Abstract
Background
Roux-en-Y gastric bypass (RYGBP) is a validated technique for the treatment of morbid obesity and results in a significant rate of remission of type 2 diabetes (T2D). Omega gastric bypass (OGBP) is an effective and simpler alternative for weight loss, but its effect on T2D is unclear.
Methods
Between December 2006 and September 2012, 804 laparoscopic OGBPs were carried out in our centre. Among these, 100 (12.4 %) patients had T2D at the time of the intervention. Remission of T2D was defined by a glycated haemoglobin (HbA1c) level of <6 % without concomitant treatment.
Results
Postoperative follow-up was completed by 81 patients (mean age: 49 ± 11 years; mean weight at surgery: 133 ± 29 kg; mean body mass index (BMI): 47 ± 9 kg/m2). Mean preoperative HbA1c was 8 ± 2 g/dL. Before OGBP, seven patients (9 %) had received no oral hypoglycaemic treatment, 30 (37 %) had received monotherapy, 26 (32 %) bitherapy, six (7 %) tritherapy and 12 (15 %) patients had used insulin. Over a mean follow-up of 26 months (range 1–75), mean weight decreased to 94 ± 23 kg and mean BMI to 35 kg/m2. Seventy-one (88 %) patients had complete remission of T2D and the other 10 (12 %) had reduced their treatment. Seven patients (58 %) initially treated with insulin no longer required this treatment. Mean time to remission of T2D for patients receiving one or more oral therapies versus insulin was 6.9 versus 17.9 months.
Conclusions
OMBP is effective treatment for obesity in terms of weight loss and remission of T2D.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
The effect of bariatric surgery on type 2 diabetes (T2D) is unclear. However, an increasing number of publications report an improvement or even remission of T2D in obese patients who have undergone bariatric surgery [1–3].
Among the different procedures used, gastric by-pass [4] and bilio-pancreatic diversions (BPD) [5] appear to bring about the best long-term results when compared to restrictive techniques. Omega loop gastric bypass (OGBP), originally described by Rutledge [6], is a recent mixed technique (restrictive + reduced absorption), which appears to give similar results in terms of weight loss to those obtained with Roux-en-Y gastric bypass (RYGBP) [7]. OGBP is simpler and quicker to perform than RYGBP and is associated with fewer complications. However, the effects of this technique on T2D remain to be completely known [8].
We analysed the outcome of OGBP on remission of T2D in obese patients undergoing bariatric surgery in our hospital. The criteria studied included change in body weight, body mass index (BMI) and glycated haemoglobin (HbA1C), as well as any modifications to hypoglycaemic treatment short- and long-term. Finally, the results were analysed for between group differences in order to identify predictive factors for T2D improvement.
Patients and methods
Study design and patients
This retrospective, monocentre study was carried out in the Department of Digestive Surgery, Georges Pompidou Hospital, Paris, France, between 2006 and 2012. The aim was to evaluate the effects of OGBP on T2D. The inclusion criteria were a preoperative diagnosis of T2D with or without hypoglycaemic treatment and a history of first-line or second-line OGBP after simple restrictive surgery (gastric banding).
Obese patients who presented with criteria for bariatric surgery were evaluated preoperatively according to the recommendations of the Haute Autorité de Santé. A complete blood examination was carried out routinely (thyroid hormones, fatty acids, glycaemia, vitamins and proteins). When an anomaly in fasting blood glucose (FBG) or HbA1c level was discovered (FBG > 1.2 g/dL or HbA1c > 6.5 %), the patients were referred to the diabetology department for a complete 5-day assessment. During this assessment, the duration of diabetes and possible secondary complications were investigated and optimal hypoglycaemic treatment was initiated.
The patients were followed by the diabetology team until a satisfactory HbA1c level was obtained. The patients were finally discussed in a multidisciplinary meeting to validate the indication for surgical treatment.
Data analysed
The following data were analysed in order to investigate the independent factors for remission of T2D: (i) treatment-related: number of patients requiring one, two or three oral hypoglycaemic treatments and patients requiring an injectable treatment (±oral treatment); (ii) BMI: <40, 40–50 or >50 kg/m2; (iii) duration of diabetes: >3 or <3 years; and (iv) preoperative diabetic control: initial HbA1c ≤6.5 %.
Surgical procedure
OGBP was carried out by laparoscopy in all patients. The surgical procedure consisted of the creation of a long gastric sleeve (sleeve gastrectomy) using a calibration probe from 34 to 36 Fr and a mechanical linear anastomosis with the small intestine, 2 m from the angle of Treitz. Despite being proposed by some authors, the length of the excluded loop was not varied according to BMI.
Water tightness of the anastomosis was determined per-operatively using methylene blue. A gastric catheter was systematically left in situ on the anastomosis until day 1. The gastric catheter was removed after measuring the level of C-reactive protein (limit: ≤300), clinical evaluation and measurement of heart rate (limit: 120 bpm). In the case of an anomaly, a high resolution scan was carried out before gastric catheter removal. An aspiration drain was inserted systematically during surgery below the anastomosis, along the line of stapling of the gastric sleeve.
Feeding was recommenced on day 2 with the introduction of drinks and was progressively enriched in texture and quantity. All patients received vitamin, zinc, iron and protein supplements from the start. Protective gastric treatment with a protein pump inhibitor was associated with supplementation.
An initial postoperative consultation was carried out by the surgeon 1 month after OGBP. A second consultation was carried out at 3 months and was combined with a consultation with a dietician. During this consultation, blood count, vitamin and ion deficiency, lipid and blood glucose examinations were performed (FBG and HbA1c). Combined follow-up was carried out every 3 months during the first year, every 6 months during the second year, and at least once per year during successive years.
Diabetes remission was defined by a reduction in HbA1c below 6 %, without the need for hypoglycaemic treatment, and FBG < 7 mmol/L. Diabetes improvement was defined as a postoperative reduction of treatment (drug number or dosage), HbA1c < 6.5 % and discontinuation of injectable hypoglycaemic drugs in patients who needed them before surgery. Remission rate and mean time to remission or improvement of diabetes were determined in all patients and in the subgroups described above (see “Data analysed”).
Results
Characteristics of the patients
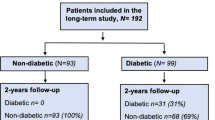
A total of 804 obese patients underwent OGBP surgery between 2006 and 2012. One-hundred (12.4 %) patients with T2D were selected and 81 of these completed the follow-up (mean follow-up time: 26.4 months (range 1–75)). Mean age of the patients at OGBP was 48.5 ± 10.8 years, mean weight was 132.9 ± 28.6 kg and mean BMI was 47.1 ± 8.5 kg/m2. Mean HbAlc level was 7.7 ± 1.9 %.
Among the 81 patients, seven (8 %) had stable HbAlc levels around 6.5 % and received no hypoglycaemic treatment, 30 (37 %) received one oral treatment, 26 (32 %) two, six (7 %) three and 12 (14 %) required insulin. Three-quarters (82.5 %) of the patients had controlled diabetes and 27.5 % had uncontrolled diabetes (HbA1c > 6.5 % despite treatment).
Clinical and biochemical characteristics post-OGBP surgery
Weight loss
For the 804 OGBPs performed, excess weight loss (EWL) at 3 years was 76 % and mean BMI reached was 30.3 kg/m2. EWL was significantly greater in the diabetic group than in the non-diabetic group (61.9 ± 32.2 vs. 54.4 ± 34.1 %, respectively; p = 0.049). At 3 years, mean weight in the diabetic patients was 93.9 ± 22.5 kg and mean BMI was 34.7 kg/m2 (Fig. 1).
Remission/improvement of diabetes
At 2 years, 71/81 patients (87.6 %) had complete remission and 10 (12.3 %) had an improvement in their diabetes (Fig. 2). Injectable hypoglycaemic treatment was stopped in 58.3 % of patients. In the seven patients not receiving hypoglycaemic treatment at the time of OGBP, the remission rate was 100 %. The mean time to remission was 1.3 months (range 0–9 months).
In patients receiving a single treatment (n = 30), the remission rate was 93.3 % (28/30) with a mean time to remission of 7 months. The other two patients in this group had an improvement in their diabetes at 26 and 28 months, respectively. Patients treated with bitherapy had a remission rate of 96 % (25/26) and a mean time to remission of 7.5 months. The other patient in this group had an improvement in their diabetes at 58 months. In the patients receiving three oral hypoglycaemic drugs (n = 6), the remission rate was 66.6 % and the mean time to remission was 4.3 months. Two patients in this group (33.3 %) had an improvement in their diabetes at 9 and 12 months, respectively.
The results were less marked in patients treated with injectable hypoglycaemic drugs. In these 12 patients, the remission rate was 50 % and the mean time to remission was 18 months. Nevertheless, the rate of improvement overall was 100 % (mean time to improvement of 5.7 months). Remission of diabetes was significantly higher in patients who were not receiving injectable hypoglycaemic treatment before surgery than in those who were (p < 0.001) (Fig. 3).
The 81 patients were divided into three groups according to their initial BMI: (i) Group 1: BMI < 40; (ii) Group 2: BMI 40–50; (iii) Group 3: BMI > 50. Group 1 (n = 15) had a diabetes remission rate of 80 % and an improvement rate of 20 %. Mean follow-up was 26.5 months (range 3–65) and mean weight was 78.5 kg (range 54–91). Group 2 (n = 37) had a remission rate of 86.6 % and an improvement rate of 13.5 %. Mean follow-up was 21 months (range 1–60) and mean weight was 89.8 kg (57–134.5). In Group 3 (n = 24), the rate of remission was 91.7 % and the improvement rate was 8.3 % (Fig. 4). Mean follow-up was 33.5 months (range 3–75) and mean weight was 109 kg (range 60–167). It was not possible to demonstrate a significant difference in remission rate as a function of BMI however due to the small group size.
Preoperative HbA1c levels were only available for 62/81 patients. The other 19 patients were therefore excluded from this analysis. Forty-five patients had poorly controlled diabetes despite treatment. The mean BMI of this group was 46.7 kg/m2 (no treatment (n = 4), monotherapy (n = 13), biotherapy (n = 14), tritherapy (n = 6) and injectable drugs (n = 8)). Mean follow-up of this group was 26.6 months. The rate of remission was 84.4 % and the improvement rate was 15.6 %. Seventeen patients had well controlled diabetes preoperatively. Mean BMI of this group was 50.2 kg/m2 (no treatment (n = 1), monotherapy (n = 9), biotherapy (n = 5), tritherapy (n = 0) and injectable drugs (n = 2)). Mean follow-up of this group was 32.4 months. The remission rate was 88.2 % and the improvement rate was 11.8 %. It was not possible to demonstrate a significant difference in remission rate between these two groups due to the small group size.
Finally, the results were analysed as a function of the duration of diabetes. Only 39/81 patients had a diagnosis with a specified date and were included in this analysis. Duration of 3 years was chosen as a limit to obtain two homogenous groups: 16 patients with diabetes for <3 years and 23 patients with diabetes for >3 years. Mean follow-up was 25 months. Patients with recent diabetes had a mean weight of 149 kg and a mean BMI of 52, whereas patients with diabetes for >3 years had a mean weight of 127 kg and a mean BMI of 46. Patients with diabetes for <3 years had a higher remission rate over follow-up than those with diabetes for >3 years. The values tended to show a plateau in each group (Fig. 5), with a remission rate of 93.7 % in patients with a recent diagnosis (and an improvement rate of 6.3 %) versus 68 % for patients with a diagnosis of >3 years (and an improvement rate of 32 %). Once again, it was not possible to demonstrate a significant difference in remission rate between these two groups due to the small group size.
Rate of complications post-OGBP
The rate of complications after OGBP surgery was 15:7.5 % early complications and 7.5 % late complications. There was no significant difference in complication rate between diabetic and non-diabetic patients. Only 5 % of complications that occurred in diabetic patients required a new surgical intervention (vs. 3.2 % in the non-diabetic group); 2.5 % were early and 2.5 % late (Table 1).
Discussion
RYGBP is a validated intervention and the treatment of choice for T2D in obese patients and its indications have progressively extended to non-obese patients with T2D [9–13]. However, this procedure is complicated to perform and is associated with a high rate of complications when performed by untrained surgeons. OGBP, which has been developed more recently, could therefore be a serious alternative. Studies comparing these two procedures have emphasised the speed and reduced rate of morbidity of OGBP when compared to RYGBP, with similar results in terms of weight loss and diabetes remission [14–19]. These results have been confirmed in small groups of non-obese subjects with T2D [20, 21].
Preoperative BMI, weight loss, age, sex, hypoglycaemic drug use and diabetes duration also have an influence on the rate of remission and re-emergence of diabetes [1, 2, 4, 10, 22–30]. The outcome of OGBP in terms of weight loss is excellent, with a weight loss at 3 years that is comparable or even superior to that reported for RYGBP. In parallel, the rate of complete remission of T2D at 2 years is remarkable and lies between that obtained with RYGBP and BPD [9, 31–34]. If the weight loss is maintained over time, it could constitute a factor for long-term remission which is better than that obtained with RYGBP [4, 9, 23, 24, 29]. In our patients, preoperative BMI was not a predictive factor for remission of diabetes, even though the results were better in patients with a higher BMI. The role of preoperative BMI in the response to bariatric surgery remains controversial and few authors have demonstrated a link with remission rate [1, 9].
It is clear that the risk of developing T2D increases with an increase in BMI, but the severity of T2D in patients with a low BMI seems to implicate a deficiency in insulin secretion rather than a phenomenon of insulin resistance [22, 25, 27, 35]. The duration of diabetes would confirm this hypothesis, with a better ≪reserve≫ for insulin secretion in obese patients recently affected by T2D [3, 10, 21–27, 30]. Our results are similar to those published previously, with a higher rate of response in patients with recent diabetes. The absence of a significant difference was probably related to the small group sizes.
Insulin requirement is widely recognised as a predictive factor for poor response and for re-emergence of T2D [4, 10, 19, 22, 25]. Our experience confirms this finding. In general, better results were obtained for patients with easier glycaemic control (diet and monotherapy). This difference, once again, lacked statistical power due to the small group sizes.
Preoperative HbA1c appears to be predictive for remission of T2D in many studies [4, 10, 22] since poorly controlled diabetes will be less sensitive to the improvement in insulin response post-surgery, given the probable pre-existing deficit in secretion by B-cells in the pancreas [36–42]. Our data are similar to those published previously, without significant superiority of the group with well-controlled diabetes pre-surgery.
Our results favour the use of OGBP for the treatment of T2D in obese patients. The rates of remission and improvement are similar to those reported with BPD, and the associated weight loss is at least equivalent to that reported with RYGBP.
Our complication rate with OGBP is low. We have never diagnosed severe hypoglycaemia or dumping syndrome in our patients. Furthermore, we have only performed five Y conversions, carried out four times for destabilising reflux in patients with a mean postoperative BMI of 25 kg/m2 and once for an anastomotic ulcer resistant to medical treatment.
These initial results suggest that OGBP could be considered as a first-line alternative to RYGBP in obese diabetic patients, due to the excellent results in terms of remission and weight loss, associated with reduced morbidity and a simple operative procedure. Studies with larger group sizes are necessary to validate these results.
References
Sjostrom CD, Lissner L, Wedel H, Sjostrom L (1999) Reduction in incidence of diabetes, hypertension, and lipid disturbances after intentional weight loss induced by bariatric surgery: the SOS Intervention Study. Obes Res 7(5):477–484
Buchwald H, Estok R, Fahrbach K, Banel D, Jensen MD, Pories WJ, Bantle JP, Sledge I (2009) Weight and type 2 diabetes after bariatric surgery: systematic review and meta-analysis. Am J Med 122(3):248–256
Pories WJ, Mac Donald KG, Morgan EJ Jr, Sinha MK, Dohm GL, Swanson MS et al (1992) Surgical treatment of obesity and its effect on diabetes: 10-year follow-up. Am J Clin Nutr 55(2 Suppl):582S–585S
Schauer PR, Burguera B, Ikramuddin S, Cottam D, Gourash W, Hamad G, Eid GM, Mattar S, Ramanathan R, Barinas-Mitchel E, Rao RH, Kuller L, Kelley D (2003) Effect of laparoscopic Roux-en Y gastric bypass on type 2 diabetes mellitus. Ann Surg 238(4):467–484
Iaconelli A, Panunzi S, De Gaetano A, Manco M, Guidone C, Leccesi L, Gniuli D, Nanni G, Castagneto M, Ghirlanda G, Mingrone G (2011) Effects of bilio-pancreatic diversion on diabetic complications: a 10-year follow-up. Diabetes Care 34(3):561–567
Rutledge R (2001) The mini-gastric bypass: experience with the first 1,274 cases. Obes Surg 11(3):276–280
Lee WJ, Yu PJ, Wang W, Chen TC, Wei PL, Huang MT (2005) Laparoscopic Roux-en-Y versus mini-gastric bypass for the treatment of morbid obesity: a prospective randomized controlled clinical trial. Ann Surg 242(1):20–28
Kim Z, Hur KY (2011) Laparoscopic mini-gastric bypass for type 2 diabetes: the preliminary report. World J Surg 35(3):631–636
Buchwald H, Avidor Y, Braunwald E, Jensen MD, Pories W, Fahrbach K, Schoelles K (2004) Bariatric surgery: a systematic review and meta-analysis. JAMA 292(14):1724–1737
Arterburn DE, Bogart A, Sherwood NE, Sidney S, Coleman KJ, Haneuse S, O’Connor PJ, Theis MK, Campos GM, McCulloch D, Selby J (2013) A multisite study of long-term remission and relapse of type 2 diabetes mellitus following gastric bypass. Obes Surg 23(1):93–102
Abbatini F, Rizzello M, Casella G, Alessandri G, Capoccia D, Leonetti F, Basso N (2010) Long-term effects of laparoscopic sleeve gastrectomy, gastric bypass, and adjustable gastric banding on type 2 diabetes. Surg Endosc 24(5):1005–1010
American Diabetes Association, Bantle JP, Wylie-Rosett J, Albright AL, Apovian CM, Clark NG, Franz MJ, Hoogwerf BJ, Lichtenstein AH, Mayer-Davis E, Mooradian AD, Wheeler ML (2008) Nutrition recommendations and interventions for diabetes: a position statement of the American Diabetes Association. Diabetes Care 31(Suppl 1):S61–78
American Diabetes Association (2011) Executive summary: standards of medical care in diabetes—2011. Diabetes Care 34(Suppl 1):S4–S10
Carbajo M, García-Caballero M, Toledano M, Osorio D, García-Lanza C, Carmona JA (2005) One-anastomosis gastric bypass by laparoscopy: results in the first 209 patients. Obes Surg 15(3):398–404
Chakhtoura G, Zinzindohoué F, Ghanem Y, Ruseykin I, Dutranoy JC, Chevallier JM (2008) Primary results of laparoscopic mini-gastric bypass in a French obesity-surgery specialized university hospital. Obes Surg 18(9):1130–1133
Kula KS, Machanda N (2010) Comparison of laparoscopic mini gastric bypass with Roux-en-Y gastric bypass for the treatment of morbid obesity. Surg Obes Relat Dis 6(3):S63–S64
Lee WJ, Lee YC, Ser KH, Su YH, Chen SC (2010) Revisional surgery of laparoscopic mini-gastric bypass: a nine-year follow-up. Surg Obes Relat Dis 6(3):S15
Rutledge R, Walsh TR (2005) Continued excellent results with the mini-gastric bypass: six-year study in 2,410 patients. Obes Surg 15(9):1304–1308
Wang W, Wei PL, Lee YC, Huang MT, Chiu CC, Lee WJ (2005) Short-term results of laparoscopic mini-gastric bypass. Obes Surg 15(5):648–654
Fobi M1, Lee H, Igwe D, Felahy B, James E, Stanczyk M, Fobi N (2002) Gastric bypass in patients with BMI < 40 but >32 without life-threatening co-morbidities: preliminary report. Obes Surg 12(1):52–56
Huang CK, Shabbir A, Lo CH, Tai CM, Chen YS, Houng JY (2011) Roux-en-Y gastric bypass for the treatment of type II diabetes mellitus in Chinese patients with body mass index of 25–35. Obes Surg 21(9):1344–1349
Hayes MT, Hunt LA, Foo J, Tychinskaya Y, Stubbs RS (2011) A model for predicting the resolution of type 2 diabetes in severely obese subjects following Roux-en Y gastric bypass surgery. Obes Surg 21(7):910–916
Campos GM, Rabl C, Mulligan K, Posselt A, Rogers SJ, Westphalen AC, Lin F, Vittinghoff E (2008) Factors associated with weight loss after gastric bypass. Arch Surg 143(9):877–883
Carbonell AM, Wolfe LG, Meador JG, Sugerman HJ, Kellum JM, Maher JW (2008) Does diabetes affect weight loss after gastric bypass? Surg Obes Relat Dis 4(3):441–444
Chikunguwo SM, Wolfe LG, Dodson P, Meador JG, Baugh N, Clore JN, Kellum JM, Maher JW (2010) Analysis of factors associated with durable remission of diabetes after Roux-en-Y gastric bypass. Surg Obes Relat Dis 6(3):254–259
Cummings DE (2009) Endocrine mechanisms mediating remission of diabetes after gastric bypass surgery. Int J Obes (Lond) 33(Suppl 1):S33–S40
DiGiorgi M, Rosen DJ, Choi JJ, Milone L, Schrope B, Olivero-Rivera L, Restuccia N, Yuen S, Fisk M, Inabnet WB, Bessler M (2010) Re-emergence of diabetes after gastric bypass in patients with mid- to long-term follow-up. Surg Obes Relat Dis 6(3):249–253
Hall TC, Pellen MG, Sedman PC, Jain PK (2010) Preoperative factors predicting remission of type 2 diabetes mellitus after Roux-en-Y gastric bypass surgery for obesity. Obes Surg 20(9):1245–1250
Melton GB, Steele KE, Schweitzer MA, Lidor AO, Magnuson TH (2008) Suboptimal weight loss after gastric bypass surgery: correlation of demographics, comorbidities, and insurance status with outcomes. J Gastrointest Surg 12(2):250–255
Vetter ML, Cardillo S, Rickels MR, Iqbal N (2009) Narrative review: effect of bariatric surgery on type 2 diabetes mellitus. Ann Intern Med 150(2):94–103
Sarson DL, Scopinaro N, Bloom SR (1981) Gut hormone changes after jejunoileal (JIB) or biliopancreatic (BPB) bypass surgery for morbid obesity. Int J Obes 5(5):471–480
Sugerman HJ, Wolfe LG, Sica DA, Clore JN (2003) Diabetes and hypertension in severe obesity and effects of gastric bypass-induced weight loss. Ann Surg 237(6):751–756
Lee WJ, Chong K, Ser KH, Lee YC, Chen SC, Chen JC, Tsai MH, Chuang LM (2011) Gastric bypass vs sleeve gastrectomy for type 2 diabetes mellitus. A randomized controlled trial. Arch Surg 146(2):143–148
Zervos E, Agle SC, Warren AJ, Lang CG, Fitzgerald TL, Dar M, Rotondo MF, Pories WJ (2010) Amelioration of insulin requirement in patients undergoing duodenal bypass for reasons other than obesity implicates foregut factors in the pathophysiology of type II diabetes. J Am Coll Surg 210(5):564–572, 572–574
Nannipieri M, Mari A, Anselmino M, Baldi S, Barsotti E, Guarino D, Camastra S, Bellini R, Berta RD, Ferrannini E (2011) The role of beta-cell function and insulin sensitivity in the remission of type 2 diabetes after gastric bypass surgery. J Clin Endocrinol Metab 96(9):E1372–E1379
Cummings S, Apovian CM, Khaodhiar L (2008) Obesity surgery: evidence for diabetes prevention/management. J Am Diet Assoc 108(4 Suppl 1):S40–S44
Koner J, Inabnet W, Febres G, Conwell IM, McMahon DJ, Salas R, Taveras C, Schrope B, Bessler M (2009) Prospective study of gut hormone and metabolic changes after adjustable gastric banding and Roux-en-Y gastric bypass. Int J Obes (Lond) 33(7):786–795
Laferrère B, Heshka S, Wang K, Khan Y, McGinty J, Teixeira J, Hart AB, Olivan B (2007) Incretin levels and effect are markedly enhanced 1 month after Roux-en-Y gastric bypass surgery in obese patients with type 2 diabetes. Diabetes Care 30(7):1709–1716
Mingrone G, Castagneto-Gissey L (2009) Mechanisms of early improvement/resolution of type 2 diabetes after bariatric surgery. Diabetes Metab 35(6 Pt 2):518–523
Morínigo R, Moizé V, Musri M, Lacy AM, Navarro S, Marín JL, Delgado S, Casamitjana R, Vidal J (2006) GLP-1, PYY, hunger and satiety following gastric bypass surgery in morbidly obese subjects. J Clin Endocrinol Metab 91(5):1735–1740
Pournaras DJ, Osbrone A, Hawkins S, Vincent RP, Mahon D, Ewings P, Ghatei MA, Bloom SR, Welbourn R, le Roux CW (2010) Remission of type 2 diabetes after gastric bypass and banding: mechanism and 2 year outcomes. Ann Surg 252(6):966–971
Lee WJ, Chong K, Chen CY, Chen SC, Lee YC, Ser KH, Chuang LM (2011) Diabetes remission and insulin secretion after gastric bypass in patients with body mass index <35 kg/m2. Obes Surg 21(7):889–895
Disclosures
Drs. Guenzi, Arman, Rau, Cordun, Moszkowicz, Voron and Chevallier have no conflicts of interest or financial ties to disclose.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Guenzi, M., Arman, G., Rau, C. et al. Remission of type 2 diabetes after omega loop gastric bypass for morbid obesity. Surg Endosc 29, 2669–2674 (2015). https://doi.org/10.1007/s00464-014-3987-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00464-014-3987-7