Abstract
Background
Transanal endoscopic microsurgery (TEM) for the excision of rectal tumor is mostly performed as an inpatient procedure. The aim of this study was to assess the feasibility and safety of TEM resection as an outpatient procedure in selected patients.
Population
All first 178 consecutive patients who underwent resection of a rectal tumor using TEM in our institution from April 2011 to September 2013 were included.
Method
Standardized retrospective chart review was performed. Primary outcome was 30-day mortality and morbidity. Secondary outcomes included unplanned admission and readmission rates, operative and pathologic data.
Results
Of the 175 patients who underwent only TEM, 80 % (140/175) were discharged the same day of surgery. There was no mortality. Morbidity rate was 31.4 %. Ninety-one percent of 154 patients planned as outpatients were discharged the same day. The most common reason for unplanned admission was urinary retention (7/14; 50 %). Twelve patients discharged the day of the procedure were readmitted at 30 days. Median operative time was 60 min (10–256 min). All lesions were removed with grossly negative margins with 15 positive microscopic margins on final pathology. A total of 124 adenomatous polyps and 37 malignant lesions were excised. Mean tumor diameter after fixation was 5.0 cm (range 0.5–11 cm).
Conclusion
Transanal endoscopic microsurgery as an outpatient procedure is feasible and safe in selected patients. The main reason for unplanned admission was urinary retention in our series.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Transanal endoscopic microsurgery (TEM) has first been described in Germany by Dr. Buess in 1980 [1, 2]. An operative proctoscope is used to create a pneumorectum, and endoscopic instruments allow for removal of tumor and suturing. This technique has recently gained new impetus in North America for resection of benign or malignant rectal tumors. This technique would replace the conventional transanal excision (TAE) or, in many cases, a transabdominal radical surgery (low anterior resection) as this approach allows resection of tumor located higher up in the rectum not accessible with standard TAE [3–5]. TEM is known to be a safe alternative to the standard TAE approach and is associated with additional benefits such as improved visualization with optical magnification and rectal distention [6, 7]. A reduction in specimen fragmentation also allows for a better histopathologic analysis. TEM resection also has been associated with a reduction in recurrence for villous tumor [4].
TEM was initially used to remove benign rectal polyp unresectable by standard endoscopic technique which would otherwise often require an anterior resection [2]. Indications have expanded to include selected T1 rectal cancer, small T2–T3 rectal cancer in patients unfit for radical surgery or small neuroendocrine tumor (<2 cm) [5].
Treatment has evolved from a radical transabdominal resection to a minimally invasive procedure using natural orifice with rectal preservation. The next step is to evaluate the potential for day surgery procedure. Few have reported on learning curve and safety of the introduction of this technique as an outpatient procedure. The aim of this study was to assess the feasibility and safety of TEM resection as an outpatient procedure in selected patients.
Population and method
All consecutive patients having had a TEM resection in our center from the beginning of the program in April 2011 to September 2013 were identified by medical record. Standardized chart review was performed by three trained research assistants. Primary outcome was 30-day mortality and morbidity. Secondary outcomes included unplanned admission and readmission rates, operative and pathologic data.
Patient selection
Preoperative investigation included colonoscopy with tumor biopsy, rigid proctoscopy and in selected cases endoanal ultrasound or pelvic MRI. Rigid proctoscopy was performed in addition to colonoscopy to establish distance from anal verge and anatomic position of the tumor to plan for intraoperative patient positioning.
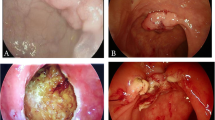
TEM procedure indications
Patient selection included any villous tumor that can be seen entirely on rigid proctoscopy. Large tumor or near circumferential tumor were included. Other indication included scar excision after endoscopic polypectomy containing early cancer and carcinoid tumor. Selected T1 rectal adenocarcinomas with good pronostic factors were also included. Selected patients with T1 or T2 cancer with poor medical condition were offered TEM procedure instead of radical resection. Patients unfit to undergo general anesthesia due to medical condition were not offered TEM resection. Patients in whom preoperative investigation revealed T1 adenocarcinoma with adverse prognostic factors (lymphovascular invasion, perineural invasion, tumoral emboli or poor differentiation) T2 or T3 were offered radical surgery according to the increased risk of regional node involvement [4, 5, 8–11].
Outpatient procedure indications
First ten patients were planned as inpatient procedure to evaluate the safety of the implementation of this new procedure in our center. Thereafter, every patient was considered for day surgery procedure. All patients were assessed for comorbidities that would require postoperative admission for monitoring. Patients with severe pulmonary (sleep apnea or COPD) or cardiac comorbidities (CAD or heart failure) were admitted for postoperative monitoring. Patients requiring medication bridging for anticoagulation were sometimes admitted. All patients planned as outpatient were required to have assistance for the first 48 h after surgery. Also patients from out of town were asked to spend the first 24 h in town. All patients were given numbers to contact their surgeon and instructed to consult to emergency room in case of fever, pain or bleeding after surgery. All patients were seen on follow-up of 4–6 weeks after discharge and were specifically asked whether they required readmission or experienced difficulties after surgery.
Technique
All surgeries were performed in one center by one of the three colorectal surgeons trained for TEM procedure. The two first procedures were performed with the TEO platform (Storz), and the 176 others were performed with the TEM platform (Wolf-Ultramed). The procedure was done under general anesthesia, except for one case realized under spinal anesthesia. All patients received two fleet enemas on the morning of the surgery and preoperative antibiotic. Antithrombotic therapy was also used in selected ones. Foley insertion was performed according to surgeon preference and planned duration of the procedure. Patients were positioned according to tumor location in lithotomy, prone or on left or right lateral side. Transmural excision was planned in the majority of patient to provide a full thickness of specimen for pathological analysis. The deficit closure was performed when possible, with multiple running sutures of 3.0 Maxon.
Patients were directed to recovery room where the Foley catheter, when used, was removed. After extubation and a period of observation, patients were directed to day surgery care unit for a 4- to 6-h observation. Discharge criteria included among others the ability to void spontaneously, adequate pain control, minimal nausea and ability to tolerate liquid intake and the availability of an adult supervision for first 24 h after the surgery. Patients unable to void spontaneously within the first 6 h after the surgery or with supra-pubic discomfort had an ultrasound bladder scan performed to evaluate residual bladder volume. In and out catheterization or Foley insertion was used when deemed appropriate. Patients planned to be admitted for postoperative care and surveillance for significant comorbidities had their Foley removed the following day.
Results
Demographics
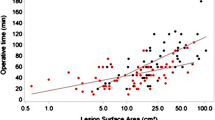
A total of 178 patients treated with TEM resection in our center from April 2011 to September 2013 were identified. Three patients were excluded from this study as they underwent synchronous right hemicolectomy in addition to TEM resection. Mean age was 68 (range 35–96 years) with 58 % of male proportion. ASA classification is shown in Table 1. A majority of patients (82 %) had an ASA score of I or II. Preoperative diagnoses were benign tumors (n = 144), rectal adenocarcinomas (n = 26) or neuroendocrine tumors (n = 5). The majority of tumors (73 %) were located in the mid or proximal rectum (Table 2). Tumor’s anatomic position was evenly distributed in the four quadrants of the rectum. Patient’s intraoperative positioning is presented in Table 2. We used it as a surrogate of tumor location as this was more consistently reported. Mean tumor diameter after fixation was 5 cm (range 0.5–11 cm). Actual rectal defect were not measured.
Operative data
Median operative time was 60 min (10–256 min), and median blood lost was 0 ml (0–500 ml). Intraperitoneal penetration occurred in 15 patients (8.6 %). All were treated with defect closure using TEM but one who required additional transabdominal laparoscopic suture closure of the rectal wall. None of these patients had intraperitoneal complication (Table 3).
Pathologic data
Final pathology revealed 124 adenomatous polyps, 35 adenocarcinomas (T1:28, T2:6 and T3:1) and two carcinoid tumors. Twenty-one specimens with preoperative diagnosis of adenoma revealed foci of transformation to invasive carcinoma on final pathology. In 14 patients, TEM resection was performed on postpolypectomy scar for adenocarcinoma or carcinoid tumor with close margins and none had residual tumor on final pathologic analysis. All lesions were removed with grossly negative margins. Fifteen specimens (8.6 %) were found to have margin focally in contact with the lesion on final pathology (13 adenomas; 2 adenocarcinomas). Both patients with adenocarcinoma with positive margin underwent radical surgery.
Overall mortality and morbidity
There was no mortality, and the 30-day morbidity rate was 31.4 % (Table 4). Of these, 33 were urinary retention (19 %). Seventeen patients were managed with single catheterizations, nine were discharge with a Foley catheter and home care services, and seven were admitted for further management. These 33 patients were all planned as an outpatient procedure. There were no recurrences. Six patients experienced postoperative bleeding (3.4 %) with one requiring colonoscopy for hemostasis. Nine patients had dehiscences (5.1 %) treated conservatively. Four had stenosis (2.3 %) only two requiring dilation. One patient had an abscess requiring drainage, and one patient developed recto-vaginal fistula. Medical complications included two non-ST elevation myocardial infarction (NSTEMI), one postoperative drowsiness and one delirium.
Univariate analysis of POUR risk factors was performed. Patient, tumor and procedure factors were analyzed (Table 5). Patient factors included the following: gender, age, comorbidities, previous pelvic surgery and benign prostatic hypertrophy. Tumor factors included the following: tumor height from anal margin, tumor localization, deficit closure and tumor diameter. Procedure factors included the following: duration of surgery, blood loss, volume of intravenous fluid administration and the utilization of intraoperative Foley catheter. None of these factors were independent predictor of POUR.
Unplanned admission and readmission rate
Of the 178 TEM patients, 154 were planned as outpatient procedure. Of these, 140 (91 %) were discharged the same day. Fourteen patients required unplanned admission for various reasons (Table 6). Seven patients had postoperative urinary retention (POUR) requiring indwelling Foley catheter (mean LOS 2.14 days). Two patients had immediate postoperative bleeding and were admitted for observation (mean LOS 2.50 days), one of them requiring blood transfusion. Two patients were admitted for monitoring after large intraperitoneal penetration during TEM resection with one requiring transabdominal laparoscopic additional suture closure of the rectal wall (LOS 2 days). One patient was admitted for monitoring after a difficult dissection (LOS 2 days), one for postoperative hematuria (LOS 1 day) and one for postoperative drowsiness (LOS 2 days). Twelve patients discharged the day of the procedure were readmitted within 30 days of the procedure. Six patients were readmitted for bleeding between postoperative days 3 and 7, with one requiring a blood transfusion. Two patients were readmitted for dehiscence, another one with an abscess and one for a recto-vaginal fistula. Two patients needed a cardiology consultation (dyspnea and sick sinus syndrome).
Discussion
We report a series of 178 consecutive patients treated with TEM. The vast majority (154 patients) of these transanal resections were planned as outpatient procedure. A total of 140 patients were successfully discharged the same day as planned. Others have reported a postoperative length of stay (LOS) of 0.54–8.7 days [1, 2, 7, 12–14]. Kumar et al. [3] reported a LOS of 0.54 days with 65.4 % of patients done as same day surgery. Ford et al. reported 48 % of cases done as same day surgery, 25 % done as 23-h stay and 26 % as inpatient procedure. Factors influencing their LOS were older age, duration of surgery, tumor diameter and number of quadrants covered by the tumor [15]. We did not use any of these criteria to select patient for day surgery procedure. Only patient unfit to undergo general anesthesia were excluded from TEM resection. Patients requiring short hospital stay for monitoring of medical condition were the only ones not considered for day surgery procedure. In our series, only major comorbidities and postoperative complications were admission criteria after the first ten cases. We performed TEM safely as an outpatient procedure even for octogenarians and nonagenarians (n = 22). Long travel distance was not an influencing factor for Ford et al., and they concluded that it was safe to treat them as outpatient basis [15]. We report the same experience.
Complications
Our series report a higher rate of morbidity (31.4 %) than usually reported in the literature 4–29 % [6, 16]. Postoperative urinary retention (POUR) was the most frequent complication in our series (19 %), which is higher than previously reported between 5 and 10 % [3, 12, 17]. We used a more inclusive definition to include all POUR that have clinical impact in our practice. Our POUR definition included the combination of the incapacity to void spontaneously after 6 h requiring the use of in and out catheterization or a Foley insertion. If we had only included the patient who needed a Foley insertion, our incidence would be around 9 %, which compares to others series [3, 13].
Several factors have been reported to be associated with increased POUR after anorectal surgery and particularly after TEM [3, 12, 18, 19]. In our cohort, we evaluated most of these traditional factors and others without identifying significant ones. General anesthesia and large operative proctoscope may in part explain the incidence of POUR. The high incidence of POUR leads us to modify the management of this complication with time. Most patients were initially admitted to the hospital, while currently these are treated in an outpatient setting. No patient experienced long-term urinary retention requiring catheterization after TEM resection in our cohort. Protocols for management of POUR should be available for surgeons and units performing TEM as a day surgery procedure.
All others complications had similar rate than previously reported in the literature [3, 13, 14, 17].
Unplanned admission
Our 30-day readmission rate remains low, with twelve patients (8.6 %) readmitted after discharge. Majority of our readmissions were postoperative bleeding (3.4 %), which compares to other large series (1.2–3.7 %) [1, 3, 12–14]. No invasive treatment was needed. Despite this low rate of readmission, the type of potential complications justifies close surveillance by an accompanying adult and a protocol for easy and quick access to care for these patients.
Bias
Our series as any retrospective study is associated with potential bias. Data regarding the reason for planned admission were not always available or clearly reported. Several patients were also referred from remote centers and some complications may not have been captured. However, all patients were seen on follow-up of 4–6 weeks after discharge and were specifically asked whether they required readmission or experienced difficulties after surgery. On the other hand, all procedures were performed by the same three surgeons in one center, which limit the variability in postoperative care. Also all patients from the beginning of the TEM program were included and not only selected ones.
Conclusion
Transanal endoscopic microsurgery (TEM) is a feasible and safe procedure while performed as an outpatient procedure in most patients. Potential for unplanned admission remains low. Postoperative urinary retention is a frequent complication after TEM; however, most patients can be treated safely with an outpatient protocol.
References
Darwood RJ, Wheeler JM, Borley NR (2008) Transanal endoscopic microsurgery is a safe and reliable technique even for complex rectal lesions. Br J Surg 95:915–918
Buess G, Kipfmuller K, Ibald R et al (1988) Clinical results of transanal endoscopic microsurgery. Surg Endosc 2:245–250
Kumar AS, Coralic J, Kelleher DC et al (2013) Complications of transanal endoscopic microsurgery are rare and minor: a single institution’s analysis and comparison to existing data. Dis Colon Rectum 56:295–300
Cataldo PA (2006) Transanal endoscopic microsurgery. Surg Clin N Am 86:915–925
Christoforidis D, Cho HM, Dixon MR et al (2009) Transanal endoscopic microsurgery versus conventional transanal excision for patients with early rectal cancer. Ann Surg 249:776–782
Langer C, Liersch T, Suss M et al (2003) Surgical cure for early rectal carcinoma and large adenoma: transanal endoscopic microsurgery (using ultrasound or electrosurgery) compared to conventional local and radical resection. Int J Colorectal Dis 18:222–229
Demartines N, von Flue MO, Harder FH (2001) Transanal endoscopic microsurgical excision of rectal tumors: indications and results. World J Surg 25:870–875
Chang AJ, Nahas CS, Araujo SE et al (2008) Early rectal cancer: local excision or radical surgery? J Surg Educ 65:67–72
Hompes R, Cunningham C (2011) Extending the role of transanal endoscopic microsurgery (TEM) in rectal cancer. Colorectal Dis 13(Suppl 7):32–36
Doornebosch PG, Zeestraten E, de Graaf EJ et al (2012) Transanal endoscopic microsurgery for T1 rectal cancer: size matters! Surg Endosc 26:551–557
Dias AR, Nahas CS, Marques CF et al (2009) Transanal endoscopic microsurgery: indications, results and controversies. Tech Coloproctol 13:105–111
Bignell MB, Ramwell A, Evans JR et al (2010) Complications of transanal endoscopic microsurgery (TEMS): a prospective audit. Colorectal Dis 12:e99–e103
Tsai BM, Finne CO, Nordenstam JF et al (2010) Transanal endoscopic microsurgery resection of rectal tumors: outcomes and recommendations. Dis Colon Rectum 53:16–23
Allaix ME, Rebecchi F, Giaccone C et al (2011) Long-term functional results and quality of life after transanal endoscopic microsurgery. Br J Surg 98:1635–1643
Ford SJ, Wheeler JM, Borley NR (2010) Factors influencing selection for a day-case or 23-h stay procedure in transanal endoscopic microsurgery. Br J Surg 97:410–414
Heintz A, Morschel M, Junginger T (1998) Comparison of results after transanal endoscopic microsurgery and radical resection for T1 carcinoma of the rectum. Surg Endosc 12:1145–1148
Bach SP, Hill J, Monson JR et al (2009) A predictive model for local recurrence after transanal endoscopic microsurgery for rectal cancer. Br J Surg 96:280–290
Baldini G, Bagry H, Aprikian A et al (2009) Postoperative urinary retention: anesthetic and perioperative considerations. Anesthesiology 110:1139–1157
Kin C, Rhoads KF, Jalali M et al (2013) Predictors of postoperative urinary retention after colorectal surgery. Dis Colon Rectum 56:738–746
Acknowledgments
Thanks to our collaborators Vicky Pelletier and Claudya Morin, clinical clerks.
Disclosures
Drs. Anne-Sophie Laliberte, Aude Lebrun, Sebastien Drolet, Philippe Bouchard and Alexandre Bouchard have no conflicts of interest or financial ties to disclose.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Laliberte, AS., Lebrun, A., Drolet, S. et al. Transanal endoscopic microsurgery as an outpatient procedure is feasible and safe. Surg Endosc 29, 3454–3459 (2015). https://doi.org/10.1007/s00464-015-4158-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00464-015-4158-1