Abstract
Background
Laparoscopic hepatectomy (Lap-Hx) has been increasingly performed for patients with liver tumors as surgical techniques and devices have progressed. However, the long-term outcomes of Lap-Hx for malignant liver tumors are not oncologically guaranteed. This study compared the short- and long-term outcomes between Lap-Hx and open hepatectomy (Open-Hx) for malignant liver tumors by matched-pair analysis.
Methods
The indications for Lap-Hx at our department are a tumor size of <5 cm and fewer than two lesions without macroscopic vascular invasion or the need for biliary reconstruction. In total, 135 patients underwent Lap-Hx for malignant liver tumors through December 2013. We compared the short- and long-term outcomes between Lap-Hx and Open-Hx in patients who met the above-mentioned indications.
Results
With respect to short-term outcomes, the operation time, blood loss, postoperative hospital stay, white blood cell count, and C-reactive protein level after Lap-Hx were significantly better than those after Open-Hx in both the patients who underwent partial resection and those who underwent lateral sectionectomy. In patients who underwent partial resection, the incidence of postoperative complications after Lap-Hx was significantly lower than that after Open-Hx; in particular, wound infection and respiratory complications were significantly lower. Furthermore, when the tumor was located in the posterosuperior segments, the operation time for Lap-Hx was not shorter than that for Open-Hx. With respect to long-term outcomes of hepatocellular carcinoma, neither overall nor disease-free survival differed between the two groups. With respect to long-term outcomes of colorectal liver metastases, the disease-free survival rate was similar between Lap-Hx and Open-Hx; however, the overall survival rate was significantly better for Lap-Hx than for Open-Hx.
Conclusions
Lap-Hx is a good option for selected patients with malignant liver tumors. The short- and long-term outcomes of Lap-Hx also are considered to be acceptable.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Laparoscopic hepatectomy (Lap-Hx) was reported for the first time by Gagner et al. [1] in 1992. Initially, Lap-Hx for hepatic diseases was limited to centers with experience in laparoscopic surgery because of difficulties with the technique and bleeding control. Previous studies [2, 3] on laparoscopic liver resection demonstrated that the procedure was feasible and safe, and did not increase tumor dissemination. With the progression of surgical techniques and devices, Lap-Hx became a realizable option for patients with liver tumors. Since then, Lap-Hx has been gradually accepted as a treatment of choice for benign and malignant hepatic diseases and has been performed in about 3,000 patients to date. Conversely, open hepatectomy (Open-Hx) is the gold standard treatment for colorectal liver metastasis (CRLM) and hepatocellular carcinoma (HCC) [2–4]. However, the short- and long-term outcomes of Lap-Hx for malignant hepatic disease remain unclear. Therefore, in this study, we compared the short- and long-term outcomes between Lap-Hx and Open-Hx for patients with CRLM and HCC by matched-pair analysis.
Materials and methods
Patient selection for laparoscopic hepatectomy
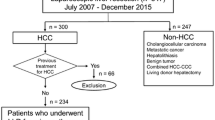
From January 2006 to December 2013, a total of 135 patients underwent Lap-Hx for malignant liver tumors at Osaka Medical College Hospital. The indications for Lap-Hx at our department are a tumor size of <5 cm and fewer than two lesions without macroscopic vascular invasion or the need for biliary reconstruction. There are no limitations regarding tumor location, and liver function requirements are identical to those for Open-Hx. However, even when tumors satisfied the above-mentioned conditions in the present study, the final decision was the surgeon’s because performance of the laparoscopic procedure involved a specialized technique.
Two analyses were performed in this study. The first compared the short-term outcomes of Lap-Hx and Open-Hx according to the type of hepatectomy. The second examined the long-term outcomes according to the disease.
Short-term outcomes
Partial resection and lateral sectionectomy were targeted in this study because there were fewer cases of other procedures involving Lap-Hx, such as anterior, posterior, and medial sectionectomy and hemihepatectomy. In total, 117 and 234 patients underwent Lap-Hx and Open-Hx, respectively, under the above-mentioned conditions through December 2013. Of the 117 patients who underwent Lap-Hx, 93 underwent partial resection and 24 underwent lateral sectionectomy. Of the 234 patients who underwent Open-Hx, 200 underwent partial resection and 34 underwent lateral sectionectomy. Perioperative outcomes, including postoperative complications, were compared between these two groups.
Long-term outcomes
From April 2000 to December 2011, 172 patients underwent initial hepatectomy for HCC under the above-mentioned tumor conditions; of these, 37 patients underwent Lap-Hx and 135 underwent Open-Hx. Furthermore, 124 patients underwent initial hepatectomy for CRLM; of these, 46 patients underwent Lap-Hx, and 78 underwent Open-Hx.
Surgical procedure
In general, the minimally invasive approach to hepatectomy can be performed by pure laparoscopy. However, a small-incision approach was very frequently performed in the introductory period of laparoscopic surgery; at that time, tumors were difficult to locate by pure laparoscopy because of the limited visualization and difficulty in controlling bleeding [5]. Thus, we chose the small-incision approach in the present study. For Lap-Hx, each patient was placed in the supine position; when lesions were located in the right lateral sector, patients were placed in the left lateral decubitus position. Trocars were inserted using an open technique, and continuous carbon dioxide pneumoperitoneum was established at a pressure of <12 mmHg to avoid gas embolism. The transection line was determined by intraoperative ultrasonography to evaluate and determine the tumor status. Parenchymal transection was performed using a laparoscopic ultrasonic surgical aspirator and laparoscopic coagulating shears. Hemostasis was performed using monopolar forceps with soft coagulation (VIO System™). The Pringle maneuver using an endoscopic intestinal clip was performed if necessary [6]. Open-Hx was performed following the standard technique as previously described [7]. Although a drain was routinely used until 2006, we thereafter inserted a drain by our previously established standard [8].
Statistical analysis
Actuarial survival rates were calculated using the Kaplan–Meier method. Univariate analyses were performed using the log-rank test. Multivariate analyses were performed by Cox proportional hazards regression. Statistical comparisons were made by Fisher’s exact probability test. All analyses were performed using the JMP version 9.0 software package (SAS Institute, Cary, NC, USA) on Mac OS X. Values of p < 0.05 were considered statistically significant.
Results
Laparoscopic hepatectomy for malignant liver tumors was performed for 137 patients (including assisted Lap-Hx in 37 patients). Of these, 74 and 61 patients underwent Lap-Hx for CRLM and HCC, respectively. Most Lap-Hx procedures comprised partial Hx (93 patients) and lateral sectionectomy (24 patients). Eleven patients were converted from Lap-Hx to Open-Hx, four underwent conversion because of a high risk of major bleeding, four underwent conversion because of severe adhesion, two underwent conversion because of poor visualization of the transection line, and one was converted to ensure a sufficient oncologic margin (Table 1).
Short-term outcomes
With respect to partial resection, although the indocyanine green retention rate at 15 min in Open-Hx was higher than that in Lap-Hx, there was no difference in pathological cirrhosis between the two groups. The operation time (p = 0.0139) and blood loss (p < 0.0001) in Lap-Hx were significantly lower than those in Open-Hx. Furthermore, the incidence of postoperative complications in Lap-Hx was significantly lower than that in Open-Hx; in particular, wound infection (p = 0.0009) and respiratory complications (p = 0.0344) were significantly lower. The postoperative hospital stay in the Lap-Hx group was shorter than that in the Open-Hx group (10 vs. 16 days, respectively; p < 0.0001). The surgical margin in Lap-Hx was more secure than that in Open-Hx (Table 2). The detailed examination according to the tumor location in partial resection revealed a significantly better operation time (p = 0.0286), blood loss (p = 0.0015), wound infection rate (p = 0.0007), respiratory complication rate (p = 0.0341), and postoperative hospital stay (p < 0.0001) in Lap-Hx than in Open-Hx for tumors of the anterolateral segments. When tumors were located in the posterosuperior segments, partial resection in Lap-Hx was associated with less blood loss (p = 0.0063) and a shorter postoperative hospital stay (p = 0.0027) than in Open-Hx (Table 3).
With respect to lateral sectionectomy, the operation time (p = 0.0345) and blood loss (p = 0.0002) in Lap-Hx were significantly lower than those in Open-Hx. The postoperative hospital stay in the Lap-Hx group was shorter than in the Open-Hx group (9 vs. 15 days, respectively; p = 0.0163) (Table 2).
In both partial resection and lateral sectionectomy, the postoperative white blood cell count and C-reactive protein level tended to be lower in the Lap-Hx group than in the Open-Hx group (Fig. 1).
Postoperative white blood cell count and C-reactive protein level. Data for Lap-Hx are shown by a thick line, and data for Open-Hx are shown by a dotted line. A Partial resection: The postoperative white blood cell count and C-reactive protein level tended to be lower after Lap-Hx than after Open-Hx. B Lateral sectionectomy: The postoperative white blood cell count and C-reactive protein level tended to be lower after Lap-Hx than after Open-Hx
Long-term outcomes
With respect to the long-term outcomes of HCC, the 1-, 3-, and 5-year disease-free survival rates were 81, 52, and 52 %, respectively, after Lap-Hx and 81, 54, and 45 %, respectively, after Open-Hx (p = 0.9373) (Fig. 2A). Alternatively, the 1-, 3-, and 5-year overall survival rates were 97, 90, and 84 %, respectively, after Lap-Hx and 96, 84, and 67 %, respectively, after Open-Hx (p = 0.7052) (Fig. 2B). The two groups did not differ significantly in terms of overall or disease-free survival.
Disease-free (A) and overall (B) survival curves after hepatectomy for small (≤5 cm) HCC without macroscopic vascular invasion in laparoscopic hepatectomy (Lap-Hx) and open hepatectomy (Open-Hx). Data for Lap-Hx (n = 37) are shown by a thick line, and data for Open-Hx (n = 135) are shown by a dotted line. A There were no significant differences in disease-free survival between the two groups. B The overall survival curves were very similar between the two groups, and there were no significant differences between them
With respect to the long-term outcomes of CRLM, the 1-, 3-, and 5-year disease-free survival rates were 61, 41, and 41 %, respectively, after Lap-Hx. The corresponding rates for Open-Hx were 58, 41, and 38 %, respectively (p = 0.6591) (Fig. 3A). On the other hand, the 1-, 3-, and 5-year overall survival rates after Lap-Hx were significantly better than those after Open-Hx (100, 88, and 88 vs. 96, 68, and 53 %, respectively; p = 0.0042) (Fig. 3B).
Disease-free (A) and overall (B) survival curves after hepatectomy for small (≤5 cm) CRLM of fewer than two lesions without macroscopic vascular invasion in laparoscopic hepatectomy (Lap-Hx) and open hepatectomy (Open-Hx). Data for Lap-Hx (n = 37) are shown by a thick line, and data for Open-Hx (n = 135) are shown by a dotted line. A There was no significant difference in disease-free survival between the two groups. B The overall survival curve of Lap-Hx was significantly better than that of Open-Hx (100, 88, and 88 vs. 96, 68, and 53 %, respectively; p = 0.0042)
Discussion
This single-institution study compared the short- and long-term outcomes of Lap-Hx with those of Open-Hx under the conditions of a tumor size of <5 cm, fewer than two lesions, and no macroscopic vascular invasion or need for biliary reconstruction. With respect to the short-term outcomes of partial resection and lateral sectionectomy, we found that operation time, blood loss, postoperative early white blood cell count, and C-reactive protein level for Lap-Hx were significantly lower than those for Open-Hx; in addition, the hospital stay for Lap-Hx tended to be shorter than that for Open-Hx. Furthermore, with respect to partial resection, the wound infection and pulmonary complication rates after Lap-Hx were significantly lower than those after Open-Hx. Regarding the long-term outcomes of HCC and CRLM, there were no significant differences in the overall or disease-free survival between the Lap-Hx and Open-Hx groups.
Since the report by Kaneko et al. [9] in 1996, many authors have indicated better results with Lap-Hx than Open-Hx with respect to short-term outcomes [10–20], wound pain [14], operation time [14, 15], blood loss [11, 14–17, 19, 20], postoperative complications [15], postoperative analgesic requirements [15], time to regular diet [11, 14], overall cost [11], postoperative hospital stay [10, 11, 15, 17–20], and other factors. This study also indicated the same benefits as those described in previous reports; furthermore, new pulmonary complications such as atelectasis or pneumonia were lower in the Lap-Hx group than in the Open-Hx group.
Thus, clinicians should be aware of the higher risk of postoperative pulmonary complications in patients undergoing hepatectomy, especially because pulmonary complications are associated with a worse prognosis in elderly patients than in younger patients [21–23]. Recent reports suggest that the rate of pulmonary complications may be lower with laparoscopic surgery than with open surgery [24], and this strategy will likely be the subject of future investigation. With respect to patients with cirrhosis, although there was no significant difference in the rate of intractable ascites and liver failure between the two groups in the present study, Kanazawa et al. [15] reported that Lap-Hx decreased the incidence of intractable ascites because this procedure minimizes blockage of the collateral circulation around the liver and abdominal wall, thus preventing lymphatic flow disturbance and postoperative portal hypertension, and minimizes parenchymal damage in comparison with Open-Hx. Lap-Hx is therefore a more useful procedure than Open-Hx for patients with poor liver function.
In terms of blood loss, most reports on Lap-Hx have shown lower bleeding volumes than those on Open-Hx [11, 14–17, 19, 20]. However, whether bleeding from small vessels can be better prevented by continuous abdominal pressure or the use of new coagulation and transection devices remains unclear. Conversely, it was found that the operation time was prolonged by inexperience with laparoscopic surgery. However, the operation time was not longer for Lap-Hx than for Open-Hx; rather, the operation time for laparoscopic lateral sectionectomy and partial resection of peripheral lesions was significantly shorter than that for Open-Hx [25, 26]. On the contrary, when the tumor was located in the posterosuperior segments (segments 4a, 7, and 8), partial resection in Lap-Hx was associated with lower blood loss volumes, but not shorter operation times, compared with Open-Hx. In previous reports, most surgeons have considered that Lap-Hx for lesions located in the posterosuperior segments is not appropriate because of the limited visualization and difficult control of bleeding. On the contrary, some recent reports have proposed the use of Lap-Hx for lesions located in the posterosuperior segments [16, 27–30]. In this study, the operation time gradually decreased to 222 min in the later period from 298 min in the early period with improvements in surgical techniques such as the insertion of intercostal ports and the use of the semi-prone position (data not shown) [31]. This will be further improved as the learning curve improves in the future.
With respect to long-term outcomes, although previous reports on Lap-Hx described fewer patients and shorter observation periods, the overall and disease-free survival rates were similar between Lap-Hx and Open-Hx for both CRLM [19, 32] and HCC [33, 34]. The overall and disease-free survival rates of patients with HCC with a tumor size of ≤5 cm and without macroscopic vascular invasion were similar between the Lap-Hx and Open-Hx groups in the present study. Although whether anatomical resection is necessary for small HCC remains controversial, a previous report showed that nonanatomical resection is more useful than anatomical resection for HCC under the above-mentioned tumor conditions [35].
In patients with CRLM, the disease-free survival rate was similar between the Lap-Hx and Open-Hx groups; however, the overall survival rate in the Lap-Hx group was better than that in the Open-Hx group in this study. Furthermore, we re-examined overall survival after adjustment for tumor background because local development of the original tumor has an influence on the overall survival; however, the overall survival after Lap-Hx was better than that after Open-Hx even with this adjustment. We speculate that this may have been associated with the fact that Lap-Hx was performed with the administration of a new anticancer agent, such as FOLFOX, at the time of recurrence in contrast to Open-Hx, which was performed with the administration of more outdated anticancer agents, and with the fact that the observation periods for Lap-Hx were shorter than these for Open-Hx.
In conclusion, regardless of the presence of HCC or CRLM, Lap-Hx is the better option for patients with a tumor size of <5 cm, fewer than two lesions, and no macroscopic vascular invasion. However, a study involving a larger number of patients is necessary to obtain definitive conclusions. Furthermore, it is necessary to establish the Lap-Hx technique for tumors located in the posterosuperior segment to ensure that the performance of Lap-Hx becomes more widespread.
References
Gagner MRM, Dubuc J (1992) Laparoscopic partial hepatectomy for liver tumor. In: Abstracts of the 1992 Scientific Session of the Society of American Gastrointestinal Surgeons (SAGES). Surg Endosc. 6:85–110 11–2 April 1992, Washington DC, USA
Abdalla EK, Adam R, Bilchik AJ, Jaeck D, Vauthey JN, Mahvi D (2006) Improving resectability of hepatic colorectal metastases: expert consensus statement. Ann Surg Oncol 13(10):1271–1280
Fong Y, Fortner J, Sun RL, Brennan MF, Blumgart LH (1999) Clinical score for predicting recurrence after hepatic resection for metastatic colorectal cancer: analysis of 1001 consecutive cases. Ann Surg 230(3):309–318 discussion 18-21
Cha CH, Ruo L, Fong Y, Jarnagin WR, Shia J, Blumgart LH et al (2003) Resection of hepatocellular carcinoma in patients otherwise eligible for transplantation. Ann Surg 238(3):315–321 discussion 21-3
Nitta H, Sasaki A, Fujita T, Itabashi H, Hoshikawa K, Takahara T et al (2010) Laparoscopy-assisted major liver resections employing a hanging technique: the original procedure. Ann Surg 251(3):450–453
Komeda K, Hayashi M, Inoue Y, Shimizu T, Asakuma M, Hirokawa F et al (2013) Clinical usefulness of endo intestinal clips during Pringle’s maneuver in laparoscopic liver resection: a technical report. Surg Laparosc Endosc Percutan Tech 23(3):e103–e105
Hirokawa F, Hayashi M, Miyamoto Y, Iwamoto M, Tsunematsu I, Asakuma M et al (2011) A novel method using the VIO soft-coagulation system for liver resection. Surgery 149(3):438–444
Hirokawa F, Hayashi M, Miyamoto Y, Asakuma M, Shimizu T, Komeda K et al (2011) Re-evaluation of the necessity of prophylactic drainage after liver resection. Am Surg 77(5):539–544
Kaneko H, Takagi S, Shiba T (1996) Laparoscopic partial hepatectomy and left lateral segmentectomy: technique and results of a clinical series. Surgery 120(3):468–475
Shimada M, Hashizume M, Maehara S, Tsujita E, Rikimaru T, Yamashita Y et al (2001) Laparoscopic hepatectomy for hepatocellular carcinoma. Surg Endosc 15(6):541–544
Tsinberg M, Tellioglu G, Simpfendorfer CH, Walsh RM, Vogt D, Fung J et al (2009) Comparison of laparoscopic versus open liver tumor resection: a case-controlled study. Surg Endosc 23(4):847–853
Ker CG, Chen HY, Juan CC, Chang WS, Tsai CY, Lo HW et al (2000) Laparoscopic subsegmentectomy for hepatocellular carcinoma with cirrhosis. Hepatogastroenterology 47(35):1260–1263
Azagra JS, Goergen M, Gilbart E, Jacobs D (1996) Laparoscopic anatomical (hepatic) left lateral segmentectomy-technical aspects. Surg Endosc 10(7):758–761
Kaneko H, Takagi S, Otsuka Y, Tsuchiya M, Tamura A, Katagiri T et al (2005) Laparoscopic liver resection of hepatocellular carcinoma. Am J Surg 189(2):190–194
Kanazawa A, Tsukamoto T, Shimizu S, Kodai S, Yamazoe S, Yamamoto S et al (2013) Impact of laparoscopic liver resection for hepatocellular carcinoma with F4-liver cirrhosis. Surg Endosc 27(7):2592–2597
Chen HY, Juan CC, Ker CG (2008) Laparoscopic liver surgery for patients with hepatocellular carcinoma. Ann Surg Oncol 15(3):800–806
Iwahashi S, Shimada M, Utsunomiya T, Imura S, Morine Y, Ikemoto T et al (2014) Laparoscopic hepatic resection for metastatic liver tumor of colorectal cancer: comparative analysis of short- and long-term results. Surg Endosc 28(1):80–84
Inoue Y, Hayashi M, Tanaka R, Komeda K, Hirokawa F, Uchiyama K (2013) Short-term results of laparoscopic versus open liver resection for liver metastasis from colorectal cancer: a comparative study. Am Surg 79(5):495–501
Guerron AD, Aliyev S, Agcaoglu O, Aksoy E, Taskin HE, Aucejo F et al (2013) Laparoscopic versus open resection of colorectal liver metastasis. Surg Endosc 27(4):1138–1143
Cheung TT, Poon RT, Yuen WK, Chok KS, Jenkins CR, Chan SC et al (2013) Long-term survival analysis of pure laparoscopic versus open hepatectomy for hepatocellular carcinoma in patients with cirrhosis: a single-center experience. Ann Surg 257(3):506–511
Zilberberg MD, Epstein SK (1998) Acute lung injury in the medical ICU: comorbid conditions, age, etiology, and hospital outcome. Am J Respir Crit Care Med 157(4 Pt 1):1159–1164
Fuso L, Cisternino L, Di Napoli A, Di Cosmo V, Tramaglino LM, Basso S et al (2000) Role of spirometric and arterial gas data in predicting pulmonary complications after abdominal surgery. Respir Med 94(12):1171–1176
Smith PR, Baig MA, Brito V, Bader F, Bergman MI, Alfonso A (2010) Postoperative pulmonary complications after laparotomy. Respiration 80(4):269–274
Jiang L, Yang KH, Guan QL, Cao N, Chen Y, Zhao P et al (2013) Laparoscopy-assisted gastrectomy versus open gastrectomy for resectable gastric cancer: an update meta-analysis based on randomized controlled trials. Surg Endosc 27(7):2466–2480
Cherqui D, Husson E, Hammoud R, Malassagne B, Stephan F, Bensaid S et al (2000) Laparoscopic liver resections: a feasibility study in 30 patients. Ann Surg 232(6):753–762
Laurent A, Cherqui D, Lesurtel M, Brunetti F, Tayar C, Fagniez PL (2003) Laparoscopic liver resection for subcapsular hepatocellular carcinoma complicating chronic liver disease. Arch Surg 138(7):763–769 discussion 9
Koffron AJ, Auffenberg G, Kung R, Abecassis M (2007) Evaluation of 300 minimally invasive liver resections at a single institution: less is more. Ann Surg 246(3):385–392 discussion 92-4
Cho JY, Han HS, Yoon YS, Shin SH (2008) Experiences of laparoscopic liver resection including lesions in the posterosuperior segments of the liver. Surg Endosc 22(11):2344–2349
Teramoto K, Kawamura T, Takamatsu S, Nakamura N, Kudo A, Noguchi N et al (2005) Laparoscopic and thoracoscopic approaches for the treatment of hepatocellular carcinoma. Am J Surg 189(4):474–478
Cho JY, Han HS, Yoon YS, Shin SH (2008) Feasibility of laparoscopic liver resection for tumors located in the posterosuperior segments of the liver, with a special reference to overcoming current limitations on tumor location. Surgery 144(1):32–38
Ikeda T, Mano Y, Morita K, Hashimoto N, Kayashima H, Masuda A et al (2013) Pure laparoscopic hepatectomy in semiprone position for right hepatic major resection. J Hepatobiliary Pancreat Sci 20(2):145–150
Castaing D, Vibert E, Ricca L, Azoulay D, Adam R, Gayet B (2009) Oncologic results of laparoscopic versus open hepatectomy for colorectal liver metastases in two specialized centers. Ann Surg 250(5):849–855
Ito K, Ito H, Are C, Allen PJ, Fong Y, DeMatteo RP et al (2009) Laparoscopic versus open liver resection: a matched-pair case control study. J Gastrointest Surg 13(12):2276–2283
Sarpel U, Hefti MM, Wisnievsky JP, Roayaie S, Schwartz ME, Labow DM (2009) Outcome for patients treated with laparoscopic versus open resection of hepatocellular carcinoma: case-matched analysis. Ann Surg Oncol 16(6):1572–1577
Tomimaru Y, Eguchi H, Marubashi S, Wada H, Kobayashi S, Tanemura M et al (2012) Equivalent outcomes after anatomical and non-anatomical resection of small hepatocellular carcinoma in patients with preserved liver function. Dig Dis Sci 57(7):1942–1948
Disclosures
Drs. Fumitoshi Hirokawa, Michihiro Hayashi, Yoshiharu Miyamoto, Mitsuhiro Asakuma, Tetsunosuke Shimizu, Koji Komeda, Yoshihiro Inoue, and Kazuhisa Uchiyama have no conflict of interests or financial ties to disclose.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Hirokawa, F., Hayashi, M., Miyamoto, Y. et al. Short- and long-term outcomes of laparoscopic versus open hepatectomy for small malignant liver tumors: a single-center experience. Surg Endosc 29, 458–465 (2015). https://doi.org/10.1007/s00464-014-3687-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00464-014-3687-3