Abstract
Background
The initial focus of simulation in surgical education was to provide instruction in procedural tasks and technical skills. Recently, the importance of instruction in nontechnical areas, such as communication and teamwork, was realized. On rotation, the surgical resident requires proficiency in both technical and non-technical skills through the entire patient care pathway, i.e., pre-, intra- and postoperatively.
Methods
The focus was upon implementation of a biliary disease-based surgical simulation curriculum. The cornerstones of this module were clinical care pathway simulation sessions, at the commencement and conclusion of the 3 days. Each resident completed a simulated outpatient encounter with a standardized patient (SP) presenting with biliary colic, performed a laparoscopic cholecystectomy on a porcine model in a simulated operating room and completed an uncomplicated follow-up visit with the same SP. Assessments of resident performance were collected for every pathway scenario using standardized assessment forms approved by the American Board of Surgery. Additional formative sessions included hands-on, didactic and SP encounter sessions.
Results
The biliary surgical simulation pathway curriculum was successful implemented over the course of a 3-day, immersive module. The curriculum was delivered within the Penn Medicine Clinical Simulation Center and accommodated six junior surgical resident learners. The curriculum was divided into 4-h sessions, each led by a department faculty member. The cost of the implementation approximated $17,500 (USD).
Conclusion
It is imperative that surgical residents undergo simulation training directly linked to their hospital responsibilities so as to provide immediate performance improvement and reduce errors in the clinical environment. This pathway curriculum has successfully shown the feasibility to implement this novel approach to surgical simulation for junior resident training at an academic medical center. Such a patient-focused approach to surgical simulation should lead to higher-quality training for residents and supports the use of this pathway curriculum in the future.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Simulation-based training in surgery is now becoming widespread. Numerous initiatives have sprouted across the globe to engage residents and medical students into simulation-based learning activities [1]. The American College of Surgeons, together with the Association of Program Directors in Surgery, has formulated a three-phase national surgical skills curriculum [2]. This includes basic skills and tasks such as knot tying and upper endoscopy, advanced procedures such as appendectomy and sentinel node biopsy, and team-based skills of trauma team training and patient hand off. The Residency Review Committee for Surgery (under the umbrella of the Accreditation Council for Graduate Medical Education, or ACGME) has mandated that ‘simulation and skills facilities must be available for all program residents’ [3].
In terms of simulation-based assessment of surgical performance, the Society of American Gastrointestinal and Endoscopic Surgeons (SAGES) have led the way with the Fundamentals of Laparoscopic Surgery (FLS) program [4]. This is a ‘comprehensive web-based education module that includes a hands-on skills training component and assessment tool designed to teach the physiology, fundamental knowledge and technical skills required in basic laparoscopic surgery.’ Following review of the extensive validation and reliability testing that went into the program, in July 2009, the American Board of Surgery (ABS) required all graduating chief residents in general surgery pass the FLS program as part of their certification process. In concert with this move are further mandates from the ABS with regard to objective tools for the assessment of operative and clinical performance [5].
A further notion is the development and implementation of competency-based curricula, which follow an outcomes-achieved rather than time-focused approach to residency progression [6]. This has been recently exemplified by the publication of ACGME milestones for semiannual review of resident performance [7]. Milestones are based upon the six ACGME core competencies and graded according to four levels of performance. This initiative seeks to blur the distinction between surgeon competence and performance, in that residents are continuously evaluated and provided with constructive feedback throughout their training program.
Returning to simulation-based activities, the issue still remains that residents are being taught isolated activities such as chest drain insertion or postoperative wound care, in situations which are devoid of the overall context. The challenge for the resident is to incorporate the knowledge, skills and attitudes learnt during simulated encounters and translate this into their performance during fast-paced, multi-professional and often challenging clinical settings. This transition is at best difficult and occurs mostly through guidance, mentorship and support of the learner by other members of the clinical team. Thus, despite extensive simulation-based training, error and adverse events may still occur, notwithstanding the effect upon the learner’s confidence, perceived ability and further clinical progression.
The aim of this study was to incorporate clinical care pathways into a simulation-based training curriculum, which is focused upon a specific disease process. This report details the design, development and implementation of a simulation pathway curriculum for biliary disease, based upon pre-, intra- and postoperative clinical encounters. The focus was upon training of junior surgical residents, with incorporation of performance measures throughout the instructional period.
Design of the simulation pathway curriculum for biliary disease
In order to design a curriculum for junior residents to acquire the knowledge, skills and attitudes with regard to management of a patient with biliary disease, it was first necessary to develop a strategic framework. The start point with regard to a clinical syllabus was the SCORE (Surgical Council on Resident Education) Portal [8]. This provides a useful categorization of all aspects of biliary disease relevant to surgical residency education. A total of 27 categories are divided into 15 disease/conditions (e.g., acute cholecystitis and biliary pancreatitis) and 12 operation/procedures (e.g., cholecystectomy and choledochoscopy). Each category is also denoted to the relevant PGY level, ranging from 1 through to 5. As the curriculum is focused for junior surgical residents, the content was based upon the defined modules for PGY1 and PGY2 (Table 1).
This framework was then built upon the care pathway for patients with biliary disease which was divided into three parts, i.e., preoperative, intra-operative and postoperative. ACGME core competencies to be addressed at each part of the pathway were also defined (Table 2).
In terms of preoperative cases, the presentation could either be in an outpatient surgical clinic following referral by a primary care clinician, or to an emergency department if the symptoms were acute in nature. Typical cases were then defined, based upon expert consensus and review of the surgical literature, i.e., biliary colic, acute cholecystitis, biliary pancreatitis and choledocholithiasis. The intra-operative part of the curriculum sought to design an immersive operating room (OR) environment in which the surgical resident performs part of a simulated laparoscopic cholecystectomy with the whole OR team present, i.e., scrub nurse, first assistant and anesthesiologist [9]. Finally, for the postoperative part of the curriculum, clinical encounters were designed to be in the postoperative recovery room, outpatient surgical clinic or the emergency room [10]. Typical cases were again defined based upon expert consensus and review of the surgical literature, i.e., normal postoperative course, bile leak, postoperative bleeding and obstructive jaundice.
It was the intention to utilize different pedagogical methods of instruction throughout the simulation-based curriculum. These included didactic and video sessions, hands-on technical skills practice (with faculty surgeon and self-directed practice), immersive encounters with simulated patients, peer-engaged learning (i.e., residents watch and learn from each other), individual and group debrief sessions.
Development of the simulation pathway curriculum for biliary disease
The simulation curriculum is based upon a novel method of pre-, intra- and postoperative encounters for a single disease entity. This part of the manuscript details the resources necessary to develop the simulation curriculum.
Preoperative encounters
-
a.
Scenarios—the four preoperative scenarios to be used for this part of the curriculum were biliary colic, acute cholecystitis, biliary pancreatitis and choledocholithiasis. The development process entailed the writing of detailed case descriptions for each scenario by a content expert (hepatobiliary faculty surgeon), based upon a previously used structure. The intent was to develop a case description which could be used by a simulated patient (SP) to play the pre-defined role. The scenarios detailed the typical patient history, vital signs, physical findings and key questions for the SP to respond to, e.g., was your urine dark?
-
b.
Settings—of the four pre-defined scenarios, only biliary colic was appropriate for the outpatient clinic setting. The other three encounters would typically occur in the emergency room. These two environments were thus created in a simulation setting (Fig. 1A).
Fig. 1 A Simulated outpatient [preoperative] clinical environment, Penn Simulation Center, Philadelphia PA; B simulated operating room [intra-operative] clinical environment, Penn Simulation Center, Philadelphia PA; C simulated recovery ward [postoperative] clinical environment, Penn Simulation Center, Philadelphia PA
-
c.
Equipment—the main resource required for these scenarios are trained SPs. Once the case scripts had been defined, appropriate SP actors were identified and underwent training for the specific roles. In addition, laboratory and imaging reports were developed, as appropriate for each case.
Intra-operative encounter
-
a.
Scenario—this part of the pathway required the resident to complete a standard laparoscopic cholecystectomy procedure, on simulated tissue, in an immersive environment. Thus, the resident operated with a scrub assistant who participated by driving the laparoscopic camera as directed by the operator. There was also a simulated anesthetist present in the room, to further enhance the realism of the simulation. Both of these confederates were trained to perform in this role, in the same manner that the SPs had been trained for the other parts of this curriculum.
-
b.
Setting—a fully immersive simulated operating room, including operating room table, anesthetic machine, operating room lights and two laparoscopic monitors with video and insufflation equipment (Fig. 1B). To add to the realism of the setting, background music played on a radio in the room.
-
c.
Equipment—the simulated laparoscopic cholecystectomy comprised a cadaveric porcine liver/gallbladder block which had been placed into a synthetic body form box trainer [11]. The box trainer had a foam-covering to simulate an abdominal wall, through which four laparoscopic operating ports had been placed. The trainer box was placed onto the operating table and then covered with sterile surgical drape, to resemble a whole patient. Standard laparoscopic instruments were provided, including traumatic and atraumatic graspers, L-hook, curved scissors, clip applier and a laparoscopic specimen bag retrieval device. A zero-degree 10-mm camera was provided for the scrub assistant, with the image relayed to the two video monitors.
Postoperative encounter
-
a.
Scenario—as per the preoperative encounters, there were four postoperative scenarios which comprised uncomplicated recovery, postoperative hemorrhage, bile leak and obstructive jaundice. Once again, the scenarios were developed in concert with an experienced hepatobiliary faculty surgeon. The case description for these four scenarios enabled an SP to undertake the required role. The scenarios detailed the patient’s current clinical status, the knowledge of their operative procedure, and for the three complicated postoperative scenarios, their concerns with regard to deviation from the expected outcome.
-
b.
Settings—the uncomplicated scenario takes place in the outpatient clinic setting, 2 weeks following the operative procedure. The bile leak and obstructive jaundice scenarios occur with the patient presenting in the emergency room, at postoperative day 5 and 10, respectively. Finally, the postoperative hemorrhage occurs in the post-anesthesia recovery unit, approximately 4 h following completion of the operative procedure. As per the preoperative encounters, these environments were all created in a simulation setting (Fig. 1C).
-
c.
Equipment—once again, the primary resource for these scenarios are trained SPs, who have been trained to the case scripts, and perform appropriately. Furthermore, appropriate laboratory and imaging reports were provided as necessary for each case.
In addition to the pathway scenarios, the 3-day module included didactic, hands-on technical skills and peer-engaged learning sessions. These are described below.
Didactic sessions
A topic of importance with regard to biliary disease is gallstone pancreatitis. The ideal manner to teach this was through a didactic session, delivered by a hepatobiliary faculty surgeon and built upon problem-based learning. The information for this session was taken directly from the SCORE module for acute pancreatitis [8]. This consists of a series of case studies, which were transposed into PowerPoint slides, and then used as a source of discussion of relevant topics.
Hands-on technical skills sessions
-
a.
Basic laparoscopic skills—the junior residents were enrolled in previously validated virtual reality (VR) training curricula for step-wise acquisition of basic laparoscopic skills. The residents undertook skills and tasks on LapSim [Surgical Science, Göteborg, Sweden] and LapMentor [Simbionix, Airport City, Israel] VR simulators and worked through the relevant curricula under the guidance of an experienced laparoscopic trainer [12, 13]. The curricula were also proficiency-based, such that residents had to achieve pre-defined metrics on the easy modules, prior to progression onto medium and hard modules. The modules were initially based upon basic laparoscopic skills, which led to procedural tasks relevant to laparoscopic cholecystectomy.
-
b.
Laparotomy and Tissue Handling—a 2-h session involving three residents and a single faculty trainer, focused upon techniques for laparoscopic first entry, full laparotomy and closure of the abdomen. A commercially available simulated abdomen model was used [Limbs & Things, Bristol, UK], with standard operative instruments.
-
c.
Sutures, Staples and Energy—residents were educated on the safe and appropriate use of sutures, staplers and energy devices for both open and laparoscopic surgery. A faculty surgeon initially taught different suture types, and then, residents performed a side-to-side, functional end-to-end linear-stapled anastomosis, with suture closure of the common enterotomy, on a synthetic small bowel model [Limbs & Things, Bristol, UK]. Operating room safety through the use of energy devices was also addressed.
-
d.
Full Procedure Laparoscopic Cholecystectomy—a setup focused upon the technical skills to perform full procedure laparoscopic cholecystectomy utilized two complementary simulation models, i.e., a porcine cadaveric model [11], and a synthetic model [Limbs & Things, Bristol, UK]. Both models were set up in a body form box trainer and utilized real surgical instruments. The session was designed so that the faculty surgeon initially explained the technical aspects of the procedure through use of an edited intra-operative video (from the SCORE website), then demonstrated it on the porcine model and then had residents perform the full procedure under supervision on porcine and synthetic tissues.
Peer-engaged learning sessions
During the 3-day module, two sessions focused upon the preoperative and postoperative management of a variety of patients with biliary disease. For example, during the preoperative session, a single faculty surgeon and three residents were together for a period of 2 h. A single SP sequentially portrayed the role of the four preoperative scenarios as previously described, i.e., biliary colic, acute cholecystitis, biliary pancreatitis and choledocholithiasis. The first resident would enter the preoperative clinic room and engage with the SP for a maximum period of 20 min. During the interaction, the faculty surgeon and other two residents would observe a video monitor in a separate control room. At the end of the simulation, the resident who undertook the simulation would return to the control room, for a 10-min debrief of the scenario, led by the faculty surgeon. After this, a second resident would go to the preoperative simulation room to interact with the same SP, but this time in a different scenario, e.g., acute cholecystitis. After this, the third resident would undergo the simulation and so on. A similar paradigm was used to teach the postoperative scenarios. This enabled residents to learn not only through doing, but also through observation of their peers.
Resident assessment of performance
It was imperative to assess performance of resident interactions during the pre-, intra- and postoperative scenarios. The American Board of Surgery has recently approved the use of three forms for resident assessment of operative and clinical performance [5]. The forms are briefly described below and were used as appropriate for assessment of pre-, intra- and postoperative encounters:
-
1.
Clinical Assessment and Management Exam—Outpatient (CAMEO) [5]: The form is designed to observe and evaluate the performance of residents when they are functioning independently in making initial decisions about patient assessment and management and conduct of the patient encounter. The form has a total of six categories, each marked on a Likert scale ranging from 1 to 5. Furthermore, the form also includes three categories (again rated on a Likert scale ranging from 1 to 5) for the patient to answer, e.g., ‘The resident listened to me, encouraged me to ask questions and took time to answer my questions.’
-
2.
Operative Performance Rating System (OPRS) [14]: This form consists of four parts, to rate intra-operative technical skills of the performing surgeon, i.e., case difficulty and degree of prompting, procedure-specific criteria, general criteria and overall performance. Categories from each part are once again rated on Likert scales ranging from 1 to 5. For this module, the OPRS for laparoscopic cholecystectomy was used.
-
3.
Mini Clinical Evaluation Exercise (Mini-CEX) [15]: This is a direct observation tool for clinical evaluation of trainees and comprises seven categories; this time rated on a Likert scales from 1 through to 9. This scale was utilized for measurement of resident performance during the postoperative encounters.
Faculty rated the performance of residents at each stage of the pathway through live video review, utilizing the appropriate scales. Residents also performed self-rating of their own performance after each encounter. SPs were asked to rate resident performance during the pre- and postoperative encounters, through use of the CAMEO and Mini-CEX scales, respectively.
Evaluation of the module
The module was evaluated through a confidence questionnaire and a module evaluation form. The intention was not only to evaluate individual resident performance and perception of the module, but also to determine overall quality of the educational activity.
-
1.
Confidence questionnaire—prior to commencement of the module, i.e., on the first morning, residents were asked to complete a paper-based questionnaire detailing their confidence with various aspects of managing patients with biliary disease, encompassing pre-, intra- and postoperative situations. This questionnaire was again completed at the end of the 3-day module.
-
2.
Module evaluation form—at completion of the module, residents were requested to rate (on a Likert scale of 1–5) the educational activity as a whole, each individual session and specific aspects of the session, e.g., faculty engagement and quality of materials used
Implementation of the simulation pathway curriculum for biliary disease
The implementation of the simulation pathway curriculum describes the learners, faculty educators, facilities required, module organization and costs incurred. In order for the simulation curriculum to be employed with minimal disruption to clinical activities, this was also a consideration of the implementation plan.
Setting
The curriculum was to be wholly delivered within the Penn Medicine Clinical Simulation Center [16]. This is a 22,000 square foot facility incorporating auditoria, conference and breakout rooms, skills training rooms, immersive operating rooms, simulated ward and simulated clinic rooms. Synthetic, cadaveric animal and virtual reality platforms are available for use, together with whole patient mannequins. The center has a technologically advanced audiovisual system which enables recording of synchronized audio and visual feeds from anywhere within the simulation center, onto a central system, which is then available through the intranet from any health system computer. Specifically for the pathway scenarios, this system enabled a faculty surgeon to be placed into a single viewing room, and concurrently watch three video screens, each one displaying audiovisual feeds from the pre-, intra- or postoperative room.
Clinical material for the module
In order to provide a standardized, up-to-date and reproducible educational experience, the decision was made to utilize teaching material which has been made available through learned societies and pre-defined educational programs. Thus, the majority of teaching material was derived from the SAGES, SCORE and ACS/APDS curriculum websites. This also ensured that faculty educators were able to turn up, teach and leave—without the issue of having to search through material and build their own presentations, etc.
Module organization
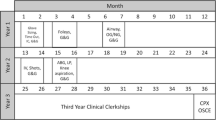
Residents would attend in groups of six for 3 days at a time. Each day lasted from 8 am until 5 pm, with a 1-h lunch break from 12 midday until 1 pm (Fig. 2). Thus, there were 8 h of simulation-based training per day. The majority of sessions involved the residents being divided into two groups of three, each led and delivered by a faculty surgeon. This high faculty/resident ratio was important to ensure that the educational experience was of the highest quality. In order to provide feedback for residents through the 3-day module, each resident underwent a full pathway curriculum on the morning of day one and again on the afternoon of day three—this enabled residents to directly compare their own performance at beginning and end of the module.
A simulation technician was also available to provide setup and takedown of each session and to ensure the necessary materials were ordered and available ahead of time. The SP resources consisted of a cadre of SP actors, two SP specialists and the director of the SP program.
It was imperative that the learners were free of clinical activities during the sessions, in order to focus upon their educational enrichment. This was achieved through two aspects: firstly, the simulation center is approximately 1.5 miles in distance from the main hospital, and thus, residents were physically not able to cover their clinical workload while at the simulation center. Secondly, residents were only pulled from clinical services where there was an additional junior resident as well as physician assistants. This would prevent overload of the rest of the clinical team, and potential patient safety issues.
Resident learners
The curriculum was focused upon knowledge, skills and attitudes required of junior surgical residents with respect to biliary disease, primarily postgraduate year (PGY) levels 1 and 2. All learners were provided with a comprehensive resident handbook at least 2 weeks prior to the start of the module. This detailed the structure of the module, the tasks to be performed and links to relevant web-based materials, e.g., the ACS/APDS curriculum.
Faculty educators
The overall responsibility for the module was undertaken by a module champion who was a content expert, and also engaged faculty colleagues to get involved. Each 4-h session was delivered by a faculty member from the Department of Surgery, who were in regular clinical practice. The faculty members had clinical expertise in biliary disease and agreed to teach of their own volition. All teaching faculties were provided with a comprehensive faculty handbook at least 2 weeks prior to the module. The handbook contained details of module organization, learning objectives, tools, techniques, simulation materials, SP scripts and links to supplemental materials (e.g., SCORE website) for each session. The handbook also contained copies of relevant scales to be used during the session for resident assessment of performance.
Costs
The implementation of this educational activity cost a total of $17,570.00 per 3-day event. This can be broken down into consumables ($5,870.00), SP actors ($3,500.00), technical staff ($1,800.00) and faculty surgeons ($6,400.00 at a rate of $200.00 per hour).
Discussion
There have been a number of mandates in recent years to engage surgical residents to undergo simulation-based training. The Residency Review Committee for Surgery insists that all residents in the United States have access to a simulation laboratory [3], and the American Board of Surgery insists that all graduating residents pass the FLS [4], and more recently the FES (or Fundamentals of Endoscopic Surgery) examinations [17]. While the tide is certainly turning toward training in the skills laboratory prior to entering the clinical domain, there remains a focus upon technical skills training. The complete surgeon must also possess medical knowledge, be a good communicator and embody systems-based practice [18].
It is our belief that the only way to train surgical residents to exemplify the ACGME competencies is to recreate the clinical environment in a simulation setting. Thus, we sought to define a disease process and focus upon clinical care pathways for that disease process. The simulation-based clinical pathway enables residents to manage a patient from the preoperative clinic or emergency room setting, through to the immersive operating room with a complete clinical team present, and then onto the follow-up clinic, recovery room or emergency room as appropriate. The pathway refocuses simulation with the patient at the center of the learning environment. In addition to the simulation-based pathway, residents undergo didactic, hands-on and SP-based learning sessions. With a focus on caring for a biliary patient through the entire care pathway (i.e., pre-, intra- and postoperatively), junior residents undergoing this curriculum develop both technical and non-technical skills in the risk-free, simulation environment, as opposed to learning on real patients.
The 3-day module is designed to provide the knowledge, skills and attitudes (i.e., KSA) building blocks for junior residents with respect to management of patients with biliary disease. While the concept is novel, the material taught is already available on the relevant websites for SCORE [8], SAGES [19] and the ACS/APDS [20] curriculum. In terms of resident assessment, this curriculum once again utilizes enduring materials from the ABS website, which are approved for use in evaluation of resident performance during clinical and operative encounters.
With regard to implementation, it is critical that residents are away from their clinical activities, and just as important, that faculty surgeons are also absolved of their clinical duties during this time. A key feature to make this work is for faculty surgeons to be able to turn up, teach and then leave, i.e., a turn-key process for the faculty to be able to teach. The setup and takedown is performed by the simulation technician, right to the level of having the PowerPoint presentation and surgical video preloaded onto the video screen in the breakout room. For the technical skills sessions, all equipment is laid out and tested beforehand, with supporting materials such as online videos also preloaded onto screens within the same room. Having trainee and faculty handbooks also maintains the level of educational quality.
While the curriculum, as designed, requires six residents in attendance for three full days, an advantage to its modular approach is the flexibility and scalability that it permits. The subtraction (or addition) of sessions within the curriculum, or modification in the timing of curriculum delivery (e.g., six half days over a 6-week period), allows this curriculum to be tailored to a wide range of residency programs. Further, the implementation of this curriculum has limited facility requirements. The clinical space, mock operating room and simulated ward are the only true requirements needed. A large, high-tech simulation center is not necessary for successful implementation.
We believe that we have presented a paradigm shift in surgical education through design, development and implementation of this novel curriculum to teach biliary disease to junior surgical residents. While organization of simulation staff, SPs, residents and faculty is necessary, we believe that these types of staff and facilities are already available in a number of simulation centers currently [21]. The issue is that the ‘dots have not been joined together,’ which prevents surgical simulation to move forward from its current focus upon technical skills training. Error in medicine is paramount, and while a large proportion of adverse events occur in the surgical domain, many of them are not solely a function of technical mishaps [22]. The training of communication skills, team-working and decision making are fundamental to enhance the quality and safety of surgical care [23]. We believe that this pathway-based curriculum refocuses simulation-based training upon the patient, and in turn, should lead to higher-quality training for our surgical residents.
References
Aggarwal R, Mytton OT, Derbrew M, Hananel D, Heydenburg M, Issenberg B, MacAulay C, Mancini ME, Morimoto T, Soper N, Ziv A, Reznick R (2010) Training and simulation for patient safety. Qual Saf Health Care 19(Suppl 2):i34–i43. doi:10.1136/qshc.2009.038562
Scott DJ, Dunnington GL (2008) The new ACS/APDS Skills Curriculum: moving the learning curve out of the operating room. J Gastrointest Surg 12(2):213–221. doi:10.1007/s11605-007-0357-y
ACGME Program Requirements for Graduate Medical Education in General Surgery. http://www.acgme.org/acgmeweb/Portals/0/PFAssets/ProgramRequirements/440_general_surgery_01012008_07012012.pdf
Peters JH, Fried GM, Swanstrom LL, Soper NJ, Sillin LF, Schirmer B, Hoffman K, Committee SF (2004) Development and validation of a comprehensive program of education and assessment of the basic fundamentals of laparoscopic surgery. Surgery 135:21–27. doi:10.1016/S0039-6060(03)00156-9
General Surgery Resident Performance Assessments. http://www.absurgery.org/default.jsp?certgsqe_resassess
Aggarwal R, Darzi A (2006) Technical-skills training in the 21st century. N Engl J Med 355(25):2695–2696. doi:10.1056/NEJMe068179
Nasca TJ, Philibert I, Brigham T, Flynn TC (2012) The next GME accreditation system–rationale and benefits. N Engl J Med 366(11):1051–1056. doi:10.1056/NEJMsr1200117
SCORE|General Surgery Resident Curriculum Portal
Aggarwal R, Undre S, Moorthy K, Vincent C, Darzi A (2004) The simulated operating theatre: comprehensive training for surgical teams. Qual Saf Health Care 13(Suppl 1):i27–i32. doi:10.1136/qhc.13.suppl_1.i27
Pucher PH, Aggarwal R, Srisatkunam T, Darzi A (2014) Validation of the simulated ward environment for assessment of ward-based surgical care. Ann Surg 259(2):215–221. doi:10.1097/SLA.0b013e318288e1d4
Aggarwal R, Ward J, Balasundaram I, Sains P, Athanasiou T, Darzi A (2007) Proving the effectiveness of virtual reality simulation for training in laparoscopic surgery. Ann Surg 246(5):771–779. doi:10.1097/SLA.0b013e3180f61b09
Aggarwal R, Grantcharov TP, Eriksen JR, Blirup D, Kristiansen VB, Funch-Jensen P, Darzi A (2006) An evidence-based virtual reality training program for novice laparoscopic surgeons. Ann Surg 244(2):310–314. doi:10.1097/01.sla.0000218094.92650.44
Aggarwal R, Crochet P, Dias A, Misra A, Ziprin P, Darzi A (2009) Development of a virtual reality training curriculum for laparoscopic cholecystectomy. Br J Surg 96(9):1086–1093. doi:10.1002/bjs.6679
Larson JL, Williams RG, Ketchum J, Boehler ML, Dunnington GL (2005) Feasibility, reliability and validity of an operative performance rating system for evaluating surgery residents. Surgery 138(4):640–647; discussion 647–649. doi:10.1016/j.surg.2005.07.017
Norcini JJ, Blank LL, Duffy FD, Fortna GS (2003) The mini-CEX: a method for assessing clinical skills. Ann Intern Med 138(6):476–481
Williams NN, Mittal MK, Dumon KR, Matika G, Pray LA, Resnick AS, Morris JB (2011) Penn medicine clinical simulation center. J Surg Educ 68(1):83–86. doi:10.1016/j.jsurg.2010.05.028
Vassiliou MC, Dunkin BJ, Fried GM, Mellinger JD, Trus T, Kaneva P, Lyons C, Korndorffer JR Jr, Ujiki M, Velanovich V, Kochman ML, Tsuda S, Martinez J, Scott DJ, Korus G, Park A, Marks JM (2014) Fundamentals of endoscopic surgery: creation and validation of the hands-on test. Surg Endosc 28(3):704–711. doi:10.1007/s00464-013-3298-4
Mery CM, Greenberg JA, Patel A, Jaik NP (2008) Teaching and assessing the ACGME competencies in surgical residency. Bull Am Coll Surg 93(7):39–47
Curriculum Outline for Resident Education—A SAGES Guideline. http://www.sages.org/publications/guidelines/curriculum-outline-for-resident-education/
Surgical Skills Curriculum|American College of Surgeons. http://www.facs.org/education/surgicalskills.html
Sachdeva AK (2010) Establishment of American College of Surgeons-accredited Education Institutes: the dawn of a new era in surgical education and training. J Surg Educ 67(4):249–250. doi:10.1016/j.jsurg.2010.07.014
Gawande AA, Thomas EJ, Zinner MJ, Brennan TA (1999) The incidence and nature of surgical adverse events in Colorado and Utah in 1992. Surgery 126(1):66–75. doi:10.1067/msy.1999.98664
Newton RC, Mytton OT, Aggarwal R, Runciman WB, Free M, Fahlgren B, Akiyama M, Farlow B, Yaron S, Locke G, Whittaker S (2010) Making existing technology safer in healthcare. Qual Saf Health Care 19(Suppl 2):i15–i24. doi:10.1136/qshc.2009.038539
Disclosures
Joseph Buchholz, Charles Vollmer, Kiyoyuki Miyasaka, Denise LaMarra and Rajesh Aggarwal have no conflict of interest or financial ties to disclose.
Author information
Authors and Affiliations
Corresponding author
Additional information
Presented at the SAGES 2014 Annual Meeting, April 2–5, 2014, Salt Lake City, Utah.
Rights and permissions
About this article
Cite this article
Buchholz, J., Vollmer, C.M., Miyasaka, K.W. et al. Design, development and implementation of a surgical simulation pathway curriculum for biliary disease. Surg Endosc 29, 68–76 (2015). https://doi.org/10.1007/s00464-014-3661-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00464-014-3661-0