Abstract
Background
Three variants of Achalasia have been described using high-resolution esophageal manometry (HRM). While manometrically distinct, their clinical significance has yet to be established. Our objective was to compare the outcome after myotomy in patients with these Achalasia subtypes.
Methods
A retrospective chart review was performed to identify patients with Achalasia who had HRM and who underwent Heller myotomy or Per oral endoscopic myotomy (POEM). Symptoms and esophageal clearance by timed barium study were compared before and after treatment.
Results
We identified 49 patients, 21 males and 28 females, with a median age of 52 years. The primary symptom in all patients was dysphagia, with a median duration of 4 years (range 4 months–50 years). By HRM, ten patients (20 %) were classified as Type I, 30 (61 %) as Type II, and 9 (18 %) as Type III. At a median follow-up of 16 months after myotomy (range 1–63 months), the median Eckardt score was zero and was similar across subtypes. Relief of dysphagia was also similar across subtypes (80 % of Type I, 93 % of Type II and 89 % of Type III).
On pre-treatment timed barium study, no patient had complete emptying at 1 or 5 min. After myotomy, complete emptying occurred within 1 min in 50 % (20/40) and within 5 min in 60 % (24/40) and was similar across groups.
Conclusion
Myotomy for Achalasia results in excellent symptomatic outcome and improvement in esophageal clearance. There was no difference among the described HRM Achalasia variants. This calls into question the clinical utility of Achalasia sub-classification and affirms the benefit of myotomy for this disease.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The diagnosis of Achalasia is typically confirmed with esophageal manometry based on the presence of incomplete lower esophageal sphincter (LES) relaxation and absent esophageal body peristalsis. Esophageal pressurization and a hypertensive LES may also be present. The introduction of high-resolution esophageal manometry (HRM) into clinical practice has provided more detail about esophageal function, and HRM studies in patients with Achalasia have identified three subtypes of this disease. Termed the Chicago classification, these subtypes are Type I or “classic” Achalasia with incomplete LES opening and an aperistaltic esophageal body, Type II with panesophageal pressurization, and Type III with no normal peristalsis but evidence of esophageal spasm [1]. While manometrically distinct, the clinical significance and treatment implications of this sub-classification system have not been clearly established. The aim of this study was to determine whether the HRM subtype impacts outcome in patients treated with myotomy for Achalasia.
Methods
In 2008, our lab transitioned from stationary motility to HRM. We conducted a retrospective chart review from 2009 to 2013 to identify all patients with Achalasia who had HRM and who subsequently underwent primary Heller myotomy or Per oral endoscopic myotomy (POEM). Patients with prior endoscopic treatment for Achalasia were included, but those who had previous foregut surgery were excluded. Information on patient BMI, age, previous intervention (Botox or dilatation), duration of symptoms, and medication history were collected. Symptoms were assessed using the Eckardt score (Table 1) [2]. In addition, esophageal clearance was evaluated with a timed barium study using a standardized protocol where the patient rapidly drank 150 ml of liquid barium, and esophageal retention was assessed at 1 and 5 min [3]. This study was approved by the IRB of the University of Southern California.
High-resolution manometry
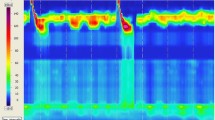
Our technique for HRM has been previously described [4]. Tracings were analyzed using the Manoview 3.0 software (Given Imaging Inc., Duluth GA). Achalasia subtypes were defined using the updated Chicago classification system [5]. In this system, all three subtypes have an elevated integrated relaxation pressure (IRP) and absence of normal peristalsis. Type I is the classic form of Achalasia, while Type II has the addition of panesophageal pressurization in ≥ 20 % of swallows. Type III Achalasia can have preserved fragments of distal peristalsis or premature (spastic) contractions in ≥ 20 % of swallows. Representative HRM tracings of the three subtypes of Achalasia are shown in Fig. 1.
HRM pressure topography maps by subtype: a) Type I Achalasia: Mean IRP > upper limit of normal, 100 % failed peristalsis b) Type II Achalasia: Mean IRP > upper limit of normal, no normal peristalsis, panesophageal pressurization with ≥ 20 % of swallows c) Type III Achalasia: Mean IRP > upper limit of normal, no normal peristalsis, preserved fragments of distal peristalsis or premature (spastic) contractions with ≥ 20 % of swallows
Myotomy
The myotomy was done either as a surgical myotomy with partial fundoplication or using the POEM technique. Our technique for surgical myotomy has previously been reported [6]. The myotomy was performed along the left side of the esophagus from the hiatus down 3 cm onto the stomach and combined with a Dor or Toupet fundoplication. The POEM procedure included a mucosotomy 10–15 cm proximal to the gastroesophageal junction (GEJ) at the 2 o’clock position. A submucosal tunnel was developed and extended 3 cm distal to the GEJ. Myotomy of the circular muscle fibers was initiated 3–5 cm distal to the mucosotomy and continued to the end of the submucosal tunnel. The mucosotomy was closed with clips.
Statistical analysis
Statistical analysis was performed using Prism 4 Statistical Software (GraphPad Software, Inc. La Jolla, CA). Comparison between groups was performed using the Kruskall Wallis one-way analysis of variance and Dunn’s test where appropriate. A p value less than 0.05 was considered statistically significant. Median values are reported with interquartile range (IQR) except where indicated.
Results
Patient characteristics and manometric findings
There were 49 patients who met the inclusion criteria, 21 males and 28 females. The median age was 52 years (range 20–76 years). By HRM, the subtype of Achalasia was Type I in ten patients (20 %), Type II in 30 patients (61 %), and Type III in nine patients (18 %). Patient characteristics by Achalasia subtype are shown in Table 2. Patients with Type I Achalasia tended to be younger than patients with the other Achalasia subtypes. The median duration of symptoms before presentation was 4 years (range 4 months–50 years) and was not different between subtypes. The primary symptom in all patients was dysphagia. Previous endoscopic treatment with Botox or balloon dilatation had been performed in 45 % of patients and was similar across subtypes. There was no difference in the frequency of hiatal hernia, Barrett’s esophagus, median pre-operative BMI, or weight loss prior to therapy between groups. Patients with Type I Achalasia had a lower pre-myotomy resting pressure than patients with the other Achalasia subtypes (p = 0.03). The median IRP was 22 mmHg (IQR 14–31 mmHg) and the median percent relaxation of the sphincter was 22 % (IQR 11–38) and did not differ between subtypes. No patient had complete emptying at 1 or 5 min on pre-myotomy timed barium study.
Symptomatic and objective outcome
A laparoscopic (n = 38) or trans-abdominal (n = 1) Heller myotomy was performed in 39 patients (80 %) and POEM was performed in ten patients (20 %). The type of operation and outcome are shown in Table 3. There was no difference in type of operation between groups. At a median follow-up of 16 months (range 1–63 months), dysphagia was relieved in 90 % of patients and was similar across subtypes. Dysphagia persisted in five patients, all of whom had a laparoscopic Heller myotomy. The median Eckardt score after myotomy was zero, but patients with Type I Achalasia had a slightly higher Eckardt score and tended to have more esophageal retention on timed barium study. Post-operative reflux was experienced by nine patients (18 %), six patients with Heller myotomy and three patients with POEM. Treatment was with PPI in seven patients and diet modification in two patients. There was no statistically significant difference in post-operative reflux between Achalasia subtypes.
Discussion
The development of high-resolution manometry catheters with 36 solid state sensors and software that graphically displays pressure topography (Clouse plots) has revolutionized the evaluation of esophageal function [7]. During HRM, the esophageal body and the upper and lower sphincters can now be evaluated simultaneously, allowing for more complete characterization of esophageal motility disorders [8, 9]. This has led to the reclassification of conditions such as Achalasia. The most widely accepted of these classification systems is the “Chicago Classification” in which there are three distinct sub-classes of Achalasia [1, 5, 8–10]. Type II Achalasia is the most common and Type III is the least common subtype [11, 12].
The clinical relevance of these Achalasia subtypes on treatment outcome is not well established and is the subject of much current investigation. Several studies have suggested that symptomatic outcome differs based on Achalasia subtype, with the best results in patients with Type II Achalasia [1, 11, 13, 14]. In our study, we found no significant difference based on subtype with a high rate of symptom resolution in all types of Achalasia. We did find that relief of dysphagia was highest (93 %) in Type II Achalasia, but the difference was not statistically significant. Symptomatic outcome has been reported to be worst in patients with Type III Achalasia [1, 11, 13, 14]. The majority of these reports assessed outcome after balloon dilatation where success rates ranged from 29 to 66 % [1, 11, 13, 14]. Symptomatic results after Heller myotomy for Type III Achalasia have been reported to be superior to those with balloon dilatation [11]. In this series, we found that both symptomatic and objective results were excellent in these patients after myotomy. Dysphagia was relieved in 89 %, the post-operative Eckardt score was zero in 78 %, and there was complete emptying at 5 min on timed barium study in 100 % of patients with Type III Achalasia.
In this series, patients with Type I Achalasia tended to have the worst outcome. The median post-operative Eckardt score was higher and only 80 % of patients had complete relief of symptoms. Further, only 14 % of patients had complete emptying at 5 min on post-operative timed barium study. These patients had a significantly lower LES resting pressure than the other subtypes, and we have previously shown that pre-operative LES resting pressure is the only predictor of outcome after myotomy, with the best results occurring in patients with higher LES pressures [6]. The results of this current study confirm this finding. We made this observation before the introduction of HRM and Achalasia subtyping, and it is interesting to speculate that perhaps the patients with the lower LES resting pressures and poorer outcome were those with Type I Achalasia.
The limitations of our study include its retrospective nature and the small number of patients in each group. This introduces the potential for a Type II error and makes firm statements about equivalency of results between groups difficult. Future studies with larger numbers of patients will be necessary to confirm our findings. Our small numbers also prevented a comparison of the outcomes between Heller myotomy and the POEM procedure. However, a strength of our study is that all patients were evaluated with HRM and classified according to the most recent version of the Chicago classification. Further, patients were evaluated not only for symptomatic outcome but with objective assessment of esophageal emptying by timed barium study.
Conclusion
High-resolution manometry identifies three subtypes of Achalasia. We found that myotomy results in excellent symptomatic outcome and improvement in esophageal clearance in all Achalasia subtypes. This calls into question the clinical utility of Achalasia sub-classification when considering Heller myotomy or POEM and affirms the benefit of myotomy for all subtypes of this disease. In particular, our excellent results with Type III Achalasia patients suggest these patients should preferentially be treated with surgical myotomy or the POEM procedure.
References
Pandolfino JE, Kwiatek MA, Nealis T, Bulsiewicz W, Post J, Kahrilas PJ (2008) Achalasia: A new clinically relevant classification by high-resolution manometry. Gastroenterology 135:1526–1533
Eckardt A, Eckardt VF (2011) Treatment and surveillance strategies in Achalasia: an update. Nat. Rev. Gastroenterol Hepatol 8:311–319
Fuller L, Huprich JE, Theisen J, Hagen JA, Crookes PF, DeMeester SR, Bremner CG, DeMeester TR, Peters JH (1999) Abnormal esophageal body function: radiographic-manometric correlation. The American Surgeon 65:911–914
Ayazi S, Hagen JA, Zehetner J, Ross O, Wu C, Oezcelik A, Abate E, Sohn HJ, Bank F, Lipham JC, DeMeester SR, DeMeester TR (2009) The Value of high-resolution manometry in the assessment of the resting characteristics of the lower esophageal sphincter. J Gastrointest Surg 13:2113–2120
Carlson DA, Pandolfino JE (2013) High-resolution manometry and esophageal pressure topography filling the gaps of convention manometry. Gastroenterol Clin N Am 42:1–15
Arain MA, Peters JH, Tamhankar AP, Portale G, DeMeester SR, Crookes PF, Hagen JA, Bremner CG, DeMeester TR (2004) Preoperative lower esophageal sphincter pressure affects outcome of laparoscopic esophageal myotomy for Achalasia. J Gastrointest Surg 8:328–334
Conklin JL (2013) Evaluation of esophageal motor function with high-resolution manometry. J Neurogastroenterol Motil 19:281–294
Kahrilas PJ, Ghosh SK, Pandolfino JE (2008) Esophageal motility disorders in terms of pressure topography. J Clin Gastroenterol 42:627–635
Kahrilas PJ (2010) Esophageal motor disorders in terms of high-resolution esophageal pressure topography: what has changed? Am J Gastroenterol 105:981–987
Bredenoord AJ, Fox M, Kahrilas PJ, Pandolfino JE, Schwizer W, Smout AJPM, Conklin JL, Cook IJ, Gyawali P, Hebbard G, Holloway RH, Ke M, Keller J, Mittal R, Peters J, Richter J, Roman S, Rommel N, Sifrim D, Tutuian R, Valdovinos M, Vela MF, Zerbib F (2012) Chicago classification criteria of esophageal motility disorders defined in high resolution esophageal pressure topography (EPT). Neurogastroenterol Motil 24:57–65
Rohof W, Salvador R, Annese V, Des Varannes SB, Chaussade S, Constantini M, Elizalde JI, Gaudric M, Smouth AJ, Tack J, Busch O, Zaninotto G, Boeckxstaens GE (2013) Outcomes of treatment for Achalasia depend on manometric subtype. Gastroenterology 144:718–725
Roman S, Zerbib F, Quenehervé L, Clermidy H, Des Varannes SB, Mion F (2012) The Chicago classification for Achalasia in a french multicentric cohort. Digestive and Liver Disease 44:976–980
Pratap N, Kalapala R, Darisetty S, Joshi N, Ramchandani M, Banerjee R, Lakhtakia S, Gupta R, Tandan M, Rao G, Reddy DN (2011) Achalasia cardia subtyping by high-resolution manometry predicts the therapeutic outcome of pneumatic balloon dilatation. J Neurogastroenterol Motil 17:48–53
Salvador R, Constantini M, Zaninotto G, Morbin T, Rizzetto C, Zanatta L, Ceolin M, Finotti E, Nicoletti L, Dalt GD, Cavallin F, Ancona E (2010) The Preoperative manometric pattern predicts the outcome of surgical treatment for esophageal Achalasia. J Gastrointest Surg 14:1635–1645
Pandolfino JE (2013) Uncovering hidden information in Achalasia using esophageal pressure topography. Gastroenterology 144:681–690
Acknowledgments
None.
Disclosures
Drs. Greene, Chang, Oh, Worrell, and Hagen have nothing to disclose.
Dr. DeMeester is a consultant for Davol, Gore, Novadaq and C2 Therapeutics, none of which are relevant to this work.
Funding
None.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Greene, C.L., Chang, E.J., Oh, D.S. et al. High resolution manometry sub-classification of Achalasia: does it really matter?. Surg Endosc 29, 1363–1367 (2015). https://doi.org/10.1007/s00464-014-3804-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00464-014-3804-3