wedge (AW), length of skin incision, VAS scores (day 0 to 3), anastomosis, and number of analgesics (day 0 to 3) were collected in a database (Table 3). There were no significant differences in the number of lymph nodes removed, operative time, blood loss, OW, or AW when comparing the two groups. The length of skin incision (4.0 versus 3.0 cm; P = 0.007) was shorter in the SRHI group. The VAS scores on day 1 and day 2 after surgery were significantly lower in the SRHI group (50 versus 30 on day 1, P = 0.037; 30 versus 10 on day 2, P = 0.029). The number of analgesics used was also significantly lower in the SRHI group (2.7 versus 1.3 times on day 1, P = 0.024; 1.4 versus 0.6 on day 2, P = 0.035). The number of trocars was lower in the SRHI group as well (3 ports versus 5 ports).
Table 4 summarizes the morbidity in each group. There were no perioperative deaths, and there was no significant difference in morbidity when comparing the two groups. Moreover, no significant differences were observed in the postoperative course or in the rate of incisional hernia at the umbilicus.
Discussion
Several studies have demonstrated that single-incision laparoscopic colon cancer surgery can achieve favorable short-term outcomes as a minimally invasive surgery [6,7,8,9,10]. Additionally, oncological long-term outcomes are similar after single-incision and multiport laparoscopic surgery for cancer [17,18,19]. However, there is significant bias in these studies due to the heterogeneity of the indications for the tumor location and use of instruments. Based on the tumor location, the characteristics of right-sided colon cancer are older and more often female, and these tumors tend to involve bulky, exophytic, and polypoid lesions growing into the colon lumen [20,21,22]. Furthermore, right-sided colon cancer is often associated with a more advanced N stage, greater tumor size, more frequent poorly differentiated tumors, and worse survival outcomes than left-sided colon cancer after curative resection [23]. Therefore, we suggest that the length of the skin incision should not be compared between right-sided and left-sided colon cancer.
Regarding other minimally invasive techniques, several meta-analyses have described that intracorporeal resection and anastomosis in laparoscopic right hemicolectomy are associated with faster bowel recovery, decreased use of analgesics, reduced short-term morbidity, and shorter duration of hospital stay [13, 14]. By performing an intracorporeal anastomosis, the incision for extraction can be smaller, which has been shown to be associated with less pain and lower infection rate. Thus, single-incision laparoscopic right hemicolectomy with intracorporeal anastomosis may be a more advanced minimally invasive surgical technique. However, this procedure is technically limited due to inline viewing, insufficient traction, and instrument crowding, which can increase the amount of stress experienced by surgeons. In addition, the necessity for intraperitoneal tomies into a contaminated transverse colon and ileum, which have proved technically difficult, could lead to a theoretical increase in intraabdominal infections. Thus, we have performed single-incision extracorporeal anastomosis. To the best of our knowledge, the present study is the first report of its kind to evaluate the clinical impact of SRHI compared to MRHE for the same indication and using the same straight laparoscopic instruments, as well as incorporating PSM analysis.
The short-term outcomes and postoperative complications were similar after MRHE and SRHI in the present study. With the exception of the total skin incision length, VAS pain scale, and number of analgesics, there were no significant differences between the MRHE and SRHI groups for any of the studied variables. Evidently, the four smaller incisions in MRHE are absent in the SRHI procedure, thus any pain from these wounds is absent in SRHI. Leung et al. have demonstrated that intracorporeal resection and anastomosis require a smaller incision, potentially leading to less postoperative pain in RCT for laparoscopic left-sided colectomy [24]. Perhaps more importantly, since the incision is made only for specimen extraction in the intracorporeal technique, it has the benefit of less retraction or tension placed on the wound, than in trying to introduce a large hand or forearm into the abdomen or to externalize the specimen for resection or anastomosis [25]. There was no conversion to MRHE in the SRHI group. Furthermore, two meta-analyses revealed a shorter hospital stay following single-incision laparoscopic colectomy [9, 10]. Spanjersberg et al. reported that the length of postoperative stay is largely dependent on the type of postoperative management [26]. According to the postoperative course in our study, no differences were evident.
In the field of surgical oncology, better cosmesis and less postoperative pain should be provided with acceptable short-term outcomes and certain oncologic clearance [27]. From this viewpoint, there were no differences in the number of lymph nodes dissected or the length of the resection margin between the MRHE and SRHI groups.
Hoyuela et al. demonstrated that the long-term rate of trocar-site hernias is probably higher after single-incision laparoscopic colectomy, especially if the incision is located at the umbilicus [9]. In single-incision laparoscopic cholecystectomy, several studies have established umbilical hernia rates of 2.9–25.9% [28,29,30]. Buckley et al. reported that both pre-existing hernia and BMI were significant independent risk factors after single-incision laparoscopy [31]. The total incisional hernia rate was 10% in the present study, which is consistent with the incisional hernia rates obtained in previous reports. Two patients had an incisional hernia at the umbilicus after SRHI, although both had pre-existing hernia. Comparing the two groups, there was no significant difference in the rate of incisional hernia.
In conclusion, SRHI appears to be safe and feasible and provides acceptable short-term outcomes when compared to MRHE. However, there is insufficient evidence to recommend its widespread use in place of MRHE. There may be other potential benefits associated with SRHI (cosmesis, pain control, patient satisfaction, and cost-effectiveness), but these remain to be proven objectively. Further investigations are necessary to evaluate the oncological long-term outcomes and specimen extraction site (e.g., Pfannenstiel). The limitations of the present data are that the study was performed at a single institution in Japan and were not generated in a prospective manner. In addition, single-incision laparoscopic surgery technique is not yet popular due to its long learning curve. However, the demand for a less invasive procedure is expected to increase. The advantages of single-incision surgery and intracorporeal resection should prove beneficial to both surgeons and patients. Therefore, the SHRI technique should be considered for use as a standard procedure for single-incision right hemicolectomy. Furthermore, multicenter studies are needed to more clearly define the advantages of SHRI over MRHE.
References
Lacy AM, Gracia-Valdecasas JC, Delgango S, Castells A, Taura P, Pique JM, Visa J (2002) Laparoscopy-assisted colectomy versus open colectomy for treatment of non-metastatic colon cancer: a randomized trial. Lancet 359:2224–2229
Clinical Outcomes of Surgical Therapy Study Group (2007) Laparoscopic colectomy for cancer is not inferior to open surgery based on 5-year data from the COST study group trial. Ann Surg 246:655–664
The Colon Cancer Laparoscopic or Open Resection Study Group (2009) Survival after laparoscopic surgery versus open surgery for colon cancer: long-term outcome of a randomized clinical trial. Lancet Oncol 10:44–52
Jayne DG, Thorpe HC, Copeland J, Quirke P, Brown JM, Guillou PJ (2010) Five-year follow-up of the medical research council CLASICC trial of laparoscopically assisted versus open surgery for colorectal cancer. Br J Surg 97:1638–1645
Yamamoto S, Inomata M, Katayama H, Mizusawa J, Etoh T, Konishi F, Sugihara K, Watanabe M, Moriya Y, Kitano S, Japan Clinical Oncology Group Colorectal Cancer Study Group (2014) Short-term surgical outcomes from a randomized controlled trial to evaluate laparoscopic and open D3 dissection for stage II/ III colon cancer: Japan Clinical Oncology Group Study JCOG 0404. Ann Surg 260:23–30
Huscher CG, Mingoli A, Sgarzini G, Mereu A, Binda B, Brachini G, Trombetta S (2012) Standard laparoscopic versus single-incision laparoscopic colectomy for cancer: early result of a randomized prospective study. Am J Surg 204:115–120
Poon JTC, Cheung CW, Fan JK, Lo OS, Law WL (2012) Single-incision versus conventional laparoscopic colectomy for colonic neoplasm: a randomized, controlled trial. Surg Endosc 26:2729–2734
Watanabe J, Ota M, Fujii S, Suwa H, Ishibe A, Endo I (2016) Randomized clinical trial of single-incision versus multiport laparoscopic colectomy. Br J Surg 103:1276–1281
Hoyuela C, Juvany M, Carvajal F (2017) Single-incision laparoscopy versus standard laparoscopy for colorectal surgery: a systematic review and meta-analysis. Am J Surg 214:127–140
Podda M, Saba A, Porru F, Pisaynu A (2016) Systematic review with meta-analysis of studies comparing single-incision laparoscopic colectomy and multiport laparoscopic colectomy. Surg Endosc 30:4697–4720
Chen WT, Chang SC, Chiang HC, Lo WY, Jeng LB, Wu C, Ke TW (2011) Single-incision laparoscopic versus conventional laparoscopic right hemicolectomy: a comparison of short-term surgical results. Surg Endosc 25:1887–1892
Keshava A, Young CJ, Richardson GL, De-Loyde K (2013) A historical comparison of single incision and conventional multiport laparoscopic right hemicolectomy. Colorectal Dis 15:e618–e622
Feroci F, Lenzi E, Garzi A, Vannucchi A, Cantafio S, Scatizzi (2013) Intracorporeal versus extracorporeal anastomosis after laparoscopic right hemicolectomy for cancer: a systematic review and meta-analysis. Int J Colorectal Dis 28:1177–1186
Oostendorp SV, Elfrink A, Borstlap W, Schoonmade L, Sietses C, Meijerink J, Tuynman J (2017) Intracorporeal versus extracorporeal anastomosis in right hemicolectomy: a systematic review and meta-analysis. Surg Endosc 31:64–77
Japanese Society for Cancer of the Colon and Rectum (2009) The guidelines for therapy of colorectal cancer. Kanehara Shuppan, Tokyo
Austin PC (2009) Some methods of propensity-score matching had superior performance to others: results of an empirical investigation and Monte Carlo simulations. Biom J 51:171–184
Kim CW, Cho MS, Baek SJ, Hur H, Min BS, Kang J, Baik SH, Lee KY, Kim NK (2015) Oncologic outcomes of single-incision versus conventional laparoscopic anterior resection for sigmoid colon cancer: a propensity-score matching analysis. Ann Surg Oncol 22:924–930
Yun JA, Yun SH, Park YA, Huh JW, Cho YB, Kim HC, Lee WY (2016) Oncologic outcomes of single-incision laparoscopic surgery compared with conventional laparoscopy for colon cancer. Ann Surg 263:973–978
Katsuno G, Fukunaga M, Nagakari K, Yoshikawa S, Azuma D, Kohama S (2016) Short-term and long-term outcomes of single-incision versus multi-incision laparoscopic resection for colorectal cancer: a propensity-score-matched analysis of 214 cases. Surg Endosc 30:1317–1325
Saltzstein SL, Behling CA (2007) Age and time as factors in the left to right shift of the subsite of colorectal adenocarcinoma: a study of 213,383 cases from the California Cancer Registry. J Clin Gastroenterol 41:173–177
Powell AG, Wallance R, McKee RF, Anderson JH, Going JJ, Edwards J, Horgan PG (2012) The relationship between tumor site, clinicopathological characteristics and cancer-specific survival in patients undergoing surgery for colorectal cancer. Colorectal Dis 14:1493–1499
Benedix F, Kube R, Mayer F, Schmidt U, Gastinger I, Lippert H, Colon/Rectum Carcinomas (Primary Tumor) Study Group (2010) Comparison of 17,641 patients with right- and left-sided colon cancer: differences in epidemiology, perioperative course, histology, and survival. Dis Colon Rectum 53:57–64
Lim DR, Kuk JK, Kim T, Shin EJ (2017) Comparison of oncological outcomes of right-sided colon cancer versus left-sided colon cancer after curative resection: which side is better outcome? Medicine 96:e8241
Leung AL, Cheung HY, Fok BK, Chung CC, Li MK, Tang CN (2013) Prospective randomized trial of hybrid NOTES colectomy versus conventional laparoscopic colectomy for left-sided colonic tumors. World J Surg 37:2678–2682
Grams J, Tong W, Greenstein AJ, Salky B (2010) Comparison of intracorporeal versus extracorporeal anastomosis in laparoscopic-assisted hemicolectomy. Surg Endosc 24:1886–1891
Spanjersberg WR, Reuings J, Keus F, van Laarhoven CJ (2011) Fast track surgery versus conventional recovery strategies for colorectal surgery. Cochrane Database Syst Rev 2:CD007635
Takemasa I, Uemura M, Nishimura J, Mizushima T, Yamamoto H, Ikeda M, Sekimoto M, Doki Y, Mori M (2014) Feasibility of single-site laparoscopic colectomy with complete mesocolic excision for colon cancer: a prospective case-control comparison. Surg Endosc 28:1110–1118
Agaba EA, Rainville H, Ikedilo O, Vemulapali P (2014) Incidence of port-site incisional hernia after single-incision laparoscopic surgery. JSLS 18:204–210
Marks JM, Phillips MS, Tacchino R, Roberts K, Onders R, DeNoto G, Gecelter G, Rubach E, Rivas H, Islam A, Soper N, Paraskeva P, Rosemurgy A, Ross S, Shah S (2013) Single-incision laparoscopic cholecystectomy is associated with improved cosmesis scoring at the cost of significantly higher hernia rates: 1-year results of a prospective randomized, multicenter, single-blinded trial of traditional multiport laparoscopic cholecystectomy vs single-incision laparoscopic cholecystectomy. J Am Coll Surg 216:1037–1047
Comajuncosas J, Hermoso J, Gris P, Jimeno J, Orbeal R, Vallverdu H, Lopez Negre JL, Urgelles J, Estalella L, Pares D (2014) Risk factors for umbilical trocar site incisional hernia in laparoscopic cholecystectomy: a prospective 3-year follow-up study. Am J Surg 207:1–6
Buckley FP 3rd, Vassaur HE, Jupiter DC, Crosby JH, Wheeless CJ, Vassaur JL (2016) Influencing factors for port-site hernias after single-incision laparoscopy. Hernia 20:729–733
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Disclosures
Drs. M. Yamamoto, M. Asakuma, K. Tanaka, S. Masubuchi, M. Ishii, W. Osumi, H. Hamamoto, J. Okuda, and K. Uchiyama have no conflicts of interest or financial ties to disclose.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Yamamoto, M., Asakuma, M., Tanaka, K. et al. Clinical impact of single-incision laparoscopic right hemicolectomy with intracorporeal resection for advanced colon cancer: propensity score matching analysis. Surg Endosc 33, 3616–3622 (2019). https://doi.org/10.1007/s00464-018-06647-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00464-018-06647-0