Abstract
Background
Laparoscopic surgery has been widely accepted for the treatment of colorectal cancer; however, long-term outcomes in elderly patients remain controversial. The midterm results of a randomized trial comparing open surgery with laparoscopic surgery in elderly patients with colorectal cancer are presented.
Methods
This was a randomized trial comparing open surgery with laparoscopic surgery in elderly patients with colorectal cancer. The primary outcome was complication rate, and secondary outcomes included 3-year recurrence-free survival and overall survival. A total of 200 patients were randomly assigned to open surgery or laparoscopic surgery between 2008 and 2012. The main study objective was to compare the midterm outcomes of open surgery with those of laparoscopic surgery in elderly patients with colorectal cancer. This trial is registered with Clinical Trials.gov (NCT01862562).
Results
There were no differences between the laparoscopic surgery group and open surgery group in the 3-year overall survival rate (91.5% for laparoscopic surgery vs. 90.6% for open surgery, p = 0.638) or the 3-year recurrence-free survival rate (84.8% for laparoscopic surgery vs. 88.2% for open surgery, p = 0.324). The local recurrence rate was significantly higher in the laparoscopic surgery group than in the open surgery group in rectal cancer (13.8% for laparoscopic surgery vs. 0% for open surgery, p = 0.038). In subgroup analysis according to tumor location, there were no significant differences in the 3-year overall survival rate or 3-year recurrence-free survival rate between the two treatment groups.
Conclusion
The midterm outcomes of laparoscopic surgery are similar to those of open surgery in elderly patients with colorectal cancer.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Colorectal cancer is the second most common cancer in both sexes in Western countries, and more than 70% of the patients are 65 years or older [1]. In Japan, colorectal cancer ranked as the second most common cancer in women and the fourth most common cancer in men in 2015 [2]. Surgical resection of colorectal cancer remains the only curative treatment. During the past decade, large randomized trials have demonstrated the oncological safety and effectiveness of laparoscopic surgery as compared with conventional open surgery in patients with colorectal cancer [3 –5]. In Japan, the Japan Clinical Oncology Group (JCOG) conducted a randomized trial comparing laparoscopic surgery with conventional open surgery in patients with advanced colon and rectosigmoid cancer. However, patients 75 years or older were not included in that study [6]. Elderly patients generally have higher medical comorbidity rates and morbidity rates than younger patients [7, 8]. Few studies have compared the surgical and oncological outcomes of laparoscopic surgery with those of open surgery in this age group, and most have been observational [9]. We previously performed a randomized controlled study comparing open surgery with laparoscopic surgery in only elderly patients and reported the short-term outcomes [9]. In that study, the duration of surgery was significantly longer, and the blood loss was significantly less in the laparoscopic surgery group than in the open surgery group. Furthermore, the laparoscopic surgery group had a significantly lower all-grade complication rate, especially in patients with colon cancer. We concluded that the short-term results of laparoscopic surgery, apart from the duration of surgery, were excellent. Laparoscopic surgery was thus considered an effective procedure for elderly patients with colorectal cancer (especially colon cancer) [9].
We now report the 3-year follow-up data, including the secondary endpoints of recurrence-free survival (RFS) and overall survival (OS), in elderly patients with colorectal cancer.
Materials and methods
Patients
This was a randomized controlled trial performed in a single institution, Yokohama City University Medical Center, Yokohama, Japan. A total of 200 elderly patients (142 with colonic cancer and 58 with rectal cancer) were randomly assigned to open surgery or laparoscopic surgery between August 2008 and August 2012. The inclusion criteria included an age of 75 years or older, a histologically confirmed diagnosis of adenocarcinoma, a clinical stage of up to T4a tumors, any N stage, no evidence of metastasis (M0), and elective surgery. The details of the treatment protocol, surgical procedures, and justification for the sample size have been reported previously [9]. The protocol of this trial was approved by the ethics committee of Yokohama City University Medical Center.
Randomization, treatment allocation, and blinding
Written informed consent was obtained from all patients. After agreement of the patients to participate in the study was confirmed, the patients were randomly assigned to receive laparoscopic surgery or open surgery. A randomization schedule was created using a random number generator and stratified according to site. To balance the operative backgrounds between the laparoscopic surgery group and the open surgery group, the patients were stratified according to tumor location (right colon, left colon, or rectum). Patients with transverse colon cancer were allocated to the right colon group. Blinding could not be performed because of the obvious difference in the surgical procedure.
Follow-up
The follow-up schedule was specified according to disease stage. Patients with stage 0 or I disease underwent outpatient examinations, including tumor marker measurements and computed tomography (CT) of the chest, abdomen, and pelvis, once a year for 5 years. Patients with stage II or IIIA disease underwent CT and tumor marker measurements every 6 months for the first 2 years, followed by once a year from years 3 to 5. Patients with stage IIIB or IIIC disease underwent CT and tumor marker measurements every 4 months for the first 2 years, followed by every 6 months from years 3 to 5.
Statistical analysis
Secondary endpoints were 3-year RFS and 3-year OS. We estimated that a sample size of 200 patients would provide a power of higher than 80% to detect a difference between the groups on analysis using a two-sided Chi-square test with a type I error rate of 0.05, when the actual complication rates were 20% for laparoscopic surgery and 40% for open surgery.
Patients’ baseline characteristics were summarized as numbers and percentages and were compared between groups by means of Chi-square tests. Recurrence rates at various sites (liver, lung, peritoneal lymph nodes, distant lymph nodes, local recurrence, others) were also compared using Chi-square tests. The 3-year RFS and 3-year OS were compared using Kaplan–Meier analyses, and statistical significance was determined by log-rank tests. In all analyses, p < 0.05 was considered to indicate statistical significance. All analyses were performed using IBM SPSS software, version 21 (SPSS Inc., Chicago, IL, USA).
The present study is registered with Clinical Trials.gov (NCT01862562).
Results
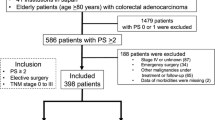
A CONSORT diagram summarizing the allocation of patients during the study is shown in Fig. 1. Seven patients in the open surgery group and two patients in the laparoscopic surgery group were excluded because metastatic disease was diagnosed at surgery. One patient in the open surgery group in whom malignant lymphoma was diagnosed postoperatively was also excluded from analysis.
The two groups were balanced with respect to baseline characteristics and pathological disease stage (Table 1). No patient received preoperative radiotherapy or chemotherapy. Adjuvant chemotherapy was given to 10 (10.8%) patients in the open surgery group and 16 (16.3%) patients in the laparoscopic surgery group. All patients received oral 5-fluorouracil derivatives only. No patient received oxaliplatin- or irinotecan-based regimens.
Overall survival
The 3-year OS is shown in Fig. 2. The median follow-up time of OS was 43 months (range, 4–74 months). The 3-year OS rate in the study group as a whole was 91.1%. The 3-year OS rate in the laparoscopic surgery group did not differ significantly than that in the open surgery group (91.5% for laparoscopic surgery vs. 90.6% for open surgery, p = 0.638).
The 3-year OS rate was 93.8% in patients with colon cancer and 84.7% in patients with rectal cancer. In colon cancer, the 3-year OS rate was 93.5% for open surgery versus 93.9% for laparoscopic surgery (p = 0.901). In rectal cancer, the 3-year OS rate was 83.1% for open surgery versus 85.7% for laparoscopic surgery (p = 0.557). When the patients were analyzed according to disease stage, there were no significant differences in the 3-year OS rate between the treatment groups (stage I: 96.3% for laparoscopic surgery vs. 100% for open surgery, p = 0.845; stage II: 91.4% for laparoscopic surgery vs. 87.4% for open surgery, p = 0.553; stage III: 85.5% for laparoscopic surgery vs. 90% for open surgery, p = 0.319). It is important to note that the stage-specific comparisons were underpowered.
Recurrence-free survival
The 3-year RFS is shown in Fig. 3. The median follow-up time of RFS was 42.5 months (range, 3–74 months). The 3-year RFS rate in the study group as a whole was 86.6%. The 3-year RFS did not differ significantly between the laparoscopic surgery group and the open surgery group (84.8% for laparoscopic surgery vs. 88.2% for open surgery, p = 0.324).
The 3-year RFS rate was 91.5% in patients with colon cancer and 76.9% in patients with rectal cancer. The 3-year RFS rate did not differ significantly between the two surgical techniques in patients with colon cancer (91.5% for open surgery vs. 89.6% for laparoscopic surgery, p = 0.73) or in patients with rectal cancer (80.5% for open surgery vs. 71.9% for laparoscopic surgery, p = 0.212). When the patients were analyzed according to disease stage, there were no differences in 3-year RFS between the treatment groups (stage I: 100% for laparoscopic surgery vs. 95% for open surgery, p = 0.845; stage II: 91.3% for laparoscopic surgery vs. 91% for open surgery, p = 0.553; stage III: 60.9% for laparoscopic surgery vs. 76.8% for open surgery, p = 0.319).
Recurrence
The overall recurrence rate at 3 years was 11.9% in the open surgery group and 17.3% in the laparoscopic surgery group. The recurrence sites in each group are shown in Table 2. The local recurrence rate was 2.1% and is presented separately for the open surgery group and laparoscopic surgery group in Table 3. The local recurrence rate was significantly higher in the laparoscopic surgery group than in the open surgery group (4.1% for laparoscopic surgery vs. 0% for open surgery, p = 0.05). All local recurrences in the laparoscopic surgery group occurred in patients with rectal cancer. Four patients in the laparoscopic surgery group had local recurrence. One had a T2 tumor and the site of recurrence was anastomotic; recurrence was apparently caused by tumor cell implantation. The other three patients with recurrence had T4 tumors. The overall distant recurrence rate at 3 years was 19.7% in the study group as a whole and is presented separately for the open surgery group and laparoscopic surgery group in Table 3. There were no significant differences in the distant recurrence rates at 3 years between the two groups.
Discussion
To our knowledge, our study is the first randomized controlled trial to compare open surgery with laparoscopic surgery in only elderly patients. Our trial demonstrated that the 3-year RFS and 3-year OS were similar for laparoscopic surgery and conventional open surgery in elderly patients with colorectal cancer.
Laparoscopic colorectal surgery has been widely accepted for the management of colorectal cancer. Several studies and our previous study have demonstrated that laparoscopic surgery for colorectal disease in elderly patients has short-term benefits, such as earlier recovery of bowel function and a shorter hospital stay [9 – 13]. A few studies have reported the long-term outcomes of laparoscopic surgery for colorectal cancer in the elderly [14 – 16]. A large multicenter case–control study conducted by Niitsu et al. reported that the 3-year OS, disease-free survival, and cancer-specific survival did not differ between laparoscopic surgery and open surgery in patients with colorectal cancer who were 80 years or older [14]. Moon et al. also found no difference in OS or RFS between laparoscopic surgery and open surgery on propensity-matched analysis [16]. The results of these studies indicated that laparoscopic surgery is comparable to open surgery in terms of long-term outcomes in elderly patients with colorectal cancer. However, these previous trials were not randomized controlled studies focusing exclusively on elderly patients. Our randomized controlled trial demonstrated that the 3-year RFS and 3-year OS were similar for laparoscopic surgery and open surgery in elderly patients with colorectal cancer.
In our study, secondary endpoints were 3-year RFS and 3-year OS. The 5-year OS rate is appropriate to evaluate when determining whether laparoscopic surgery influences survival, which is the true target of the surgical treatment of malignant, but potentially curable colorectal cancer. However, there are many other potential causes of death, such as other diseases, in elderly patients. We therefore decided that the 3-year RFS rate was an appropriate secondary endpoint.
In the survival analysis, 3-year RFS and OS did not differ significantly between open surgery and laparoscopic surgery in elderly patients with colorectal cancer. In addition, because recurrence rates are known to vary according to the location of the primary tumor, we analyzed outcomes after stratifying the patients according to whether they had colon cancer or rectal cancer. Our results showed no difference in the 3-year RFS or OS between open surgery and laparoscopic surgery in either colon cancer or rectal cancer. In addition, there were no significant differences between the treatment groups in 3-year RFS or OS on subgroup analysis according to disease stage. In the famous, large CLASICC and COLOR randomized controlled trials, the 3-year RFS rates were 67.7 and 76.2% for open surgery and 66.3 and 74.2% for laparoscopic surgery, respectively. The 3-year OS rates were, respectively, 66.7 and 84.2% for open surgery and 68.4 and 81.8% for laparoscopic surgery [5, 17]. The midterm outcomes in our study were better than those obtained in these previous Western trials.
The Japanese standard procedure for colectomy in patients with rectal cancer involves complete tumor resection with extended D2/D3 lymph node dissection, including the pericolic, intermediate, and mostly central lymph nodes [18], and total mesorectal excision [19]. Our previous study revealed acceptable short-term outcomes in elderly patients who underwent standard Japanese surgical procedures, and favorable midterm outcomes were obtained in the present study.
We also analyzed recurrence patterns in both treatment groups. Previous large randomized trials found no significant differences in distant, local, or wound/port-site recurrence between open surgery and laparoscopic surgery [3, 5]. However, our trial showed that open surgery was associated with a lower risk of local recurrence than laparoscopic surgery in patients with rectal cancer.
The CLASICC trial reported that the rate of circumferential resection margin (CRM) positivity was higher in patients undergoing laparoscopic anterior resection (i.e., 6.3% for open surgery vs. 12.4% for laparoscopic surgery), whereas local recurrence rate did not differ significantly [3 , 20]. The ACOSOG Z6051 randomized trial comparing open surgery with laparoscopic surgery in patients with stage II or III rectal cancer showed that the rate of a negative CRM was 87.9% for laparoscopic resection and 92.3% for open resection [21]. The findings did not support the use of laparoscopic resection in patients with stage II or III rectal cancer. In our study, the rate of circumferential margin involvement did not differ significantly between open surgery and laparoscopic surgery (4.0% for open surgery vs. 3.0% for laparoscopic surgery) [9]. However, some patients with local recurrence after laparoscopic surgery had T4 tumors. Therefore, the CRM of these patients may have been too close to the primary tumor. In our study, no patient received preoperative radiotherapy or chemotherapy. In Japan, extended surgery including lateral pelvic node dissection (LPND) without preoperative chemoradiotherapy (CRT) has been the standard surgical procedure for locally advanced rectal cancer [22, 23]. Sugihara et al. suggested that LPND might reduce local recurrence and improve survival rates [24]. However, there are no large randomized trials comparing preoperative CRT + TME with TME + LPND. In our study, some patients with T4 tumors had local recurrence. In such patients, preoperative CRT might be necessary to obtain wide surgical margins. In rectal cancer, we should carefully determine the indications of laparoscopic surgery.
The present study had several limitations. First, our study was underpowered to conclude that laparoscopic surgery was noninferior to open surgery in elderly patients with colorectal cancer, because the sample size was based on the expected complication rates. Furthermore, because we included patients with colon cancer as well as those with rectal cancer, this study also has the potential to be underpowered in this respect. Second, our study was small and conducted at a single hospital. A larger, multicenter randomized trial is needed to confirm the results of survival analysis.
In conclusion, our study is the first randomized controlled trial to show that the midterm outcomes of laparoscopic surgery are similar to those of open surgery in elderly patients with colorectal cancer.
References
Group CCC (2000) Surgery for colorectal cancer in elderly patients: a systematic review. The Lancet 356(9234):968–974
National Cancer Center Japan PCSRCf, Cancer Control and Information Services CIS.
Green BL, Marshall HC, Collinson F, Quirke P, Guillou P, Jayne DG, Brown JM (2013) Long-term follow-up of the Medical Research Council CLASICC trial of conventional versus laparoscopically assisted resection in colorectal cancer. Br J Surg 100(1):75–82
Clinical Outcomes of Surgical Therapy Study Group (2004) A comparison of laparoscopically assisted and open colectomy for colon cancer. N Eng J Med; 350(20): 2050–2059
Buunen M, Veldkamp R, Hop WC, Kuhry E, Jeekel J, Haglind E, Pahlman L, Cuesta MA, Msika S, Morino M, Lacy A, Bonjer HJ (2009) Survival after laparoscopic surgery versus open surgery for colon cancer: long-term outcome of a randomised clinical trial. Lancet Oncol 10(1):44–52
Kitano S, Inomata M, Sato A, Yoshimura K, Moriya Y (2005) Randomized controlled trial to evaluate laparoscopic surgery for colorectal cancer: Japan Clinical Oncology Group Study JCOG 0404. Jpn J Clin Oncol 35(8):475–477
Alves A, Panis Y, Mathieu P, Mantion G, Kwiatkowski F, Slim K. (2005) Postoperative mortality and morbidity in French patients undergoing colorectal surgery: results of a prospective multicenter study. Archives Surg 140(3): 278–283, discussion 284.
Duron JJ, Duron E, Dugue T, Pujol J, Muscari F, Collet D, Pessaux P, Hay JM (2011) Risk factors for mortality in major digestive surgery in the elderly: a multicenter prospective study. Ann Surg 254(2):375–382
Fujii S, Ishibe A, Ota M, Yamagishi S, Watanabe K, Watanabe J, Kanazawa A, Ichikawa Y, Oba M, Morita S, Hashiguchi Y, Kunisaki C, Endo I (2014) Short-term results of a randomized study between laparoscopic and open surgery in elderly colorectal cancer patients. Surg Endosc 28(2):466–476
Vignali A, Di Palo S, Tamburini A, Radaelli G, Orsenigo E, Staudacher C (2005) Laparoscopic vs. open colectomies in octogenarians: a case-matched control study. Dis Colon Rectum 48(11):2070–2075
Frasson M, Braga M, Vignali A, Zuliani W, Di Carlo V (2008) Benefits of laparoscopic colorectal resection are more pronounced in elderly patients. Dis Colon Rectum 51(3):296–300
Lian L, Kalady M, Geisler D, Kiran RP (2010) Laparoscopic colectomy is safe and leads to a significantly shorter hospital stay for octogenarians. Surg Endosc 24(8):2039–2043
Vallribera Valls F, Landi F, Espin Basany E, Sanchez Garcia JL, Jimenez Gomez LM, Marti Gallostra M, Salgado Cruz L, Armengol Carrasco M (2014) Laparoscopy-assisted versus open colectomy for treatment of colon cancer in the elderly: morbidity and mortality outcomes in 545 patients. Surg Endosc 28(12):3373–3378
Niitsu H, Hinoi T, Kawaguchi Y, Ohdan H, Hasegawa H, Suzuka I, Fukunaga Y, Yamaguchi T, Endo S, Tagami S, Idani H, Ichihara T, Watanabe K, Watanabe M. (2015) Laparoscopic surgery for colorectal cancer is safe and has survival outcomes similar to those of open surgery in elderly patients with a poor performance status: subanalysis of a large multicenter case-control study in Japan. J Gastroenterol 51(1):43–54
Tokuhara K, Nakatani K, Ueyama Y, Yoshioka K, Kon M (2016) Short- and long-term outcomes of laparoscopic surgery for colorectal cancer in the elderly: a prospective cohort study. Int J Surg 27:66–71
Moon SY, Kim S, Lee SY, Han EC, Kang SB, Jeong SY, Park KJ, Oh JH. (2016) Laparoscopic surgery for patients with colorectal cancer produces better short-term outcomes with similar survival outcomes in elderly patients compared to open surgery. Cancer med 5(6):1047–1054
Jayne DG, Guillou PJ, Thorpe H, Quirke P, Copeland J, Smith AM, Heath RM, Brown JM, Group UMCT (2007) Randomized trial of laparoscopic-assisted resection of colorectal carcinoma: 3-year results of the UK MRC CLASICC Trial Group. Jclin oncol 25(21):3061–3068
West NP, Kobayashi H, Takahashi K, Perrakis A, Weber K, Hohenberger W, Sugihara K, Quirke P (2012) Understanding optimal colonic cancer surgery: comparison of Japanese D3 resection and European complete mesocolic excision with central vascular ligation. J clin oncol 30(15):1763–1769
Heald RJ (1979) A new approach to rectal cancer. Br J Hosp Med 22(3):277–281
Guillou PJ, Quirke P, Thorpe H, Walker J, Jayne DG, Smith AMH, Heath RM, Brown JM (2005) Short-term endpoints of conventional versus laparoscopic-assisted surgery in patients with colorectal cancer (MRC CLASICC trial): multicentre, randomised controlled trial. The Lancet 365(9472):1718–1726
Fleshman J, Branda M, Sargent DJ, Boller AM, George V, Abbas M, Peters WR Jr, Maun D, Chang G, Herline A, Fichera A, Mutch M, Wexner S, Whiteford M, Marks J, Birnbaum E, Margolin D, Larson D, Marcello P, Posner M, Read T, Monson J, Wren SM, Pisters PW, Nelson H (2015) Effect of laparoscopic-assisted resection vs open resection of stage II or III rectal cancer on pathologic outcomes: The ACOSOG Z6051 randomized clinical trial. Jama 314(13):1346–1355
Moriya Y, Sugihara K, Akasu T, Fujita S (1997) Importance of extended lymphadenectomy with lateral node dissection for advanced lower rectal cancer. World J Surg 21(7):728–732
Takahashi T, Ueno M, Azekura K, Ohta H (2000) Lateral node dissection and total mesorectal excision for rectal cancer. Dis Colon Rectum 43(10 Suppl):S59–S68
Sugihara K, Kobayashi H, Kato T, Mori T, Mochizuki H, Kameoka S, Shirouzu K, Muto T (2006) Indication and benefit of pelvic sidewall dissection for rectal cancer. Dis Colon Rectum 49(11):1663–1672
Author contributions
Ishibe Atsushi and Fujii Shoichi contributed to the study conception and design. Ota Mitsuyoshi, Yusuke Suwa, Shinsuke Suzuki, Hirokazu Suwa, Jun Watanabe, and Kazuteru Watanabe contributed to data acquisition. Ishibe A contributed to data analysis, interpretation, and writing the report. Masataka Taguri contributed to statistical analysis. Chikara Kunisaki and Itaru Endo contributed to editing, reviewing, and final approval of the report.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Disclosure
Drs. Atsushi Ishibe, Mitsuyoshi Ota, Shoichi Fujii, Yusuke Suwa, Hirokazu Suwa, Masashi Momiyama, Jun Watanabe, Kazuteru Watanabe, Masataka Taguri, Chikara Kunisaki, and Itaru Endo have no conflicts of interest or financial ties to disclose.
Rights and permissions
About this article
Cite this article
Ishibe, A., Ota, M., Fujii, S. et al. Midterm follow-up of a randomized trial of open surgery versus laparoscopic surgery in elderly patients with colorectal cancer. Surg Endosc 31, 3890–3897 (2017). https://doi.org/10.1007/s00464-017-5418-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00464-017-5418-z