Abstract
Given the current healthcare environment, optimization of patient outcomes and maximization of limited financial resources are prerequisites for the adoption of any surgical procedure. Laparoscopic common bile duct exploration (LCBDE) is an example of a safe, cost-effective strategy for managing patients who present with choledocholithiasis. However, despite the currently available evidence highlighting the clinical value of LCBDE, utilization has continued to decline, while the use of endoscopic retrograde cholangiopancreatography (ERCP) continues to increase. Commonly cited reasons for this trend include the advanced technical demands of the LCBDE procedure in addition to a lack of exposure to the procedure during surgical training. In the current era of graduate medical education (GME), restrictions on resident work hours have limited the amount of time that resident physicians can spend directly involved in patient care activities. In the field of surgical education, the practical consequence of this development is reduced time spent in the operating room under the guidance of a supervising surgeon, which has traditionally formed the foundation of surgical training. The emergence of simulation-based mastery learning (SBML) has provided surgical educators with a strategy for providing trainees with exposure to certain procedures prior to implementation in the clinical setting or as a way to teach techniques that are rarely encountered. This chapter describes the development of a low-cost simulator for teaching surgical residents the necessary knowledge and skills to perform LCBDE in the appropriately selected patient. Included is a brief discussion of the impact of implementing a simulation-based mastery learning curriculum for LCBDE with a focus on clinical outcomes for patients presenting with choledocholithiasis.
Access provided by CONRICYT-eBooks. Download chapter PDF
Similar content being viewed by others
Keywords
- Graduate medical education
- Laparoscopic common bile duct exploration
- Surgical education
- Competency-based education
- Mastery learning
- Simulation-based education
- Simulation-based mastery learning
- Translational science
Introduction
Surgical education in the United States has long been influenced by the ideology of William Halsted, MD, FACS, and William Osler, MD, in which the role of graduated responsibility under the close supervision of an experienced surgeon was paramount [1, 2]. This “apprenticeship model” would go on to form the foundation of surgical training for years to come. Surgeons who trained during this era were often exposed to a broad range of surgical disease and pathology since there were no viable alternatives at the time. This allowed them to become experts in the management of a large number of conditions. A number of factors in the current era of surgery and graduate medical education (GME) have contributed to limit the utility of apprenticeship education. Numerous technological and educational advancements have resulted in the development and proliferation of alternative treatments that have lessened the dependence on surgical intervention to treat human disease. In addition, restrictions placed on resident training in addition to the expansion of specialized postgraduate fellowships have served to limit exposure to a wide range of procedures for general surgical trainees in the modern era when compared to their predecessors [3].
Numerous examples of this evolution can be found in the field of hepatopancreatobiliary (HPB) surgery , which has traditionally fallen under the scope of general surgery. Various developments have served to fundamentally alter the approach to managing hepatobiliary pathology in a way that has had profound implications for the training of general surgeons. Management of biliary disease in particular is one area that has seen a major evolution in the surgical approach to managing these conditions. For example, the introduction of the laparoscopic cholecystectomy caused an almost overnight revolution in the management of gallbladder disease, resulting in a precipitous drop in the number of open cholecystectomies being performed by general surgeons [4]. While this development had obvious benefits for patients in the form of reduced postoperative pain and a shorter length of stay, the near universal incorporation of the technique had a number of implications for the practice of general surgery, and for the training of general surgery residents in particular. While the widespread use of laparoscopic cholecystectomy encouraged surgeons to become comfortable with general laparoscopic techniques, it also served to significantly limit their exposure to the principles of open hepatobiliary surgery.
The approach to the management of common bile duct stones provides another example of how surgical practice and education has been profoundly influenced by the introduction and widespread adoption of an alternative treatment. The first use of endoscopic retrograde cholangiopancreatography (ERCP) for the management of biliary disease occurred in the 1970s [5]. While ERCP allows patients to avoid surgery in many cases, the procedure is not without risk. Post-procedural pancreatitis and hemorrhage are two feared complications of ERCP that can result in significant morbidity and mortality. Despite these considerations, ERCP rapidly replaced common duct exploration (CDE) as a primary treatment for choledocholithiasis. A 2005 study analyzing the effect of decreased utilization of surgical CDE on complication rates estimated that approximately 47,000 CDEs were performed per year in the late 1970s prior to the widespread introduction of ERCP. This number would fall to less than 10,000 cases per year by 2001 and has continued to decrease [6, 7]. While it is tempting to accept that surgical exploration of the common bile duct (CBD) has been rendered obsolete by ERCP, it should be remembered that the use of LCBDE offers distinct advantages over endoscopy. A single-stage operation with LCBDE at the time of laparoscopic cholecystectomy (LC) obviates the need for patients to undergo a two-stage procedure with ERCP either before or after LC, thereby avoiding a second anesthetic in addition to adding the previously described risks of ERCP. Multiple studies have demonstrated that LCBDE is equivalent to ERCP for achieving clearance of ductal stones [8, 9].
The declining utilization of LCBDE has serious implications for training of general surgeons (Fig. 16.1). A recent study examining the operative case logs of graduating chief general surgery residents showed that residents only participated in an average of 1.7 open CDEs and 0.7 LCBDEs over the course of their training [10]. These findings have raised concerns that the next generation of general surgeons is receiving inadequate exposure to the surgical management of biliary disease. While ERCP provides an attractive alternative for patients hoping to avoid surgery, surgeons need to be proficient in the general principles of CDE as surgical intervention is now generally the last resort for patients with choledocholithiasis not resolved after endoscopic intervention.
Utilization trends of surgical common bile duct exploration from 1998 to 2013. Reprinted with permission from Wandling et al. [7]
Simulation and Laparoscopic Common Bile Duct Exploration
One of the commonly cited reasons for the lack of utilization of the LCBDE procedure is that it requires advanced laparoscopic skills in order to successfully obtain clearance of the CBD. While it is true that a transcholedochal exploration requires the surgeon to be familiar with advanced laparoscopic maneuvers including intracorporeal suturing in order to repair the choledochotomy, the transcystic approach can be safely attempted by any surgeon with basic laparoscopic training. There are a series of operative steps that must be followed in order to increase the likelihood of successfully clearing any CBD obstruction via the laparoscopic approach. However, as is the case with any procedure that is done infrequently, many surgeons are unfamiliar with the procedural steps of LCBDE. Most also lack knowledge regarding strategies that can be employed when dealing with a variety of intraoperative scenarios, including obtaining and maintaining guidewire access, accessing the CBD with the choledochoscope, manipulation of the choledochoscope during stone retrieval, and appropriate management of the cystic duct stump (see Video 16.1). Surgical simulation has emerged as a viable option for training of novice physicians in a multitude of procedures and is not limited only to those in procedural fields. The scope of these simulators ranges widely, including various low-cost inanimate task trainers aimed primarily at practicing a single skill, up to live animal models that afford trainees the opportunity to practice skills in an environment that closely approximates that found in the operating room—but these models are limited by issues of cost and ethical concerns.
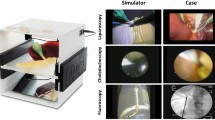
In an attempt to improve upon previous LCBDE simulation models, Santos and colleagues at Northwestern University Feinberg School of Medicine develope d a low-cost LCBDE simulation program aimed at teaching learners a stepwise approach to performance of an LCBDE (Fig. 16.2) [11]. The development of the simulator began by defining a comprehensive algorithm covering the cognitive and technical considerations necessary for successfully performing an LCBDE (Fig. 16.3).
Algorithm outlining key cognitive and technical steps of LCBDE. Reprinted with permission from Santos et al. [11]
The physical simulator was then developed and incorporated multiple modalities utilized during a clinical LCBDE case, including a laparoscopic image utilizing the static camera of a Fundamentals of Laparoscopic Surgery™ trainer box, a simulated fluoroscopic view by using a second camera and mirror in addition to the endoscopic image provided by a flexible choledochoscope for retrieving the CBD “stone” (Fig. 16.4).
LCBDE simulated views. (a) Laparoscopic view demonstrating liver (black), gallbladder (green), cystic duct, and common bile duct (CBD). (b) Fluoroscopic view demonstrating distal filling defect (black) after establishment of guidewire access. (c) Endoscopic view demonstrating CBD stone (black) trapped in endoscopic basket retrieval device
Performance on a simulated task is improved when learners are provided with targeted assessment and feedback at the conclusion of the training session. Therefore, in addition to development of the multimodality LCBDE simulator, procedure-specific rating scales based on the objective structured assessment of technical skills (OSATS) principles were developed for the purpose of evaluating a participant’s performance on the simulator. Rather than u sing a generic rating scale based solely on technical skill, the rating scale was based on the previously developed algorithm and assessed learners on their cognitive understanding of the LCBDE procedure in addition to their technical skill. Examples of these components included assessing the understanding of the available adjuncts available for clearing the CBD prior to embarking on a laparoscopic exploration, in addition to managing the cystic duct stump at the conclusion of the procedure. Learners were also asked to provide justification for their choice of operative approach, as the simulator was originally designed to permit either a transcholedochal or a transcystic laparoscopic exploration. Given the complex nature of the decision-making process necessary for performing LCBDE, utilizing this approach allows raters to better assess a participant’s overall understanding of the various considerations that must be accounted for during the performance of an LCBDE procedure.
Mastery Learning
While simulation certainly provides advantages for learners, isolated performance of a simulated procedure is not adequate preparation for optimal performance in a real-world situation. Rather, simulation should function as one part of a comprehensive, goal-directed curriculum designed to provide learners with a global understanding of the subject material. Mastery learning (ML ) is an educational strategy that has undergone a resurgence, particularly in the field of medical education and simulation. ML is founded on the principle that any motivated learner has the capacity to reach a predefined competency level, otherwise known as the “mastery” standard, provided they are given the necessary time and resources in order to attain a particular educational goal. This approach is in contrast to the contemporary model, whereby learners are given a discrete unit of time in which to accomplish the educational task. This has traditionally resulted in variable educational outcomes given that a proportion of learners will be unable to achieve the defined educational standard within the allotted time. In contrast, mastery learning is focused on universal achievement at the expense of variable learni ng time and requires a paradigm shift in medical education, and particularly surgical education, given the time constraints placed on residents. The concept of mastery learning has traditionally been broken down into seven core features (Table 16.1) [12].
One of the key tenets of ML is the concept of “deliberate practice” [13]. Deliberate practice describes a process of immersive, goal-directed practice and involves targeted and immediate feedback for the learner. The timely provision of this feedback provides learners with an opportunity to quickly correct mistakes and increases the likelihood of reaching the defined mastery standard within the allotted time. This process fosters a high level of achievement among learners while simultaneously reducing variation in educational outcomes, the keystone of the mast ery learning approach. ML concepts are widely applicable and have found fertile ground in the field of medical simulation [14,15,16,17].
Simulation-based mastery learning (SBML) has emerged as a unique opportunity in the field of surgical education as a strategy to address training deficiencies while promoting graduated responsibility among surgical residents. There are a variety of applications for well-designed SBML curricula. SBML can be used to provide novices with exposure to various surgical techniques prior to applying those techniques in the operating room. Another benefit of SBML is the ability to provide residents with exposure to surgical procedures not commonly encountered during the normal course of their clinical training. As described earlier, one of the commonly cited reasons for the low utilization of LCBDE is lack of exposure to the procedure during clinical training.
Using the previously described simulator, Teitelbaum and colleagues designed an SBML educational curriculum aimed at teaching senior surgical residents the essential steps for performing both a transcystic and a transcholedochal LCBDE [18]. The curriculum consisted of a pretest, where resident surgeons were asked to perform a simulated LCBDE without any preparation. They were then provided with didactic materials and given opportunities for deliberate practice followed by a posttest assessment on the simulator. The minimum passing score, or “mastery standard,” was previously defined by two senior surgeons with prior LCBDE experience utilizing the previously described OSATS assessment tool. The SBML curriculum was then evaluated am ong a group of ten senior surgical residents with no prior LCBDE experience. None of the original ten residents who participated in the study achieved the mastery standard during the initial pretest. However, all residents were able to achieve the mastery standard on their posttest after a period of deliberate practice using the LCBDE simulator. In addition to achieving the mastery standard, pre- and post-surveys completed by the participating residents demonstrated a significant improvement in their perceived ability to perform an LCBDE independently. Importantly, steps were taken to include operating room (OR) nurses and staff in the training sessions. This served two primary functions: It improved OR staff awareness of the equipment needed when the decision is made to proceed to LCBDE and also acquainted them with the key procedural steps. Senior residents rotating on the minimally invasive surgery service are now required to demonstrate successful completion of the LCBDE mastery curriculum as a core requirement of the rotation.
Preliminary work examining the clinical impact of the LCBDE curriculum demonstrates a number of trends that have significant implications, both for patients presenting with choledocholithiasis and for the training of surgical residents. Fi rst, an analysis of LCBDE utilization before and after implementation of the SBML curriculum demonstrated a statistically significant increase in the clinical use of LCBDE, both in terms of the absolute number of cases being performed per year and the overall percentage of patients presenting with choledocholithiasis who underwent single-stage management with LC/LCBDE compared to two-stage management with LC + ERCP. In addition to the overall increase in the use of LCBDE, the analysis demonstrated that the majority of cases done after curriculum implementation were performed by surgical faculty who had no prior LCBDE experience with the assistance of a resident who had successfully completed the LCBDE curriculum. This is an example of an educational intervention aimed solely at residents that resulted in a change in the pattern of surgical practice within an institution and represents a profound deviation from the traditional structure of surgical education. Additionally, when compared to ERCP + LC, the use of LCBDE among similarly matched patients resulted in significant cost savings and a reduced length of stay. These unpublished results (in press) provide an example of the potential benefits of implementing a targeted intervention designed to address a deficiency in current surgical practice and suggest that a well-designed SBML curriculum can effectively supplement the traditional apprenticeship model for the benefit of trainee surgeons while also resulting in significantly improv ed patient-level outcomes.
Conclusion
The use of LCBDE remains a clearly underutilized modality for managing patients who present with uncomplicated choledocholithiasis, despite continued evidence of its efficacy and cost-effectiveness when compared to the use of ERCP. While there is clearly a role for endoscopic management of these patients, it must be remembered that the procedure is not without its attendant risks, some of which can result in major morbidity or mortality. In addition, the use of single-stage LCBDE and laparoscopic cholecystectomy has obvious benefits to patients by avoiding multiple procedures, limiting anesthetic interventions, and shortening hospital stay. We believe that LCBDE should be the first choice for appropriately selected patients who present with choledocholithiasis.
Given the current clinical environment where ERCP is often the first step in management, opportunities for surgical residents to gain experience with the techniques necessary to perform a safe and therapeutic LCBDE are limited. Performing LCBDE does require surgeons to follow a series of cognitive and technical steps that will increase the likelihood of success and is not necessarily intuitive to those unfamiliar with the procedure. In an attempt to address the decline of LCBDE in surgical training and clinical use, researchers at Northwestern University designed, built, and evaluated a low-cost, multimodality LCBDE simulator and developed an SBML curriculum aimed at teaching novices the necessary skills to perform the procedure. Analysis of utilization trends and clinical outcomes demonstrated a significant increase in the use of LCBDE in addition to significant decreases in hospital length of stay and cost for patients who underwent LCBDE after implementation of the curriculum.
The success of this intervention represents an example of translational science in action, namely, a comprehensive SBML program designed to address a specific clinical deficiency in surgical training resulted in clinically significant high-level outcomes in the form of reduced cost, length of stay, and a high return of investment for the home institution. SBML will continue to serve as a powerful tool for surgical educators as they strive to prepare the next generation of surgeons for practice in an era of increasing technological advances and evolving patient care management strategies.
References
Halsted WS. The training of the surgeon. Bull Johns Hopkins Hosp. 1904;15(162):267–75.
Osler W. The hospital as a college. In: Osler W, editor. Aequanimitas. Philadelphia: P. Blakiston’s Son & Co.; [1903] 1932.
Bell RH Jr, Biester TW, Tabuenca A, Rhodes RS, Cofer JB, Britt LD, Lewis FR Jr. Operative experience of residents in U.S. general surgery programs: a gap between expectation and experience. Ann Surg. 2009;249:719–24.
Begos DG, Modlin IM. Laparoscopic cholecystectomy: from gimmick to gold standard. J Clin Gastroenterol. 1994;19(4):325–30.
Katon RM, Lee TG, Parent JA, Bilbao MK, Smith FW. Endoscopic retrograde cholangiopancreatography (ERCP). Experience with 100 cases. Am J Dig Dis. 1974;19(4):295–306.
Livingston EH, Rege RV. Technical complications are rising as common duct exploration is becoming rare. J Am Coll Surg. 2005;201(3):426–33.
Wandling MW, Hungness ES, Pavey ES, Stulberg JJ, Schwab B, Yang AD, et al. Nationwide assessment of trends in choledocholithiasis management in the United States from 1998 to 2013. JAMA Surg. 2016;151(12):1125–30.
Dasari BV, Tan CJ, Gurusamy KS, Martin DJ, Kirk G, McKie L, et al. Surgical versus endoscopic treatment of bile duct stones. Cochrane Database Syst Rev. 2013;12:CD003327.
Rogers SJ, Cello JP, Horn JK, Siperstein AE, Schecter WP, Campbell AR, et al. Prospective randomized trial of LC+LCBDE vs ERCP/S+LC for common bile duct stone disease. Arch Surg. 2010;145(1):28–33.
Helling TS, Khandelwal A. The challenges of resident training in complex hepatic, pancreatic, and biliary procedures. J Gastrointest Surg. 2008;12(1):153–8.
Santos BF, Reif TJ, Soper NJ, Nagle AP, Rooney DM, Hungness ES. Development and evaluation of a laparoscopic common bile duct exploration simulator and procedural rating scale. Surg Endosc. 2012;26(9):2403–15.
McGaghie WC, Siddall VJ, Mazmanian PE, Myers J. Lessons for continuing medical education from simulation research in undergraduate and graduate medical education: effectiveness of continuing medical education: American college of chest physicians evidence-based educational guidelines. Chest. 2009;135(3, Suppl):62S–8S.
Ericsson KA, Krampe RT, Tesch-Römer C. The role of deliberate practice in the acquisition of expert performance. Psychol Rev. 1993;100:363–406.
Barsuk JH, Cohen ER, Vozenilek JA, et al. Simulation-based education with mastery learning improves paracentesis skills. J Grad Med Educ. 2012;4:23–7.
Wayne DB, Barsuk JH, O’Leary KJ, Fudala MJ, McGaghie WC. Mastery learning of thoracentesis skills by internal medicine residents using simulation technology and deliberate practice. J Hosp Med. 2008;3(1):48–54.
Barsuk JH, McGaghie WC, Cohen ER, O’Leary KJ, Wayne DB. Simulation-based mastery learning reduces complications during central venous catheter insertion in a medical intensive care unit. Crit Care Med. 2009;37:2697–701.
Zendejas B, Cook DA, Hernández-Irizarry R, Huebner M, Farley DR. Mastery learning simulation-based curriculum for laparoscopic TEP inguinal hernia repair. J Surg Educ. 2012;69:208–14.
Teitelbaum EN, Soper NJ, Santos BF, Rooney DM, Patel P, Nagle AP, et al. A simulator-based resident curriculum for laparoscopic common bile duct exploration. Surgery. 2014;156(4):880–7.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Electronic Supplementary Material
The video demonstrates the key steps for transcystic common bile duct exploration in both a real case and in the simulator. Steps include (1) cholangiogram, (2) wire access, (3) cystic duct dilation, (4) choledochoscope insertion and maneuvering, (5) stone capture, (6) stone extraction, (7) completion cholangiogram, and (8) cystic duct ligation (MP4 212302 kb)
Rights and permissions
Copyright information
© 2018 Springer International Publishing AG, part of Springer Nature
About this chapter
Cite this chapter
Schwab, B., Campagna, R.A., Hungness, E.S. (2018). Training in Laparoscopic Common Bile Duct Exploration: Role of Simulation and Its Impact on Clinical Outcomes. In: Santos, B., Soper, N. (eds) Choledocholithiasis . Springer, Cham. https://doi.org/10.1007/978-3-319-74503-9_16
Download citation
DOI: https://doi.org/10.1007/978-3-319-74503-9_16
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-319-74502-2
Online ISBN: 978-3-319-74503-9
eBook Packages: MedicineMedicine (R0)