Abstract
Background
Laparoscopic surgery is commonly used in elderly patients over 80 years old. The purpose of this study was to compare the perioperative and oncologic outcomes between laparoscopic surgery and open surgery in elderly patients with colorectal cancer.
Methods
We retrospectively analyzed the medical records of patients aged ≥ 80 years who underwent curative resection of colorectal cancer at six Hallym University-affiliated hospitals. The perioperative outcomes and oncologic outcomes were compared between laparoscopic and open surgery
Results
Of 294 elderly patients, 104 (35.3%) underwent open surgery and 190 (64.7%) underwent laparoscopic surgery. The postoperative hospital stay (P = 0.019) and time to soft diet (P = 0.009) were shorter in the laparoscopic group than in the open group. Postoperative complications were less frequent in the laparoscopic group than in the open group (P < 0.001), including wound infection (P = 0.005), ileus (P = 0.005), and pneumonia (P = 0.001). The 3-year overall survival (OS) (P = 0.982) and recurrence-free survival rates (RFS) (P = 0.532) were similar in both groups. In multivariable analyses, positive lymph node status was the only independent factor associated with OS (P = 0.019) and RFS (P = 0.012). Laparoscopic surgery was not associated with OS (P = 0.874) and RFS (P = 0.772).
Conclusion
Laparoscopic surgery offers several perioperative advantages over open surgery and similar long-term oncological outcomes for elderly patients with colorectal cancer. Therefore, we suggest that laparoscopic surgery can be safely performed for the treatment of elderly patients (≥ 80 years old) with colorectal cancer.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
According to the United Nations World Population Ageing 2019 report, the number of persons worldwide aged 65 years or over will increase from 703 million in 2019 to nearly 1.5 billion in 2050 [1]. Because elderly patients may have decreased physiological functions, higher American Society of Anesthesiologists (ASA) scores [2], and multiple comorbidities [2,3,4], they may be at increased risk of postoperative morbidities and mortality [5,6,7,8,9,10]. Moreover, elderly patients are more likely to present with advanced disease or acute conditions requiring emergent surgery at the time of diagnosis [6, 10, 11].
Colorectal cancer is the third most common cancer and the second leading cause of cancer-related deaths worldwide, with nearly 1.8 million new colorectal cancer cases and 881,00 deaths recorded in 2018 [12].
Several large-scale randomized controlled trials have compared laparoscopic surgery and open surgery for colorectal cancer, and demonstrated that laparoscopic surgery has several short-term advantages, including reduced postoperative pain, shorter hospital stay, and earlier return to normal activity, and similar long-term outcomes, including overall survival (OS) and disease-free survival (DFS) [13,14,15,16]. However, because the mean/median age of patients enrolled in randomized trials ranged from 58 to 70 years, the safety and feasibility of laparoscopic surgery is unclear in octogenarians with colorectal cancer. Aspects of laparoscopic surgery, including pneumoperitoneum, long operative time, and the Trendelenburg position, may be associated with postoperative complications in elderly patients that are unlikely to be seen in younger patients [17,18,19].
A systematic review that compared laparoscopic colectomy and open colectomy in elderly patients with colorectal cancer revealed that laparoscopic colectomy was associated with less blood loss, lower morbidity, fewer surgical site infections, and fewer cases of ileus compared with open colectomy. As long-term outcomes, there were no significant differences in OS and DFS. However, the number of randomized controlled trials was limited [20] and few studies have reported advantages of laparoscopic surgery among elderly patients. Prior studies in this setting enrolled small numbers of patients and were generally performed at single institutions [2, 21,22,23,24,25,26,27]. Furthermore, few studies reported long-term oncologic outcomes [21, 23, 24, 28, 29].
Therefore, the purpose of this study was to compare the perioperative and oncologic outcomes between laparoscopic surgery and open surgery in elderly patients with colorectal cancer.
Methods
We retrospectively analyzed the medical records of patients aged ≥ 80 years who underwent curative resection of colorectal cancer at six Hallym University-affiliated hospitals (Han Gang Sacred Heart Hospital, Gang Nam Sacred Heart Hospital, Gang Dong Sacred Heart Hospital, Chun Cheon Sacred Heart Hospital, Hallym Sacred Heart Hospital, and Dong Tan Sacred Heart Hospital) between January 2010 and December 2019.
We excluded patients with a synchronous colorectal cancer, patients with incomplete data, and patients with a history of another primary malignancy. We also excluded patients who underwent palliative surgery, including bypass surgery or stoma construction, patients who only underwent local tumor resection, and patients who underwent emergent surgery due to intestinal obstruction, bleeding, or perforation.
The choice of surgical approach (laparoscopic or open surgery) was at the surgeon’s discretion. Patient characteristics, operative variables, short-term postoperative outcomes, histopathologic variables, and long-term oncologic outcomes were retrieved from the medical records.
Patient characteristics included age, sex, body mass index (BMI), ASA score, comorbidities, serum carcinoembryonic antigen (CEA) level, and tumor location. The perioperative variables included operation time, conversion, and procedure type. The short-term postoperative outcomes included the time to flatus, time to soft diet intake, postoperative hospital stay, complications, and the 30-day mortality rate. The pathological results included the histologic type of cancer, tumor size, proximal resection margin (PRM), distal resection margin (DRM), lymphovascular invasion (LVI), perineural invasion (PNI), number of harvested lymph nodes, presence of positive lymph nodes, and TNM classification.
After discharge, patients were followed up with physical examinations and measurement of serum CEA/CA (cancer antigen) 19–9 concentrations every 3–6 months for the first 2 years, and every 6 months thereafter until 5 years. Chest and abdominopelvic computed tomography (CT) scans were repeated every 6 months until 5 years. Colonoscopy was performed at 1 year and then biennially during the follow-up period.
Postoperative complications were defined as any condition that required an additional procedure or resulted in prolonged hospitalization, including wound infection, intraabdominal abscess, anastomotic leakage, pneumonia, ileus. Complications were classified using the Clavien–Dindo classification [30]. Conversion to an open procedure was defined as an abdominal incision greater in size than that needed for specimen retrieval.
The long-term oncologic outcomes were evaluated in terms of the OS and recurrence-free survival (RFS). OS was defined as the time from surgery to death from any cause or the last follow-up date. RFS was defined as the time from cancer-related surgery to disease recurrence or death from any cause. The primary end point was the OS rate at 3 years after surgery. The secondary endpoints were postoperative complications and the 30-day mortality rate.
Statistical analysis
All statistical analyses were performed using SPSS version 26.0 (SPSS Inc., Chicago, IL, USA). Continuous variables were compared using Student’s t test or the Mann–Whitney U test, as appropriate, and are presented as the mean ± standard deviation or the median and range. Categorical variables were analyzed using the χ2 test or Fisher’s exact test, as appropriate, and are presented as the number and percentage of patients. OS and RFS were assessed using the Kaplan–Meier method and compared with the log-rank test. Factors associated with survival and recurrence were analyzed using a Cox proportional hazards regression model. The factors included sex, ASA (≥ 3), number of comorbidities (≥ 2), tumor location (rectal cancer), lymph node metastasis, histologic type, type of surgery (laparoscopic surgery), PNI, and LVI. P values of < 0.05 were considered statistically significant.
Results
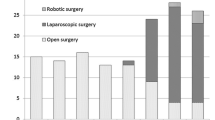
During the 10-year study period, a total of 344 elderly patients underwent surgery for colorectal cancer. We excluded 4 patients with synchronous colorectal cancer, 10 patients with incomplete data, eight patients with a history of another primary malignancy, 14 patients who underwent palliative surgery, 4 patients who only underwent local tumor resection, and ten patients who underwent emergent surgery. After excluding these 50 patients, 294 patients were included in the present study. Of these, 104 (35.3%) underwent open surgery and 190 (64.7%) underwent laparoscopic surgery.
The patients’ characteristics are summarized in Table 1. The mean ages of the open and laparoscopic groups were 84.1 and 83.5 years, respectively (P = 0.141). There were no significant differences between the two groups in terms of the proportions of males/females, ASA score, prior surgical history, and number of comorbidities; however, the proportion of patients with rectal cancer was greater in the laparoscopic group than in the open group (32.1% vs 14.4%, P = 0.001).
Perioperative outcomes according to type of surgery are shown in Table 2. The mean operation time was significantly longer in the laparoscopic group than in the open group (211.9 vs 170.2 min, P < 0.001). The transfusion rate and the types of procedures were similar in both groups. Fecal diversions were more frequently performed in the open group than in the laparoscopic group (P = 0.008). When the patients with colon cancer and rectal cancer were analyzed separately, the operation time was longer in the laparoscopic group than in the open group for colon cancer (195.9 vs 167.0 min, P = 0.002) and for rectal cancer (260 vs 185 min, P = 0.014; Supplemental Table 1). Fecal diversion was performed more frequently among patients with colon cancer in the open group than in the laparoscopic group (29.2% vs 7.0%, P < 0.001) (Supplemental Table 1). There were 21 (11.1%) conversions from laparoscopic surgery to open surgery because of severe adhesion in five patients, invasion to adjacent structures in five patients, inadequate surgical field due to bowel distension in four patients, a huge tumor mass in four patients, intraoperative bleeding in two patients, and empyema in one patient. The time to flatus (3.9 vs 4.9 days, P = 0.006), time to soft diet (6.1 vs 8.6 days, P = 0.009), and length of hospital stay (14.2 vs 17.8 days, P = 0.019) were significantly shorter in the laparoscopic group than in the open group (Table 2). In patients with colon cancer, the times to flatus (3.9 vs 4.9 days, P = 0.033) and soft diet (6.2 vs 8.5 days, P = 0.023) were significantly shorter in the laparoscopic group than in the open group. In patients with rectal cancer, the time to soft diet was significantly shorter in the laparoscopic group than in the open group (6.0 vs 7.0 days, P = 0.043; Supplemental Table 1). The length of hospital stay tended to be longer in the open group than in the laparoscopic group (17.8 vs 14.1 days, P = 0.054) (Supplemental Table 1). In patients with rectal cancer, the times to soft diet (6.0 vs 7.0 days P = 0.043) were significantly shorter in the laparoscopic group than in the open group (Supplemental Table 1). Postoperative complications were less frequent in the laparoscopic group than in the open group (8.4% vs 25.0%, P < 0.001) (Table 2). In particular, wound infection (1.6% vs 8.7%, P = 0.005), ileus (1.6% vs 8.7%, P = 0.005), and pneumonia (0.5% vs 7.7%, P = 0.001) were significantly less frequent in the laparoscopic group than in the open group. According to the Clavien–Dindo classification, the frequency of Grade I–II complications was significantly lower in the laparoscopic group than in the open group (1.6% vs 16.3%, P < 0.001). The 30-day mortality rate was not significantly different between the two groups (1.6% vs 2.9%, P = 0.669). When patients with colon cancer and rectal cancer were analyzed separately, the overall complication rate was lower in the laparoscopic group for both cancer types (colon: P < 0.001; rectum: P = 0.038) (Supplemental Table 1). For patients with colon cancer, wound infection (P = 0.009), ileus (P = 0.002), and pneumonia (P = 0.002) were less frequent in the laparoscopic group than in the open group.
Tumor size, histologic type, PNI, and TNM stage were similar in both groups (Table 3). PRM (20.5 vs 13.1 cm, P = 0.006), DRM (11.8 vs 8.9 cm, P = 0.027), and LVI (59.2% vs 37.9%, P < 0.001) were significantly greater in the open group than in the laparoscopic group. The number of harvested lymph nodes was significantly greater in the open group than in the laparoscopic group (27.3 vs 20.1, P = 0.002). Among patients with rectal cancer, there were no significant differences in PRM, DRM, LVI, or the number of harvested lymph nodes (Supplemental Table 2). Among patients with colon cancer, the PRM (21.7 vs 12.5 cm, P = 0.003), LVI (61.4% vs 41.1%, P = 0.003), and number of harvested lymph nodes were greater in the open group than in the laparoscopic group (Supplemental Table 2).
The mean duration of follow-up was 33.9 months (range, 2–110 months; open group: 34.8 months; laparoscopic group: 33.4 months). During the follow-up period, 47 of the 294 patients died (19.5%). The most common cause of death was progression of colorectal cancer in 12 patients, followed by pneumonia or acute respiratory distress syndrome in 10 patients, myocardial infarction or heart failure in six patients, another malignancy in six patients, septic shock due to bowel perforation in four patients, acute renal failure in two patients, and gastrointestinal bleeding in two patients. The cause of death was unknown in five patients because they had died before arrival at the emergency center. The 3-year OS rates in the open and laparoscopic groups were 68.8% and 70.5%, respectively (P = 0.982; Fig. 1a). The 3-year RFS rates in the open and laparoscopic groups were 57.2% and 59.1%, respectively (P = 0.532; Fig. 2a). When patients with stage II or III colorectal cancer were analyzed separately, survival outcomes were similar between the open and laparoscopic groups in terms of 3-year OS (stage II: P = 0.972; stage III: P = 0.498; Fig. 1b, c) and 3-year RFS (stage II: P = 0.766; stage III: P = 0.450; Fig. 2b, c). During the follow-up period, disease recurrence occurred at a similar rate in the laparoscopic and open groups (15.8% vs 14.4%, P = 0.756). The most common site of recurrence was the lung, followed by the liver, peritoneum, abdominal lymph nodes, bone, and abdominal wall (Table 4).
In the multivariable analyses, positive lymph node status was independently associated with OS (P = 0.019) and RFS (P = 0.012). Laparoscopic surgery was not associated with OS (P = 0.874) or RFS (P = 0.772) (Table 5).
Discussion
Previous studies have reported that the time to flatus, time to soft diet, and the postoperative hospital stay were significantly shorter after laparoscopic surgery than after open surgery [21, 23,24,25, 27]. The results in this study are consistent with those of previous studies. Hinoi et al. analyzed elderly patients with colon cancer and rectal cancer separately, and reported that patients with colon cancer who underwent laparoscopic surgery had shorter time to bowel movements and a shorter hospital stay than patients who underwent open surgery, whereas the hospital stay in patients with rectal cancer was similar between the laparoscopic and open surgery groups (19 days vs 18 days, P = 0.990) [28]. Among patients with rectal cancer in the present study, the postoperative hospital stay was about 3.8 days shorter in the laparoscopic group than in the open group. However, this was not statistically significant (P = 0.149), possibly due to the relatively small number of patients, which prevented us from reaching a definitive conclusion.
Although several studies have reported similar rates of postoperative complications between laparoscopic surgery and open surgery in elderly patients [5, 25, 26, 31], others have reported lower rates of postoperative complications with laparoscopic surgery [20, 21, 23, 24, 32]. In the present study, the overall postoperative complication rate was significantly lower in the laparoscopic group than in the open group (8.4% vs 25.0%, P < 0.001). In particular, the rates of wound infection, ileus, and pneumonia were significantly lower in the laparoscopic surgery group, which could be explained by several advantages of minimal invasive surgery, including the shorter incision length and less postoperative pain [15, 33]. These results in the present study applied to colon cancer, but not rectal cancer. A randomized controlled trial (Comparison of Open versus laparoscopicsurgery for mid and low REctal cancer After Neoadjuvant chemoradiotherapy: COREAN Trial) of patients with mid or low rectal cancer also showed no significant differences in the overall and individual complications between open and laparoscopic surgery [16].
The number of harvested lymph nodes was greater in the open group than in the laparoscopic group (27.3 vs 20.1, P = 0.002) in the present study. When we analyzed patients with colon cancer and rectal cancer separately, the number of harvested lymph nodes was greater with open surgery than with laparoscopic group among patients with colon cancer (29.1 vs 20.7, P = 0.002). A systematic review that assessed the adequacy of lymph node harvesting in patients with colon cancer demonstrated that the number of harvested lymph nodes is associated with survival and recommended that the surgeon should harvest at least 12 lymph nodes for adequate sampling [34]. The mean number of harvested lymph nodes in the laparoscopic group was 20, which exceeds the recommended number of lymph node for adequate sampling. In rectal cancer, the mean number of harvested lymph nodes was not significantly different between the two groups (18.9 vs 16.8, P = 0.437). The COREAN trial also reported that the number of harvested lymph nodes was similar between open and laparoscopic surgery (18 vs 17, P = 0.085) [16]. In the study by Hinoi et al., the number of harvested lymph nodes was similar between open and laparoscopic surgery (11 vs 12.5, P = 0.995) among elderly patients with rectal cancer [28].
Sufficient proximal and distal margins are required when removing the mesocolic lymph nodes to achieve safe oncologic outcomes. Previous studies reported that a longitudinal tumor spread exceeding 10 cm is very rare in patients with colon cancer [35, 36]. Therefore, recent guidelines for colon cancer surgery recommend a longitudinal resection margin of at least 10 cm [37]. In the present study, although the mean DRM in the laparoscopic group was 8.9 cm, the mean DRM in patients with colon cancer was 10.9 cm (Supplemental Table 2), which was compatible with the guidelines for colon cancer.
Several studies have reported the long-term outcomes of laparoscopic surgery for elderly patients [21, 24, 28]. Hinoi et al. reported that the 3-year OS, DFS, and cancer-specific survival rates in elderly patients with rectal or colon cancer did not differ between laparoscopic and open surgery [28]. In another recent study of elderly patients over 80 years old, there were no significant differences in long-term outcomes, namely the 5-year OS (P = 0.224) and DFS (P = 0.230) rates, between laparoscopic and open surgery [21]. In the present study, the 3-year OS and RFS rates were not significantly different between the open and laparoscopic groups (OS: P = 0.982, RFS: P = 0.532). Furthermore, we found no differences in the OS and DFS rates between the two groups in patients with stage II (OS: P = 0.972; RFS: P = 0.766) or stage III (OS: P = 0.498, RFS: P = 0.450) cancer. These results are comparable with those of previous studies [21, 24, 28].
There are several limitations to the present study. First, it was a retrospective study, which may introduce selection bias. It is possible that the surgeons tended to perform laparoscopic surgery in patients with good performance status and early-stage colorectal cancer, whereas open surgery may have been preferred for patients with poor performance status and advanced-stage cancers. However, because of ethical issues associated with enrolling elderly patients in clinical trials, it will be difficult to perform prospective randomized trials to reach a definitive conclusion. Moreover, although the present study was conducted at six hospitals, the number of patients was insufficient to reach a definite conclusion. We did not perform adequate propensity score matching analysis to eliminate possible bias. Third, the median follow-up time in the present study was 33.9 months, which was shorter than that of previous studies, where it ranged from 37.4 to 39.5 months [21, 24, 28]. This may be due to the retrospective design of our study and greater loss to follow-up. Despite these limitations, this study provides valuable clinical information regarding the treatment of elderly patients with colorectal cancer.
Conclusion
Laparoscopic surgery offers several perioperative advantages over open surgery and similar long-term oncological outcomes for elderly patients with colorectal cancer. Therefore, we suggest that laparoscopic surgery can be safely performed for the treatment of elderly patients (≥ 80 years old) with colorectal cancer.
References
United Nations, Department of Economic and Social Affairs (2019) Population division. World Population Prospects, 2019
Tomimaru Y, Ide Y, Murata K (2011) Outcome of laparoscopic surgery for colon cancer in elderly patients. Asian J Endosc Surg 4(1):1–6
Senagore AJ, Madbouly KM, Fazio VW et al (2003) Advantages of laparoscopic colectomy in older patients. Arch Surg 138(3):252–256
Frasson M, Braga M, Vignali A et al (2008) Benefits of laparoscopic colorectal resection are more pronounced in elderly patients. Dis Colon Rectum 51(3):296–300
Vignali A, Di Palo S, Tamburini A et al (2005) Laparoscopic vs. open colectomies in octogenarians: a case-matched control study. Dis Colon Rectum 48(11):2070–2075
Turrentine FE, Wang H, Simpson VB et al (2006) Surgical risk factors, morbidity, and mortality in elderly patients. J Am Coll Surg 203(6):865–877
Biondi A, Vacante M, Ambrosino I et al (2016) Role of surgery for colorectal cancer in the elderly. World J Gastrointest Surg 8(9):606–613
Chang GJ, Skibber JM, Feig BW et al (2007) Are we undertreating rectal cancer in the elderly? An epidemiologic study. Ann Surg 246(2):215–221
Basili G, Lorenzetti L, Biondi G et al (2008) Colorectal cancer in the elderly. Is there a role for safe and curative surgery? ANZ J Surg 78(6):466–470
Colorectal Cancer Collaborative Group (2000) Surgery for colorectal cancer in elderly patients: a systematic review. Lancet 356(9234):968–974
Scott NA, Jeacock J, Kingston RD (1995) Risk factors in patients presenting as an emergency with colorectal cancer. Br J Surg 82(3):321–323
Bray F, Ferlay J, Soerjomataram I et al (2018) Global cancer statistics 2018: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J Clin 68(6):394–424
Nelson H, Sargent DJ, Wieand HS et al (2004) A comparison of laparoscopically assisted and open colectomy for colon cancer. N Engl J Med 350(20):2050–2059
Guillou PJ, Quirke P, Thorpe H et al (2005) Short-term endpoints of conventional versus laparoscopic-assisted surgery in patients with colorectal cancer (MRC CLASICC trial): multicentre, randomised controlled trial. Lancet 365(9472):1718–1726
Veldkamp R, Kuhry E, Hop WC et al (2005) Laparoscopic surgery versus open surgery for colon cancer: short-term outcomes of a randomised trial. Lancet Oncol 6(7):477–484
Jeong SY, Park JW, Nam BH et al (2014) Open versus laparoscopic surgery for mid-rectal or low-rectal cancer after neoadjuvant chemoradiotherapy (COREAN trial): survival outcomes of an open-label, non-inferiority, randomised controlled trial. Lancet Oncol 15(7):767–774
Russo A, Marana E, Viviani D et al (2009) Diastolic function: the influence of pneumoperitoneum and Trendelenburg positioning during laparoscopic hysterectomy. Eur J Anaesthesiol 26(11):923–927
van der Pas MH, Haglind E, Cuesta MA et al (2013) Laparoscopic versus open surgery for rectal cancer (COLOR II): short-term outcomes of a randomised, phase 3 trial. Lancet Oncol 14(3):210–218
Odeberg-Wernerman S (2000) Laparoscopic surgery–effects on circulatory and respiratory physiology: an overview. Eur J Surg Suppl 585:4–11
Fujii S, Ishibe A, Ota M et al (2014) Short-term results of a randomized study between laparoscopic and open surgery in elderly colorectal cancer patients. Surg Endosc 28(2):466–476
Zhou S, Wang X, Zhao C et al (2019) Laparoscopic vs open colorectal cancer surgery in elderly patients: short- and long-term outcomes and predictors for overall and disease-free survival. BMC Surg 19(1):137
Chan TY, Foo CC, Law WL et al (2019) Outcomes of colorectal cancer surgery in the nonagenarians: 20-year result from a tertiary center. BMC Surg 19(1):155
Miguchi M, Yoshimitsu M, Hakoda K et al (2018) Short-term outcomes of laparoscopic surgery in octogenarians with colorectal cancer: a single-institution analysis. Surg Today 48(3):292–299
Moon SY, Kim S, Lee SY et al (2016) Laparoscopic surgery for patients with colorectal cancer produces better short-term outcomes with similar survival outcomes in elderly patients compared to open surgery. Cancer Med 5(6):1047–1054
Nishikawa T, Ishihara S, Hata K et al (2016) Short-term outcomes of open versus laparoscopic surgery in elderly patients with colorectal cancer. Surg Endosc 30(12):5550–5557
Mukai T, Akiyoshi T, Ueno M et al (2014) Outcomes of laparoscopic surgery for colorectal cancer in oldest-old patients. Surg Laparosc Endosc Percutan Tech 24(4):366–369
Lian L, Kalady M, Geisler D et al (2010) Laparoscopic colectomy is safe and leads to a significantly shorter hospital stay for octogenarians. Surg Endosc 24(8):2039–2043
Hinoi T, Kawaguchi Y, Hattori M et al (2015) Laparoscopic versus open surgery for colorectal cancer in elderly patients: a multicenter matched case-control study. Ann Surg Oncol 22(6):2040–2050
Nakamura T, Sato T, Miura HT et al (2014) Feasibility and outcomes of surgical therapy in very elderly patients with colorectal cancer. Surg Laparosc Endosc Percutan Tech 24(1):85–88
Dindo D, Demartines N, Clavien PA (2004) Classification of surgical complications: a new proposal with evaluation in a cohort of 6336 patients and results of a survey. Ann Surg 240(2):205–213
Chern YJ, Tsai WS, Hung HY et al (2018) The dark side of laparoscopic surgery for colorectal cancer patients aged 75 years or older. Int J Colorectal Dis 33(10):1367–1371
Tei M, Ikeda M, Haraguchi N et al (2009) Postoperative complications in elderly patients with colorectal cancer: comparison of open and laparoscopic surgical procedures. Surg Laparosc Endosc Percutan Tech 19(6):488–492
Braga M, Vignal A, Gianotti L et al (2002) Laparoscopic versus open colorectal surgery: a randomized trial on short-term outcome. Ann Surg 236(6):759–766 (discussion 767)
Chang GJ, Rodriguez-Bigas MA, Skibber JM et al (2007) Lymph node evaluation and survival after curative resection of colon cancer: systematic review. J Natl Cancer Inst 99(6):433–441
Morikawa E, Yasutomi M, Shindou K et al (1994) Distribution of metastatic lymph nodes in colorectal cancer by the modified clearing method. Dis Colon Rectum 37(3):219–223
Toyota S, Ohta H, Anazawa S (1995) Rationale for extent of lymph node dissection for right colon cancer. Dis Colon Rectum 38(7):705–711
Søndenaa K, Quirke P, Hohenberger W et al (2014) The rationale behind complete mesocolic excision (CME) and a central vascular ligation for colon cancer in open and laparoscopic surgery: proceedings of a consensus conference. Int J Colorectal Dis 29(4):419–428
Acknowledgements
This research was supported by Hallym University Research Fund, 2020 (HURF-2020-58).
Funding
Hallym University Research Fund, 2020 (HURF-2020-58).
Author information
Authors and Affiliations
Contributions
All authors contributed to the study conception and design. Material preparation, data collection and analysis were performed by ITS, BMK, BCK and MJK. The first draft of the manuscript was written by JYK and JWK. And all authors commented on previous versions of the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Conflict of interest
All authors declare that they have no conflict of interest.
Ethical approval
The study was approved by the Institutional Review Board of Dongtan Sacred Heart Hospital (IRB 2020-08-001-001). The Institutional Review Board waived the need to obtain informed consent in view of the retrospective nature of the study.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
About this article
Cite this article
Son, I.T., Kim, J.Y., Kim, M.J. et al. Clinical and oncologic outcomes of laparoscopic versus open surgery in elderly patients with colorectal cancer: a retrospective multicenter study. Int J Clin Oncol 26, 2237–2245 (2021). https://doi.org/10.1007/s10147-021-02009-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10147-021-02009-4