Abstract
Background
Two-dimensional (2D) view is known to cause practical difficulties for surgeons in conventional laparoscopy. Our goal was to evaluate whether the new-generation, Three-Dimensional Laparoscopic Vision System (3D LVS) provides greater benefit in terms of execution time and error number during the performance of surgical tasks.
Methods
This study tests the hypothesis that the use of the new generation 3D LVS can significantly improve technical ability on complex laparoscopic tasks in an experimental model. Twenty-four participants (8 experienced, 8 minimally experienced, and 8 inexperienced) were evaluated for 10 different tasks in terms of total execution time and error number. The 4-point lickert scale was used for subjective assessment of the two imaging modalities.
Results
All tasks were completed by all participants. Statistically significant difference was determined between 3D and 2D systems in the tasks of bead transfer and drop, suturing, and pick-and-place in the inexperienced group; in the task of passing through two circles with the needle in the minimally experienced group; and in the tasks of bead transfer and drop, suturing and passing through two circles with the needle in the experienced group. Three-dimensional imaging was preferred over 2D in 6 of the 10 subjective criteria questions on 4-point lickert scale.
Conclusions
The majority of the tasks were completed in a shorter time using 3D LVS compared to 2D LVS. The subjective Likert-scale ratings from each group also demonstrated a clear preference for 3D LVS. New 3D LVS has the potential to improve the learning curve, and reduce the operating time and error rate during the performances of laparoscopic surgeons. Our results suggest that the new-generation 3D HD LVS will be helpful for surgeons in laparoscopy (Clinical Trial ID: NCT01799577, Protocol ID: BEHGynobs-4).
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Laparoscopic surgery has become the standard of practice for many gynecological procedures. One of the greatest challenges in laparoscopic surgical training is adaptation to the two-dimensional (2D) flat view of the surgical field [1]; thus it is well recognized that 2D view causes difficulty for the surgeon. In this context, surgeons have to relearn their operative skills and accustom their brain to acquire spatial orientation [2]. On the other hand, the three-Dimensional Laparoscopic Vision System (3D LVS) has entered the practice also in the da Vinci Robotic System. In both the da Vinci Robotic System and 3D LVS, one of the most important points is how 3D imaging affects the surgical operation to be performed. Byrne et al. have reported that independently of the biomechanical advantages of the da Vinci Robot System, 3D LVS improved performance times by 34–46 % and reduced error rates by 44–66 % for both inexperienced residents and advanced laparoscopic surgeons [3]. Ohuchida et al. have stated that 3D system might contribute to a reduction in the number of surgical accidents [4]. If 3D LVS proves to reduce the surgical execution time and number of mistakes, considering its cost-effectivity in relation to the da Vinci Robotic System, the former might achieve a good place in surgical practice.
The greatest contribution of 3D imaging to surgical practice is the depth perception. Depth perception allows us to carry out our actions with lesser mistakes while both moving and performing tasks. A simple test might exemplify the importance of 3D imaging: shut one eye with one hand and experience the difficulty of walking or performing a task. Several companies have offered the 3D LVS to the use of surgeons to overcome this handicap of 2D imaging systems. The system uses 2 cameras, that are set up in parallel configuration with two separate optical channels. Using the shutter glasses, 3D LVS system projects images obtained from each camera to the monitor at a rate that cannot be detected by man eye. The electronic processor embedded in the glasses relays images to the right and left eye, respectively, to allow perception of two separate images. However, in 3D LVS where polarized glasses are used, images are simultaneously relayed to the monitor at various angles. Each one of the polarized glasses conducts the image to each eye separately.
Since Becker et al. have reported that a 3D LVS might improve laparoscopic procedures; many researchers have investigated the effects of 3D LVS on laparoscopic performance [5, 6]. Information regarding the usefulness of previous generation 3D systems are contradictory; some trials have reported that the tasks can be performed significantly faster with fewer errors and greater performance scores using 3D LVS, whereas others have found no significant difference in the accuracy or speed of the performance of tasks [1, 7–11]. Furthermore, previous 3D systems have been stated to cause visual fatigue in surgeons [12]. Nowadays, last generation high-definition (HD) 3D LVS has entered the practice; however, research is limited on this novel modality. Three-dimensional LVS has been suggested to facilitate the surgical performance for inexperienced surgeons and not to pose any additional challenges for experienced surgeons [7, 13]. In this study, we test the hypothesis that the use of new-generation 3D HD LVS offers greater benefit in terms of execution time and number of mistakes during the performance of complex laparoscopic tasks by surgeons of three different experience levels. This is the first randomized prospective experimental study carried out in different experience groups with Viking 3D HD LVS newly released to the market.
Material and methods
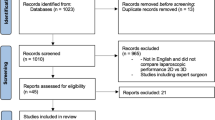
This is a prospective randomized comparative study. Participants were evaluated for 10 different surgical tasks in terms of total execution time and error number by both objective (10 tasks on a 3D laparoscopic instrument fitted to the trainer box) and subjective criteria (4 point lickert scale). Institutional ethics committee approval was obtained, and all participants were informed of the study and provided written informed consent prior to the performance of any study procedures. The study protocol was registered at clinicaltrials.gov before starting the study (Clinical Trial ID: NCT01799577, Protocol ID: BEHGynobs-4).
Participants
A total of 24 volunteering surgeons were evaluated in this experimental study. Surgeons without normal vision, depth perception and/or surgeons with motor dysfunction were excluded from the study. Participants were allocated into three groups based on their level of experience; i.e., inexperienced, minimally experienced (<50 operations = beginners) and experienced (>50 operations). Eight surgeons were included in each group. An experienced participant was defined as a surgeon who has performed a minimum of 50 complete endoscopic procedures involving complex maneuvers such as suturing [14].
Set up
The Viking 3D HD LVS, endoscopic tissue graspers (Autosuture, Covidien, Colorado, USA), scissor (Ethicon, NJ, USA) and needle driver (Karl Storz, Germany) were used in the trainer box platform (Genmed, Istanbul, Turkey) (Fig. 1). 3–0 Vicryl (Ethicon, OH, USA) was used for all suturing tasks. 0° endoscope (Viking Systems, Inc., Westborough, MA, USA) was used for 2D and 3D views. Images were projected to a high definition monitor positioned across the table in direct view of the participant during the performance of laparoscopic tasks. In 2D imaging, the same system was set to 2D and used without glasses to mimic real-life practice. Optimal brightness, contrast, and focus were ensured for both systems, and same laparoscopic instruments were used. Camera was controlled by the same observer (AO) in all performances. Participants were allowed to familiarize themselves with the instrument under 2D and 3D views. To avoid a learning curve bias, a computer-based randomization was used to determine whether the participants began the study with 2D or 3D LVS (Fig. 1).
3D high definition laparoscopic vision system (3D HD LVS)
The Viking 3D HD Laparoscopic Vision System (Viking Systems, Inc., Westborough, MA, USA) consisting of a binocular optic channel scope, a stereoscopic camera and 3D processing unit was used (Fig. 2A). In 3D HD visualization, the monitor shows two separate images for the left and right eyes; which are displayed to the corresponding eye by special filter glasses using micropolarization technology [15]. Participants were asked to wear passive, lightweight, polarized glasses to perceive 3D images displayed on a 3D, high definition video-monitor (Fig. 2B).
Tasks
Ten complex tasks were used for objective assessment [3, 4, 16] (Fig. 2). All tasks were completed on the same day. A detailed description of each task is provided below.
Touching a sequence of circles with a needle
Participants were asked to touch circles at different heights labeled as 1, 2, and 3 with the needle at the tip of the needle driver (Fig. 2C).
Cutting task
Participants were asked to cut a marked line without running over (Fig. 2D).
Passing through two circles with the needle
Participants were asked to pass two metal circles (a narrow and a broad circle) with the needle (Fig. 2E).
Bead transfer and drop
Ten beads were placed at the bottom of a plastic cylinder. The container cup was cut so as to accept only one bead at a time. The participants were asked to transfer 10 beads from the cylinder to the container (Fig. 2F).
Suturing task (a, b, c)
a—Participants were asked to pass the Penrose drain with suture from right to left with right hand, b—Participants were asked to pass the Penrose drain with suture from right top to left bottom with right hand, c—Participants were asked to pass the Penrose drain with suture from left to right with left hand (Fig. 2G).
Pick and place
Participants were asked to place 10 rings onto 10 pins (Fig. 2H)
Needle transfer
Participants were asked to transfer the needle from one instrument to another instrument.
Catch the suture material with needle driver
Participants were asked to catch the loosely situated suture material with the grasper.
Evaluation
Objective evaluation
The time required for task completion as well as any “errors” occurring during the performances were recorded.
Subjective evaluation
Upon the completion of tasks, subjects were asked to evaluate the subjective complexity level of each task on a scale from 1 (very simple) to 10 (very complex). Also, participants were asked to compare the two imaging systems on 4-Point Lickert scale (excellent, good, poor, very poor) with regard to the imaging quality, satisfaction, preference, spatial orientation, exhaustion, physical discomfort, visual strain, facial discomfort, headache, and difficulty [17].
Statistical analysis
The Statistical Package for Social Sciences (SPSS) software version 11.1 (SPSS, Chicago, IL, USA) was used to perform statistical analyses. Data were presented as arithmetic means, and standard deviation was calculated for each group. Overall study data were assessed with definitive statistical methods (mean, standard deviation) and Kolmogorov–Smirnov distribution test was used in data with normal distribution. Non-parametric statistical analyses were used since normal distribution was not achieved in many parameters and the number of observations was below 30. Quantitative data and experience groups were compared using the Kruskal–Wallis test, and Mann–Whitney U test was performed to test the significance of pairwise differences using Bonferroni correction to adjust for multiple comparisons (p < 0.05/3 for 3 combinations assessed). The significant post correction alpha value was calculated as 0.167. Wilcoxon sign test was used in 2D–3D intra-group comparisons. Results were evaluated with a 95 % confidence interval, a significance level of p < 0.05, and Bonferroni correction to p < 0.0167 and p < 0.01 p < 0.001 and advanced significance level.
Results
Participants consisted of 12 males and 12 females and mean age was 33.2 ± 8.1 (range 24–56) years. All tasks were completed by all participants.
In the group with no experience, the average number of mistakes was statistically significantly lower in 3D as compared to 2D LVS in the tasks of bead transfer (Z = −2.121; p = 0.034 < 0.05) and suturing from left top to right bottom of Penrose drain with the left hand (Z = −2.000; p = 0.046 < 0.05) (Table 1).
In the group with minimal experience, the time taken to touch a sequence of circles with the needle was statistically significantly lower in 3D as compared to 2D LVS (Z = −2.028; p = 0.043 < 0.05) (Table 1), and the complexity level was statistically significantly lower in 3D as compared to 2D LVS (Z = −2.207; p = 0.027 < 0.05) (Table 2).
In the experienced group, the time taken for bead transfer, and pick and place tasks was statistically significantly shorter in 3D compared to 2D LVS (Z = −2.100; p = 0.036 < 0.05 and Z = −2.100; p = 0.036 < 0.05, respectively) (Table 1). Also, suturing from the right top to left bottom of Penrose drain with right hand lasted statistically significantly shorter in 3D compared to 2D LVS (Z = −2.380; p = 0.017 < 0.05) (Table 2).
Wilcoxon test was performed to identify the difference between 2D and 3D LVS in terms of the time spent by 24 participants to transfer the beads from one container to the other, and demonstrated a statistically significant difference (p = 0.032 < 0.05) (Table 2). Although it took shorter time (18.542 ± 21.387 s and 25.167 ± 21.546 s, respectively) and less mistakes (0.208 ± 1.021, 0.583 ± 1.530, respectively) to transfer the needle from one instrument to the other in 3D as compared to 2D LVS, the difference was not statistically significant (p = 0.176, p = 0.343, respectively). However, on subjective questioning participants found it easier to perform the needle transfer task with 3D LVS (p = 0.047 < 0.05) (Table 2). Although there was a statistically significant difference between 3D and 2D LVS in terms of time spent by 24 participants to pass the needle through the circles (p = 0.013 < 0.05), there was not a significant difference between the two systems in terms of the number of mistakes in the same task (p = 0.136) (Table 2). Again, on subjective questioning, participants identified 3D LVS as the system that made the performance easier. (p = 0.044 < 0.05) (Table 2). The task of suturing from the left top to the right bottom of Penrose drain with left hand was performed faster (142.000 ± 101.608, 171.958 ± 115.551 s, respectively), and the number of mistakes was lower in 3D compared to 2D LVS (0.292 ± 0.859, 0.417 ± 0.504, respectively); however, the differences did not reach statistical significance (p = 0.184, p = 0.285, respectively). On subjective questioning, participants identified 3D LVS as the system that made it easier to perform the latter task (p = 0.039 < 0.05) (Table 2).
Regardless of experience, ten questions about 2D and 3D imaging systems were asked to each participant based on the 4-Point Lickert scale (Table 3). 3D LVS was found to be statistically significantly better in six of ten questions (image quality, satisfaction, preference, spatial orientation, exhaustion, physical discomfort), and no statistically significant difference was determined between the two systems in the remaining four questions (complexity, headache, eye fatigue, facial discomfort) (Table 3). Overall in study participants, total rates of excellent and good were 95.8 % in 3D LVS and 70 % in 2D LVS (p < 0.05) in terms of preference (Table 3). In the experienced group, there was not a significant difference in terms of the 10 questions of the 4-Point Lickert scale (p > 0.05).
Discussion
Laparoscopy with 2D imaging has been limited by lack of depth perception and spatial orientation [3]. Monocular cues are used in 2D laparoscopy to compensate for this lack of depth perception, and through experience, processing of monocular cues can be learned and depth perception might be improved [3, 18, 19]. Laparoscopic surgeons require extensive experience to overcome these handicaps of 2D display [4]. Additionally, the risk of injury increases due to potential misperception of the originally 3D structure of human anatomy in the 2D system [20, 21]. Although a laparoscopic 3D display has been reported to be useful over two decades ago, 3D systems have not been used widely [4, 13]. The role of newly designed HD, stereoscopic 3D visualization system in overcoming the drawbacks of 2D system is worth investigating [22]. Silvestri et al. have reported that the main problem with these studies was that they compared low-resolution 3D displays with high definition 2D [16]. Previous studies comparing 2D and 3D LVS have been limited by the technology available, and several studies have failed to demonstrate statistically significant improvement in performance or accuracy with 3D compared to 2D imaging [2, 18, 23–26]. Some studies cite a steep learning curve with 2D imaging obviating any improvement that may have been observed with 3D vision [2, 3, 18, 27, 28]. Others criticize the quality of the 3D technology [2, 18, 27]. However, most of these studies have been conducted before 2000s [2, 18, 27]. Today, studies have reported that 3D HD imaging system provides a good imaging experience thanks to the current technological developments [15, 22]. Novel 3D systems provide superior depth perception and resolution relative to the more rudimentary systems previously evaluated [22].
Experienced endoscopists are able to gather spatial clues (e.g., shadows or triangle parallax) subconsciously from a 2D view, and interpret them into precision and speed [7, 29]. Hence, the perceived ease and objective performance success with 3D systems should hypothetically be more significant for beginners [7]. Patel et al. have stated that inexperienced surgeons would find this system more useful [7]. On the other hand, Byrn et al. have suggested that both experienced and inexperienced surgeons could benefit from 3D LVS [3]. However, studies have reported no difference between the performances of these two groups of surgeons, [2, 25, 30, 31]. In our study, we did not find any difference in terms of the performance of tasks between the two imaging systems in different experience groups. Our study was based on the evaluation of completion time of ten surgical tasks that have been previously reported, from simple to complex, and the number of mistakes made during the performances was used as an objective criteria [3, 4]. We found that all participants completed the tasks of transferring beads and passing two circles with the needle in a shorter time with 3D LVS. Also, when participants were asked to evaluate the systems by the ease of use, they pointed out 3D LVS as providing more ease in performing the tasks including passing two circles with the needle and suturing from left top to right bottom with left hand. When participants were allocated into 3 experience groups, it was observed that the number of mistakes was significantly lower with 3D LVS in the tasks of bead transferring and suturing from left top to right bottom with left hand in the inexperienced group. Also, passing two circles with a needle took shorter and was easier with 3D LVS for the minimally experienced participants. Furthermore, participants in the experienced group performed the tasks of bead transferring, picking and placing, and suturing from right top to left bottom with right hand faster with 3D LVS. Contrary to the statements of Thomson et al., we found that with 3D LVS some of tasks were performed in a statistically significantly shorter time with a lower number of mistakes and with more preference on subjective evaluation [14].
Upon the completion of all the tasks with both systems, 10 questions of subjective evaluation criteria were asked to all subjects as per 4-point Lickert scale, and participants reported a preference for 3D LVS in 6 out of 10 questions (image quality, satisfaction, preference, spatial orientation exhaustion and physical discomfort). In the remaining 4 questions (visual strain, facial discomfort, headache, difficulty) participants reported no difference between the two systems. Pietrabissa et al. and Mueller et al. have stated that they observed fatigue, headache, visual strain in surgeons using the 3D system [25, 30]. However, these disadvantages have not been described in most reports, including our study [18]. These reported complaints might be due to the use of an old system; i.e., the heavy and cumbersome 3D Head Mounted Device (HMD). Also, the use of active optic shuttering feature in old type 3D systems contrary to the use of passive polarized glasses in the last generation 3D HD system might have contributed to these handicaps. Active optic shuttering feature has been reported to cause eye strain in surgeons [22]. Ramanathan et al. have reported two significant problems about HMD; i.e., weight of the system and the difficulty of mounting and demounting the instruments from the ports due to restriction of field of vision [31]. The novel 3D HD system is advantageous in the sense that it utilizes the polarization technology, implying very light glasses that do not obstruct the field of vision.
Most previous studies including that of Kong et al. have been performed using the old type non-HD 3D system [32]. One of the most important technical details in these studies is that they have compared non-HD 2D and non-HD 3D systems [32]. Today, the HD feature is included in both 2D and 3D display systems. However, significant technical advances have been made in the design of 3D HD LVS [22], which might explain the lack of visual strain, headache, physical discomfort and other complaints in our study.
Similar to our study, Tanagho et al. have also compared the Viking 3D HD and the 2D system [22], though with a different percentage distribution of experience levels (69.7 % no-experience, 9.1 % min. experience, and 6.1 % experienced) [22]. In our study, we included equal number of participants in each experience group and thus aimed to prevent any bias due the different number of subjects in group comparisons.
Bilgen et al. have compared the 3D LVS with 2D system in cholecystectomy [33] in a few number of patients, and concluded that the operation was performed in a significantly shorter time with 3D LVS. Storz et al. have also reported that operations can be performed faster and with less harm thanks to 3D HD; and suggested that patient safety can be enhanced in more complex operations with 3D HD LVS [15]. Shortening in operation durations has an utmost importance particularly in long operations, since it may reduce surgical complications due to tiredness. Also, shorter operations will ensure efficient use of the operating room. The number of mistakes was one of the most significant objective criteria in our study; because fewer mistakes in tasks performed with 3D LVS might mean less complication during operations.
Although the currently used 3D system is more expensive than the standard 2D system, this higher cost seems to be verified when the former’s potential to replace the much more expensive robotic imaging in endoscopic surgery is considered. Current robotic surgery system is used extensively despite its high costs both in terms of the device itself and its yearly maintenance. Considering the fact that one of the most important features of robotic surgery is its 3D imaging; we believe the comparatively inexpensive 3D LVS system might find itself a significant place in endoscopic surgery.
Most previous studies about 2D and 3D LVS, including the recent ones, have used separate systems for 2D and 3D; i.e., the telescope, camera, light source and monitor used in each system was different [6, 34]. However, we used the same system in both modalities, i.e., the same telescope, camera and monitor, and conducted the study only by changing the 2D–3D setting. Therefore, contrary to the previous literature studies, we avoided any mistakes due to system difference.
Our study had certain limitations including the experimental design itself. When the number of mistakes and subjective criteria were evaluated in all the tasks 3D LVS was not superior to 2D LVS. We believe that although we studied at least as many participants as in comparable previous studies, examination of a bigger participant population and more tasks would have resulted in support of 3D LVS. The weightiness and bulkiness of the 3D camera used in our study should also be deemed as yet another limitation causing extra fatigue in surgeons. On the other hand, our study was designed to mimic the actual clinical practice as closely as possible. Hence, participants in the 2D group did not wear glasses, contrary to the participants in the 3D group. Although it might have been possible to obtain a better statistical comparison with glasses on for both 2D and 3D groups, we preferred to perform our study without altering the standard practice procedures of the two imaging systems to grasp an understanding of real life conditions.
Consequently the majority of the tasks were completed in shorter time with the novel 3D HD LVS, and subjective criteria indicated 3D as being better than 2D system. Additionally, 3D visualization produced less visual strain, facial discomfort, headache, difficulty, or other side effects than the 2D visualization. Our results also demonstrated that both experienced and inexperienced surgeons may benefit from 3D HD LVS. Majority of the participants preferred 3D over 2D visualization. Improved 3D imaging systems have the potential to shorten the learning curve, and reduce the operating time and error rate during the performances of laparoscopic surgeons. Thus, it might be asserted that myomectomy, sacrocolpopexy, intraabdominal adhesion, or pelvic lymphadenectomy operations can be performed faster, and with less mistakes and complications with the help of deep perception in 3D HD systems. While endo-wristed technology and 3D imaging stand out as significant advantages in the Robotic system, their cost and heavy structure remain as disadvantages [12]. 3D laparoscopy systems can be used in almost every gynecologic operation since they are cheaper and more mobile than Robotic system, allow more than one person to follow the case, and have no maintenance cost incurred. We believe, 3D HD LVS will soon be more commonly used with glass-free 3D monitors. Yet, it would not be a surprise to see that 2D is replaced by 3D HD imaging system in laparoscopic surgery in near future.
References
Bhayani SB, Andriole GL (2005) Three-dimensional (3D) vision: does it improve laparoscopic skills? An assessment of a 3D head-mounted visualization system. Rev Urol 7:211–214
Chan AC, Chung SC, Yim AP et al (1997) Comparison of two-dimensional versus three-dimensional camera systems in laparoscopic surgery. Surg Endosc 11:438–440
Byrn JC, Schluender S, Divino CM et al (2007) Three-dimensional imaging improves surgical performance for both novice and experienced operators using the da Vinci Robot System. Am J Surg 193:519–522
Ohuchida K, Kenmotsu H, Yamamoto A, Sawada K, Hayami T, Morooka K, Hoshino H, Uemura M, Konishi K, Yoshida D, Maeda T, Ieiri S, Tanoue K, Tanaka M, Hashizume M (2009) The effect of CyberDome, a novel three-dimensional dome-shaped display system, on laparoscopic procedures. Int J Comput Assist Radiol Surg 4(2):125–132
Becker H, Melzer A, Schurr MO, Buess G (1993) 3D video techniques in endoscopic surgery. Endosc Surg Allied Technol 1(40–46):2
Cicione A, Autorino R, Breda A, De Sio M, Damiano R, Fusco F, Greco F, Carvalho-Dias E, Mota P, Nogueira C, Pinho P, Mirone V, Correia-Pinto J, Rassweiler J, Lima E (2013) Three-dimensional versus standard laparoscopy: comparative assessment using a validated program for laparoscopic urologic skills. Urology 82(6):1444–1450
Patel HRH, Ribal MJ, Arya M, Nauth-Misir R, Joseph JV (2007) Is it worth revisiting laparoscopic three-dimensional visualization? a validated assessment original research article. Urology 70(1):47–49
Birkett DH, Josephs LG, Este-McDonald J (1994) A new 3D laparoscope in gastrointestinal surgery. Surg Endosc 8:1448–1451
van Bergen P, Kunert W, Schurr MO et al (1996) Comparative study of endoscopic 2D and 3D imaging systems. Langenbecks Arch Chir Suppl Kongressbd 113:634–637
Taffinder N, Smith SG, Huber J et al (1999) The effect of a second generation 3D endoscope on the laparoscopic precision of novices and experienced surgeons. Surg Endosc 13:1087–1092
Sun CC, Chiu AW, Chen KK et al (2000) Assessment of a three-dimensional operating system with skill tests in a pelvic trainer. Urol Int 64:154–158
Buchs NC, Volonte F, Pugin F, Toso C, Morel P (2013) Three-dimensional laparoscopy: a step toward advanced surgical navigation. Surg Endosc 27:692–693
Durrani AF, Preminger GM (1994) Advanced endoscopic imaging: 3D laparoscopic endoscopy. Surg Technol Int 3:141–147
Thomsen MN, Lang RD (2004) An experimental comparison of three-dimensional and two-dimensional endoscopic systems in a model. Arthroscopy 20:419–423
Storz P, Buess GF, Kunert W, Kirschniak A (2012) 3D HD versus 2D HD: surgical task efficiency in standardized phantom tasks. Surg Endosc 26:1454–1460
Silvestri M, Simi M, Cavallotti C, Vatteroni M, Ferrari V, Freschi C, Valdastri P, Menciassi A, Dario P (2011) Autostereoscopic three-dimensional viewer evaluation through comparison with conventional interfaces in laparoscopic surgery. Surg Innov 18(3):223–230
Blavier A, Gaudissart Q, Cadiere GB, Nyssen AS (2007) Comparison of learning curves and skill transfer between classical and robotic laparoscopy according to the viewing conditions: implications for training. Am J Surg 194:115–121
Hanna GB, Shimi SM, Cuschieri A (1998) Randomised study on influence of two-dimensional versus three-dimensional imaging on performance of laparoscopic cholecystectomy. Lancet 351:248–251
Coren S, Ward LM (1989) Sensation and perception. Harcourt Brace Jovanovich College Publishers, Orlando, pp 17–19
Khoshabeh R, Juang J, Talamini MA, Nguyen TQ (2012) Multiview glasses-free 3D laparoscopy. IEEE Trans Biomed Eng 59(10):2859–2865
Gofrit ON, Mikhail AA, Zorn KC, Zagaja GP, Steinberg GD, Shalhav AL (2008) Surgeons’ perceptions and injuries during and after urologic laparoscopic surgery. Urology 71:404–407
Tanagho YS, Andriole GL, Paradis AG, Madison KM, Sandhu GS, Varela JE, Benway BM (2012) 2D versus 3D visualization: impact on laparoscopic proficiency using the fundamentals of laparoscopic surgery skill set. J Laparoendosc Adv Surg Tech A 22(9):865–870
Crosthwaite G, Chung T, Dunkley P, Shimi S, Cuschieri A (1995) Comparison of direct vision and electronic two- and three-dimensional display systems on surgical task efficiency in endoscopic surgery. Br J Surg 82:849–851
Rabin J (1995) Two eyes are better than one: binocular enhancement in the contrast domain. Ophthalmic Physiol Opt 15:45–48
Pietrabissa A, Scarcello E, Mosca F (1994) Three-dimensional versus two-dimensional video system for the trained endoscopic surgeon and the beginner. End Surg 2:315–317
Cagenello R, Arditi A (1993) Binocular enhancement of visual acuity. J Opt Soc Am A 10:1841–1848
Jones DB, Brewer JD, Soper NJ (1996) The influence of three-dimensional video systems on laparoscopic surgery. Surg Laparosc Endosc 6:191–197
Yohannes P, Rotariu P, Pinto P et al (2002) Comparison of robotic versus laparoscopic skills: is there a difference in the learning curve? Urology 60:39–45
Danis J (1996) Theoretical basis for camera control in teleoperating. Surg Endosc 10:804–808
Mueller MD, Camartin C, Dreher E et al (1999) Three-dimensional laparoscopy: gadget or progress? A randomized trial on the efficacy of three-dimensional laparoscopy. Surg Endosc 13:469–472
Ramanathan R, Salamanca JIM, Mandhani A, Leung RA, Rao SR, Berryhill R, Tewari A (2009) Does three-dimensional (3D) visualization improve the quality of assistance during robotic radical prostatectomy? World J Urol 27:95–99
Kong SH, Oh BM, Yoon H, Ahn HS, Lee HJ, Chung SG, Shiraishi N, Kitano S, Yang HK (2010) Comparison of two- and three-dimensional camera systems in laparoscopic performance: a novel 3D system with one camera. Surg Endosc 24(5):1132–1143
Bilgen K, Ustun M, Karakahya M, Isik S, Sengul S, Cetinkunar S, Kucukpinar TH (2013) Comparison of 3D imaging and 2D imaging for performance time of laparoscopic cholecystectomy. Surg Laparosc Endosc Percutan Tech 23(2):180–183
Wagner OJ, Hagen M, Kurmann A, Horgan S, Candinas D, Vorburger SA (2012) Three-dimensional vision enhances task performance independently of the surgical method. Surg Endosc 26(10):2961–2968
Acknowledgments
We would like to thank all participants involved in the study including Riza Kutanis, Atilla Celik, Gülcin Ercan, Baris Sana, Hüseyin Bilge, Sinan Binboga, Rumeysa Ilkar, and Elif Gür of the Department of General Surgery; Serdar Aykan of the Department of Urology; Ulviye Hanli, Hikmet Kocer, Alper Tosun, Hüseyin Dayan, Banu Güler, Eylem Odacilar, Selim Oztürk, Gülümser Ece Aksakal, Elif Cansu Gündogdu, and Merve Ozkan of the Department of Obstetrics and Gynecology, and OR nurses and staff including Sevil Topuz, Gulluhan Erbas, and Yavuz Karayilan.
Disclosures
Drs. Usta, Ozkaynak, Kovalak, Ergul, Naki and Kaya have no conflicts of interest or financial ties to disclose.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Usta, T.A., Ozkaynak, A., Kovalak, E. et al. An assessment of the new generation three-dimensional high definition laparoscopic vision system on surgical skills: a randomized prospective study. Surg Endosc 29, 2305–2313 (2015). https://doi.org/10.1007/s00464-014-3949-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00464-014-3949-0