Abstract
Background
The aim of this study was to evaluate the effect and cosmetic results of endoscopic thyroidectomy (ETE) via the areola approach for patients with thyroid diseases.
Methods
A total of 1,250 patients with thyroid diseases underwent ETE via the areola approach between April 2005 and January 2011. Of these, 898 were benign goiters, 260 were Graves’ disease, 28 were secondary hyperthyroidism, and 64 were papillary carcinomas.
Results
The surgery was successfully completed in 1,249 cases, and 1 case was converted to open surgery. The mean operation time, estimated blood loss, and hospital stay after surgery for patients with a goiter, hyperthyroidism, and papillary carcinoma were 94.4 min, 15.2 ml, 5.0 days, 97.9 min, 16.1 ml, 5.5 days, and 134.3 min, 18.6 ml, 6.4 days, respectively. Complications included 4 cases of postoperative bleeding, 1 case of transection of the recurrent laryngeal nerve (RLN) on one side, 7 cases of temporary RLN injury, 34 cases of transient hypocalcemia, 5 cases of skin bruising on the chest wall, and 1 case of subcutaneous infection in the neck. At 4.6-year (2.5–8 years) follow-up of 1,185 (94.8 %) patients, 3 patients with Graves’ disease had recurrence of hyperthyroidism, and 4 patients with nodular goiter had recurrence of small nodules. Four patients had discomfort on swallowing, 4 patients had an abnormal sensation of skin traction on the neck and the chest, and 1 patient with scar diathesis had mild scar hyperplasia. A total of 876 patients were satisfied, 4 equivocal, and 0 unsatisfied with the cosmetic results.
Conclusion
ETE via the areola approach for patients with benign goiters, Graves’ disease, secondary hyperthyroidism, and papillary carcinomas without metastasis to lateral cervical lymph nodes is an effective and safe procedure with excellent cosmetic results.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
In 1996, Gagner [1] performed and reported the first endoscopic parathyroid surgery. Since then, several approaches of endoscopic thyroidectomy (ETE) have been introduced, including the cervical approach [2], the small anterior cervical incisions approach [3], the subclavian approach [4], the axillary approach [5], the areola and cleavage approach [6], and so on. However, the small surgical scar left on or near the neck is not acceptable for patients with high expectation for cosmetic results, especially Asian patients with particularly pronounced scars. With ETE through the axillary approach, resection of the contralateral gland is difficult, which limits its application.
Our hospital has treated various benign and malignant thyroid diseases with ETE via an areola and cleavage approach since 2002 and achieved satisfactory cosmetic result. Then, we moved the surgical incision of the observation port outward and applied ETE via an areola and chest wall approach to improve the cosmetic results. However, after years of practice, we found that some of the patients who received these two types of surgeries showed scar hyperplasia due to significant skin tension in front of or close to the sternum [7]. In addition, the subcutaneous tissue in this place is tight, and the samples collected here need to be fully broken up, which increases the difficulty of the pathology examination. Therefore, we took advantage of the fact that the position of the areola is concealed, that female breasts have mobility that subcutaneous tissues in the breast are relatively loose and established ETE via the areola approach in April 2005.
We have performed 1,250 cases using this approach between April 2005 and January 2011, and have summarized them below.
Materials and methods
Patients
A total of 1,250 patients with thyroid diseases who had high expectation of cosmetic results were included. The group of patients consisted of including 256 males and 994 females. The mean age of the patients was 31.6 (14–56 years). The following inclusion criteria were used: thyroid solid or cystic mass (maximum diameter not greater than 7 cm), secondary hyperthyroidism, patients with Graves’ disease who were not tolerant to long-term medication and did not want to receive 131I therapy, thyroid goiters that were suspected to be micro-carcinoma, and lymphocytic thyroiditis that was suspected to be malignant (no metastasis to lateral cervical lymph node or distant metastasis, diameter less than 2 cm, age <45 years). The exclusion criteria were as follows: poor general condition that could not tolerate general anesthesia, severe coagulopathies, tumor diameter greater than 7 cm, tumors extending beyond the sternum for more than 3 cm, thyroid cancer with metastasis to lateral cervical lymph nodes or distant metastasis, and postoperative recurrence with large and fixed lumps. The included patients voluntarily chose surgical treatment because of poor esthetic appearance, local sensation of pressure, psychological fear of tumors, intolerance to long-term medication for hyperthyroidism, suspected cancer, and other reasons. The surgical options were discussed with the patients before surgery, and the patients chose ETE via the areola approach.
Preoperative management
B-ultrasound and CT scans of the neck were performed before the surgery and fine needle aspiration (FNA) was also performed in some cases. In addition, vocal cord movement was examined with laryngoscopy before and after the surgery. Patients also underwent blood tests for thyroid function, IPTH level, serum Ca2+ level, and coagulation function. Patients with hyperthyroidism took antithyroid drugs to control symptoms of hyperthyroidism and then received an oral compound iodine solution for 3 weeks.
Surgical procedure
Working space
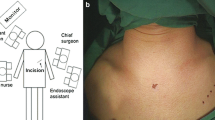
After endotracheal intubation under general anesthesia, the patient was placed in a supine position with all limbs spread outward. Cushions were used to lift the shoulders so that the neck was slightly extended. The patient was prepped and draped in the usual sterile fashion. The surgeon stood between the patient’s legs, and the assistants stood on both sides of the patient’s neck. The “inflation liquid” that consisted of 1 mg adrenaline mixed with 500 ml saline was injected subcutaneously into the medial edge of the right areola. A 12-mm curved incision was made based on 2–4 points along the edge of the areola, and approximately 50–100 ml “inflation liquid” was injected into the subcutaneous deep fascia below the suprasternal notch with a water injector. A subcutaneous separation stick was used to separate the skin through the incision resulting in fanning out from the deep layer of the superficial fascia toward the suprasternal fossa. After the subcutaneous tunnel was formed, excess liquid was suctioned out. A trocar with an inner diameter of 10 mm was placed and a 10 mm, 30° laparoscope was used. CO2 was maintained at a constant pressure of 6 mmHg. At the 11 o’clock positions on the left and right edges of the areola, a 5-mm trocar was placed, which served as the main and auxiliary operation ports (Fig. 1). An ultrasonic scalpel and a pair of toothless graspers were placed in the main and auxiliary operation ports, respectively. The ultrasonic scalpel was used to separate subcutaneous loose connective tissues superiorly to the upper edge of the cricoid cartilage and laterally to the midline of the sternocleidomastoid. The separation was between the superficial layer of the sternohyoid muscles and the deep layer of the platysma muscle.
Thyroidectomy
The ultrasonic scalpel was used to open the midline of the infrahyoid muscles. After the infrahyoid muscles and the thyroid capsule were separated, a suture was placed into the working space, and the tail of the suture was left outside the operation space. Then, we sutured the muscle layers beneath the hyoid, and the head of the suture was kept outside the working space. Thus, the muscles could be suspended to help expose the thyroid gland by pulling the sutures outside the working space. First, the isthmus was separated from the trachea and cut off using the ultrasonic scalpel. The lower pole of the thyroid structure was exposed through blunt dissection with endoscopic forceps, and the inferior thyroid arteries and veins were resected. The lobe was then retracted superiorly and medially, and the middle thyroid vein and Berry’s ligament were cut using the ultrasonic scalpel. The recurrent laryngeal nerve (RLN) was partially exposed to reveal its position and course by blunt dissection. Subsequently, the lobe was retracted inferiorly to expose the superior thyroid arteries, which were then resected using the ultrasonic scalpel. Lastly, the lobe was resected, and the contralateral lobe was resected in a similar manner. All of the resected tissues were placed in a specimen bag, taken out through the observation port, and sent for intraoperative frozen pathology.
Graves’ disease
Bilateral subtotal resections (4–6 g gland retained) or Dunhill’s operation (lobectomy and contralateral subtotal resection, 2–3 g gland retained) were performed for patients with Graves’ disease. Total resection was performed for the patients who were diagnosed with Graves’ disease combined with thyroid cancers by intraoperative frozen pathology. Fractional resection was performed for patients with a huge thyroid gland.
Benign goiter
Unilateral subtotal, near-total (less than 0.5 g gland retained), or total resection was performed for patients with a unilateral benign goiter. Bilateral subtotal, near-total, or total resection was performed for patients with bilateral benign goiters. The thyroid gland can be suspended by a suture if en bloc resection is difficult to achieve during the operation. The method was similar to that used to suspend the muscle layers beneath the hyoid, the difference was that we sutured the thyroid gland with an “8” shape knot. Thus, the thyroid gland could be suspended by pulling the suture outside of the working space to help expose it. The anterior cervical muscles were severed when the lump was huge (about 7 cm in diameter).
PTC (papillary thyroid carcinoma)
Total resection was performed for patients with a diagnosis of PTC that was confirmed by intraoperative frozen section. Then, the working space was expanded to the lateral edge of the carotid sheath on the ipsilateral side and to the level of the hyoid bone superiorly. The RLN was fully exposed when lymph node clearance was carried out in the central zone, including the prelaryngeal, pretracheal, and paratracheal areas. The lymph nodes and fat tissues were pulled upward to reach the thymus when lymph node resection was carried out at the lower pole and pretracheal. Parathyroid glands and their blood vessels were retained in situ as much as possible during the surgery. When the resected tissues were suspected to be parathyroid glands, a small piece of the tissue was routinely collected and sent for intraoperative frozen biopsy. The remaining tissues were soaked in saline. The tissues were cut into small pieces that were approximately 1–2 mm in size and then endoscopically transplanted into the sternocleidomastoid in once they were confirmed as parathyroid glands. The resected lymph nodes in the central zone were sent for intraoperative frozen pathology. The surgery was completed if there were no metastases of thyroid cancer in the lymph nodes. Endoscopic lymphadenectomy on the ipsilateral side in zones III and IV was performed if there were metastases of thyroid cancer to multiple lymph nodes.
After careful examination for surgical bleeding, absorbable sutures were used for interrupted closure of the linea alba cervicalis. A silicone drainage tube was placed in the thyroid fossa that exited through the incision at the edge of the areola and was then connected to a negative pressure drainage bottle. In some cases, the drainage tube was not placed.
Postoperative management
After the surgery, patients with hyperthyroidism were given an oral iodine preparation to prevent thyroid storm. Patients with hypocalcemia were given calcium supplements. An inhaled expectorant was used to induce sputum discharge with cough, and discutients were applied to reduce swelling of the surgical site. The drainage tube was removed when the drainage volume was less than 30 ml in 24 h. Patients with papillary carcinoma were treated postoperatively according to the guideline of the American Thyroid Association (ATA) [8–10]. A retrospective analysis on surgical time, blood loss, complications, length of hospital stay, and thyroid function was performed.
A total of 1,185 (94.8 %) patients were followed up in the outpatient clinic or by telephone for over 2 years. The remaining patients were lost to follow-up due to relocation or loss of contact. The mean duration of follow-up was 4.6 years (2.5–8 years). The physicians conducted a survey in the outpatient clinic or by telephone on the patients over a one-year period after surgery. This survey included feelings in the neck and chest, whether there was scar hyperplasia of the surgical incision, and satisfaction scores regarding the cosmetic results (0–10 points, from very dissatisfied to very satisfied).
Statistics
PASW Statistics 18 software (IBM Corp, U.S.) was used for variable analysis. χ 2-test was performed for comparison of categorical variables. The t-test was performed for comparison of measurement data. The SNK test or Tamhane’s T2 test of one-way ANOVA was performed for pairwise comparisons. Data are expressed as mean ± standard deviation.
Results
Overall outcome
The surgery was successfully completed in 1,249 cases, and 1 was converted to open surgery (due to bleeding that could not be controlled). There were 810 cases of nodular goiters, 67 cases of follicular adenoma, 30 cases of lymphocytic thyroiditis which were combined with thyroid nodules (including 21 cases of benign nodules, 9 cases of papillary carcinoma, diameters 0.3–2 cm), 260 cases of Graves’ disease (2 cases combined with papillary micro-carcinoma, diameters 0.3–0.5 cm), 28 cases of secondary hyperthyroidism, and 55 cases of papillary carcinoma (diameters 0.3–2 cm), which were confirmed by pathological examination.
The surgical outcomes of goiters, hyperthyroidism, and PTC are shown as Table 1. The mean surgical time of PTC was higher than for thyroid goiters and hyperthyroidism by SNK test (F = 65.249, P = 0.000), but there was no difference between thyroid goiters and hyperthyroidism, with a mean operation time of 94.4, 97.9, and 134.3 min, respectively. There was no difference in mean blood loss between the different groups by Tamhane’s T2 test (F = 0.746, P = 0.474), with mean blood losses of 15.2, 16.1, and 18.6 ml, respectively. There was a significant difference in mean drainage time between the groups by SNK test (F = 39.277, P = 0.000), with mean drainage times of 2.5, 2.8, and 2.7 days, respectively. In addition, there was a significant difference in mean hospital stay after surgery between the groups by Tamhane’s T2 test (F = 34.865, P = 0.000), with mean hospital stays after surgery of 5.0, 5.5, and 6.4 days, respectively.
Postoperative bleeding occurred in 2 cases of bleeding from the observation tunnel, 1 case of anterior jugular venous bleeding, and 1 case of oozing from the glandular section, which caused a hematocele in the working space within 2 h after surgery. All patients were treated successfully with endoscopic exploration. There were no cases with permanent hypocalcemia. For the patients who had transient hypocalcemia after surgery, the serum calcium and the parathyroid hormone were restored to normal levels within 3 months with intravenous or oral calcium supplements. Vocal cord paralysis was confirmed by laryngoscopy in 8 cases after surgery. The voices recovered in 7 cases on day 2 to 62 postoperative, and normal vocal cord movement was confirmed by laryngoscopy, except for 1 case, in which the RLN was transected on one side of a papillary carcinoma. There was 1 case of subcutaneous infection in the neck, which was cured successfully with drainage of the purulent material through repeated puncture and anti-inflammatory therapy. There were 4 cases of swallowing discomfort, and 4 cases of abnormal sensation of skin traction on the neck and the chest within 2 year postoperatively.
Graves’ disease
Bilateral subtotal resection (4–6 g gland retained), Dunhill’s operation (2–3 g gland retained), or bilateral total resections were performed in patients with Graves’ disease, and the surgical outcomes are shown in Table 2. There were no differences in surgical time, estimated blood loss, weight of resected gland, and complications between them (P>0.05), but number of hypothyroidism over 2 years after Dunhill’s operation was higher than bilateral subtotal resection (P = 0.000). There were 3 cases of recurrence of hyperthyroidism after bilateral subtotal resection, 2 were cured with 131I therapy and 1 was cured with endoscopic surgery.
Benign goiters
Unilateral resection (163 cases), bilateral subtotal or near-total resection (613 cases), or total resection (122 cases) was performed in patients with benign goiters, and the surgical outcomes are shown in Table 3. There was a significant difference in mean surgical time between the groups by Tamhane’s T2 test (F = 212.843, P = 0.000), with mean operation times of 65.1, 97.7, and 116.8 min, respectively. The mean blood loss of unilateral resections was lower than that of bilateral subtotal or near-total resections and total resections by Tamhane’s T2 test, but there was no difference in between bilateral subtotal or near-total resections and total resections (F = 7.918, P = 0.000), with mean blood losses of 9.9, 15.1, and 22.6 ml, respectively. Recurrences of small nodules after surgery were confirmed by B-ultrasound in 4 cases, which are still being followed up.
PTC
Total resection plus ipsilateral central lymphadenectomy was performed in patients with papillary carcinomas, and the surgical outcomes are shown in Table 4. The surgical time and estimated blood loss of total resection plus bilateral central lymphadenectomy were higher than total resection plus unilateral central lymphadenectomy (P < 0.05). There were no differences in RLN injury and transient hypocalcemia between them (P > 0.05). There were 34 cases of lymph node metastasis in the central zone, no lymph node metastasis in zones III and IV, and 48 cases of them needed postoperative 131I therapy according to the guideline of the ATA. There was no recurrence of thyroid cancer in any of the patients for over 2.5 years of follow-up.
Questionnaires
Questionnaires were distributed to 880 patients more than 2 years postoperatively. The content of the questionnaire included feelings in the neck and chest, the presence of scar hyperplasia of the surgical incision, and the satisfaction scores regarding the cosmetic results. The results showed that there were 4 patients with swallowing discomfort, 4 patients with abnormal sensation of skin traction on the neck and the chest, and 1 case with scar diathesis and mild scar hyperplasia of the surgical incision. The remaining patients did not have any scar hyperplasia of the surgical incision. Overall, 876 patients were satisfied with the cosmetic results, 4 were equivocal, and none of the patients were unsatisfied, and the mean scores of patients in their 10, 20, 30, 40, and 50 s were 9.8, 9.9, 9.6, 9.5, and 9.5, respectively (Table 5).
Discussion
Patients for this surgery
ETE via various approaches has been applied to treat various thyroid diseases in many countries. The incidence of postoperative bleeding, RLN injury, parathyroid gland injury, and other complications was low in these studies [11–16]. We could prevent these complications in our study in the case of the quantity of the case was large and the types of disease were abundant, with postoperative bleeding occurred in 0.3 %, transient hypocalcemia in 2.72 %, permanent RLN injury in 0.08 %, and temporary RLN injury in 0.56 %. We reduced the risk of conversion to open surgery by choosing appropriate patients at the beginning of the study. The first 50 patients we chose were all young women, and one of the following conditions had to be met: benign tumor with maximum diameter of ≤5 cm, primary or secondary hyperthyroidism with less than 60 g of estimated gland weight, and differentiated thyroid micro-carcinoma without metastasis to lateral cervical lymph nodes.
We chose female patients at the beginning mainly because theirs breasts have better mobility and the operation was relatively easy. Then, we were able to perform this surgery on male patients, most of the benign goiter, Graves’ disease with huge thyroid gland, and low-risk PTC without metastasis to lateral cervical lymph nodes. The maximum diameter of the resected benign tumors in this study was 7 cm and the maximum weight of the resected thyroid gland of Graves’ disease was over 150 g. However, patients with metastasis of thyroid cancer to the lateral cervical lymph nodes or to distant lymph nodes were excluded. Patients with large thyroid goiters that may not have had enough available space for the operation were also excluded. There was a patient whose thyroid gland was full of severe eggshell calcifications, which made it difficult to loosen the gland and led to uncontrollable bleeding in the lower pole, and the operation was converted to open surgery. Hence, open surgery should be chosen for cases in which preoperative assessment shows that the thyroidectomy would be difficult to complete through this surgery.
Surgical techniques and options for different thyroid diseases
Prevention of bleeding is the most important part of endoscopic surgery for Graves’ disease, because there is a risk of converting to open surgery due to the high vascularity of the thyroid gland [17]. Sasaki et al. [17] suggested that it was relatively safe to perform endoscopic surgery when the weight of thyroid glands was less than 60 g. Yamamoto et al. [16] proposed that endoscopic surgery was only suitable for treating Graves’ disease when the gland weight was less than 100 g because small gland volume can provide a better field of view during the surgery. However, most of the patients with Graves’ disease had huge thyroid gland when they accepted the surgery because of years of medical treatment. And most of them were young women with a high demand for cosmetic results, converting to open surgery might be contrary to the original intention of surgical treatment and the scar on neck might change their lives. We also had the experience of converting to open surgery due to the blood loss during ETE through an areola and chest wall approach for Graves’ disease, with the time for iodine intake before the surgery was about 2 weeks. After this, we extended the time for iodine intake to 3 weeks before the surgery to reduce bleeding during surgery and the difficulty of the operation and have obtained satisfactory results. Although we have performed fractional resections, there was almost no bleeding in the glands when it was cut off with ultrasonic scalpel. The mean blood loss in our study was approximately 25 ml, and the mean weight of the resected gland was greater than 60 g. These were significantly lower than the results in the previous literatures [17, 18]. None of the cases had to be converted to open surgery due to intraoperative bleeding or insufficient surgical space.
The current leading trend in surgical treatment of Graves’ disease is to perform total resection [19–21]. However, bilateral subtotal resection with 4–6 g of retained gland is considered to be the standard surgical treatment for Graves’ disease in Asian countries [16, 17, 22]. We adopted this procedure in the early stage of the study. However, there was still a risk of hyperthyroidism recurrence with that amount of gland retained [17, 18, 22]. Therefore, we performed Dunhill’s operation with approximately 2–3 g of gland retained on the patients who agreed to take long-term levothyroxine supplements after surgery. The risk of complication for Dunhill’s operation was not higher than that for bilateral subtotal resections (Table 2). With Dunhill’s operation, the retained gland is on one side, which can help to estimate the amount of residual gland. The side with the complete resection will not be involved once hyperthyroidism recurs. This can maximally reduce the chance of hyperthyroidism recurrence while retaining a small amount of gland. In addition, thyroid function can be maintained at the normal level in the long term with postoperative levothyroxine supplementation. So, it can be an important choice for carefully selected patients with Graves’ disease. Near-total resection (with a retained gland of less than 0.5 g) was performed instead of total resection when a lobectomy was difficult to complete. For patients who had hyperthyroidism combined with thyroid cancer or secondary hyperthyroidism, total or near-total resection was performed.
Unilateral subtotal or near-total lobectomy was performed in most patients with unilateral benign nodules in the early stage of this study. Bilateral subtotal resection was performed on some patients with bilateral benign nodules. As we know, the surgeon cannot touch the thyroid tissue in ETE directly. Thus, small nodules may be left behind when there is gland retained, and this may be the main source of postoperative recurrence. Therefore, total resection is reasonable [23–25]. However, total resection may also increase the risk of complications during the surgery, although it was safe in our study. Thus, bilateral near-total resection may be the best choice for the cases, in which it is difficult to achieve total resection, and it can maximally reduce the chance of recurrence after surgery without increasing the possibility of injuries of the RLN and the parathyroid gland.
The technique of thyroid gland suspension is very important in our study, especially for huge thyroid goiters and thyroid glands, which are located behind the sternum. We have benefited from when the surgery was preformed in the patients who had a short neck and in the male patients whose sternocleidomastoid was very strong, which made the thyroid gland extend behind the neck and therefore hard to expose. Since the thyroid gland can be moved into different directions to help expose it, the difficulty of the surgery and the risk of converting to open surgery can be significantly reduced.
Whether to clear lateral cervical lymph nodes preventatively in treating papillary carcinoma without clinical evidence indicating metastasis is still controversial [26]. Therefore, total resection plus ipsilateral central lymphadenectomy was performed for patients without lateral cervical lymph node enlargement in our study. Open functional cervical lymphadenectomy was performed for patients with PTC with lateral cervical lymph node enlargement. The resection of lymph nodes behind the sternum is the most difficult part of this surgery when lymph node resection was carried out in the center zone. Therefore, we pulled the lymph nodes and fat tissue upward to reach the thymus gland when the lymph node resection was carried out at the lower pole and pretracheal. None of the patients had any residual lymph nodes indicating metastasis of thyroid cancer on 131I scans. A majority of the patients were treated with 131I therapy postoperatively and levothyroxine replacement according to the most updated ATA. None of the patients had thyroid cancer recurrence in the follow-up period.
Prevention of complications
In our study, the RLN was partially exposed to reveal its position and course during thyroidectomy, while it was fully exposed when lymph node clearance was carried out in the central zone. Intraoperative neuromonitoring system(IONM) can be used to identify the RLN in lymph node clearance; however, considering that this would significantly increase the cost and we could protect the RLN very well by carefully operation, it has not been routinely used. For the patients who had temporary vocal cord paralysis, the movement function of the vocal cords could be well recovered by pronunciation training. We also pay attention to protect superior laryngeal nerve in this surgery, we pulled the thyroid gland outward to cut off the suspensory ligaments, and cut off the superior artery close to the thyroid gland to avoid superior laryngeal nerve.
The inferior parathyroid generally locates between the two capsules of thyroid and beneath the inferior artery. The superior parathyroid generally locates near the place where the RLN goes into the throat, which can make it easily be identified and reserved. During the thyroidectomy of benign thyroid disease, we separated the tissues closely to the thyroid gland, therefore, the parathyroid gland and its vessels and fat tissues could be preserved. However, the inferior parathyroid had a risk of being resected in the PTC thyroidectomy due to the complete resection of central lymph node, and the function of parathyroid might be injured because of the injury of its blood supply, even though it has not been resected. Therefore, re-implantation of parathyroid was performed once it was confirmed. The location of superior parathyroid is relatively fixed, and we can preserve it very well. There was no permanent hypoparathyroidism in our series, which might have benefited a lot from this strategy. Although nanocarbon can be used to recognize the lymph nodes in PTC thyroidectomy, which can recognize the parathyroid indirectly, it also has its disadvantages, such as lymph nodes cannot be displayed whose lymphatic vessels had been clogged, which may lead to confuse with parathyroid. Considering that this technique would significantly increase the cost, and we could prevent permanent hypoparathyroidism through the strategy mentioned above, we had not used nanocarbon routinely.
This surgery involves the breast and the pectoralis major muscle more than other approaches because the observation port is closer to the lateral side of the chest wall. Therefore, accidental trocar insertion into the breast should be avoided in women, and accidental insertion into the pectoralis major muscle should be avoided in men. For underweight patients whose subcutaneous fat layer is relatively thin, more attention should be paid to prevent damage to the skin during subcutaneous separation. To ensure that the trocar is inserted into the subcutaneous layer accurately, we injected inflation liquid along the path of the trocar and the area in which tissue separation was needed. This method can effectively help to find the right layer and reduce the risk of bleeding and skin punctures by the trocar.
Attentions should be paid to bleeding in the trocar tunnel and subcutaneous tissue during this approach. We routinely observed whether there was active bleeding in the operation tunnel or subcutaneous tissue in the neck and chest before withdrawing the endoscope. Bleeding in the operation tunnel can be treated with a suture and pressure to prevent blood accumulation in the subcutaneous space of the neck, which may lead to serious consequences. However, there were three patients still needed for re-operation to stop bleeding even with this strategy. We also checked whether there was bleeding in the operation tunnel or subcutaneous bleeding in the neck after carbon dioxide was discharged. Our experience has shown that this strategy can effectively rule out the possibility that the already injured veins do not bleed under the air pressure, yet start bleeding once the air pressure disappears.
Postoperative drainage and discomfort related to the operation
The inflation liquid was used to help separate the subcutaneous tissues during the operation, and postoperative drainage was applied to reduce the chance of subcutaneous effusion and infection. The neck should be kept immobile and hot and solid food should be avoided after the surgery to reduce the time needed for the drainage tube, and reduce the length of hospital stay after surgery. There is no need to use antibiotics prophylactically. Compared to ETE through a cervical approach, this surgery operated over a longer distance, and the range of subcutaneous separation is larger. Hence, postoperative swallowing discomfort and skin traction in the neck and chest may occur in a small number of patients, particularly in underweight patients. Therefore, it is necessary to explain the postoperative discomfort related to the operation to the patients before the surgery.
The advantages of ETE via areola approach
This approach has the advantages of handling bilateral lesions simultaneously, performing lymph node dissection, over a long distance between the surgical incision and the neck, which is similar to ETE via the breast approach. The surgical incision of this surgery is even more concealed compared to ETE via the breast approach (Fig. 2). In addition, scar hyperplasia due to skin tension does not occur because the skin tension around the areola is relatively small. Young women 10–30 years of age were more satisfied with the cosmetic results of our operation than older women (Table 5). The resected tissue samples were taken out through the tunnel where the surrounding tissues are relatively loose and easy to expand. The feedback from pathologists showed that these samples were more complete and it was easier to identify nodules compared to samples from the ETE via the breast approach.
Although the surgical incision of robotic transaxillary thyroidectomy is relatively concealed, the surgical incision is relatively large due to the design of single hole. Moreover, this procedure requires a robotic surgical system, which is very expensive and has a lengthy learning curve as the author mentioned, and these may limit its widespread application [27, 28]. Although ETE via areola approach still leaves very small surgical scars at the edge of the areolas, which makes its cosmetic results not as good as ETE via the oral vestibular approach which we developed [29], ETE via the oral approach is still in the exploratory stage. Therefore, ETE via the areola approach is still the choice of most patients with thyroid disease.
Conclusion
ETE via the areola approach for patients with benign goiters, Graves’ disease, secondary hyperthyroidism, and papillary carcinomas without metastasis to lateral cervical lymph nodes is an effective and safe procedure with excellent cosmetic results. Dunhill’s operation with approximately 2–3 g of gland retained can be an important choice for carefully selected patients with Graves’ disease. Bilateral near-total resection may be the best choice for benign nodules. Total resection plus ipsilateral central lymphadenectomy plus postoperatively 131I and levothyroxine replacement therapy are an effective strategy for the PTC patients without lateral cervical lymph node enlargement.
References
Gagner M (1996) Endoscopic subtotal parathyroidectomy in patients with primary hyperparathyroidism. Br J Surg 83:875
Huscher CS, Chiodini S, Napolitano C, Recher A (1997) Endoscopic right thyroid lobectomy. Surg Endosc 11:877
Miccoli P, Berti P, Raffaelli M, Conte M, Materazzi G, Galleri D (2001) Minimally invasive video-assisted thyroidectomy. Am J Surg 181:567–570
Shimizu K, Akira S, Tanaka S (1998) Video-assisted neck surgery: endoscopic resection of benign thyroid tumor aiming at scarless surgery on the neck. J Surg Oncol 69:178–180
Ikeda Y, Takami H, Sasaki Y, Kan S, Niimi M (2000) Endoscopic neck surgery by the axillary approach. J Am Coll Surg 191:336–340
Ohgami M, Ishii S, Arisawa Y, Ohmori T, Noga K, Furukawa T, Kitajima M (2000) Scarless endoscopic thyroidectomy: breast approach for better cosmesis. Surg Laparosc Endosc Percutan Tech 10:1–4
Sasaki A, Nakajima J, Ikeda K, Otsuka K, Koeda K, Wakabayashi G (2008) Endoscopic thyroidectomy by the breast approach: a single institution’s 9-year experience. World J Surg 32:381–385
Cooper DS, Doherty GM, Haugen BR, Kloos RT, Lee SL, Mandel SJ, Mazzaferri EL, McIver B, Pacini F, Schlumberger M, Sherman SI, Steward DL, Tuttle RM, Ata (2009) Revised American Thyroid Association Management Guidelines for Patients with Thyroid Nodules and Differentiated Thyroid Cancer. Thyroid 19:1167–1214
Smith BR, Cooper DS, Doherty GM, Haugen BR, Kloos RT, Lee SL, Mandel SJ, Mazzaferri EL, McIver B, Sherman SI, Tuttle RM, Amer Thyroid Assoc Guidelines Taskforce (2006) Management guidelines for patients with thyroid nodules and differentiated thyroid cancer. Thyroid 16:109
Singer PA, Cooper DS, Daniels GH, Ladenson PW, Greenspan FS, Levy EG, Braverman LE, Clark OH, McDougall IR, Ain KV, Dorfman SG (1996) Treatment guidelines for patients with thyroid nodules and well-differentiated thyroid cancer. American Thyroid Association. Arch Intern Med 156:2165–2172
Sasaki A, Nakajima J, Ikeda K, Otsuka K, Koeda K, Wakabayashi G (2008) Endoscopic thyroidectomy by the breast approach: a single institution’s 9-year experience. World J Surg 32:381–385
Miccoli P, Minuto MN, Ugolini C, Pisano R, Fosso A, Berti P (2008) Minimally invasive video-assisted thyroidectomy for benign thyroid disease: an evidence-based review. World J Surg 32:1333–1340
Wang C-c, Yang J-g, Hu Y-z, Chen J, Xu P, Su C (2007) Endoscopic thyroidectomy via chest and breasts approach in 500 cases. Zhonghua er bi yan hou tou jing wai ke za zhi = Chin J Otorhinolaryngol Head Neck Surg 42:919–923
Maeda S, Uga T, Hayashida N, Ishigaki K, Furui J, Kanematsu T (2006) Video-assisted subtotal or near-total thyroidectomy for Graves’ disease. Br J Surg 93:61–66
Shimizu K, Tanaka S (2003) Asian perspective on endoscopic thyroidectom—a review of 193 cases. Asian journal of surgery/Asian Surgical Association 26:92–100
Yamamoto M, Sasaki A, Asahi T, Shimada Y, Sato N, Nakajima J, Mashima R, Saito K (2001) Endoscopic subtotal thyroidectomy for patients with Graves’ disease. Surg Today 31:1–4
Sasaki A, Nitta H, Otsuka K, Obuchi T, Kurihara H, Wakabayashi G (2009) Endoscopic subtotal thyroidectomy: the procedure of choice for graves’ disease? World J Surg 33:67–71
Li ZY, Wang P, Wang Y, Xu SM, Cao LP, Que RS (2010) Endoscopic thyroidectomy via breast approach for patients with graves’ disease. World J Surg 34:2228–2232
Wilhelm SM, McHenry CR (2010) Total thyroidectomy is superior to subtotal thyroidectomy for management of graves’ disease in the United States. World J Surg 34:1261–1264
Stalberg P, Svensson A, Hessman O, Akerstrom G, Hellman P (2008) Surgical treatment of Graves’ disease: evidence-based approach. World J Surg 32:1269–1277
Ku CF, Lo CY, Chan WF, Kung AWC, Lam KSL (2005) Total thyroidectomy replaces subtotal thyroidectomy as the preferred surgical treatment for Graves’ disease. Anz J Surg 75:528–531
Sugino K, Ito K, Nagahama M, Kitagawa W, Shibuya H, Ito K (2008) Surgical management of Graves’ disease—10-year prospective trial at a single institution. Endocr J 55:161–167
Dogan L, Karaman N, Yilmaz KB, Ozaslan C, Atalay C (2011) Total thyroidectomy for the surgical treatment of multinodular goiter. Surg Today 41:323–327
Albayrak Y, Demiryilmaz I, Kaya Z, Aylu B, Guzel IC, Ozcan O, Aslan S, Yenisolak A, Ozturk M, Celik S (2011) Comparison of total thyroidectomy, bilateral subtotal thyroidectomy and Dunhill operations in the treatment of benign thyroid disorders. Minerva Chir 66:189–195
Agarwal G, Aggarwal V (2008) Is total thyroidectomy the surgical procedure of choice for benign multinodular goiter? An evidence-based review. World J Surg 32:1313–1324
Bhattacharyya N (2003) Surgical treatment of cervical nodal metastases in patients with papillary thyroid carcinoma. Arch Otolaryngol Head Neck Surg 129:1101–1104
Kandil EH, Noureldine SI, Yao L, Slakey DP (2012) Robotic transaxillary thyroidectomy: an examination of the first one hundred cases. J Am Coll Surg 214:558–564
Ryu HR, Kang S-W, Lee SH, Rhee KY, Jeong JJ, Nam K-H, Chung WY, Park CS (2010) Feasibility and safety of a new robotic thyroidectomy through a gasless, transaxillary single-incision approach. J Am Coll Surg 211:e13–e19
Wang C, Zhai H, Liu W, Li J, Yang J, Hu Y, Huang J, Yang W, Pan Y, Ding H (2014) Thyroidectomy: a novel endoscopic oral vestibular approach. Surgery 155:33–38
Acknowledgments
This work was supported by Science and Technology Development Fund Project, Macao (Grant 027/2010/A).
Disclosures
Drs. Cunchuan Wang, Zhiqi Feng, Jinyi Li, Wah Yang, Hening Zhai, Nim Choi, Jingge Yang, Youzhu Hu, Yunlong Pan, and Guo Cao have no conflicts of interest or financial ties to disclose.
Author information
Authors and Affiliations
Corresponding author
Electronic supplementary material
Below is the link to the electronic supplementary material.
Supplementary material 1 (WMV 58568 kb)
Supplementary material 2 (WMV 122658 kb)
Supplementary material 3 (WMV 40514 kb)
Supplementary material 4 (WMV 59296 kb)
Rights and permissions
About this article
Cite this article
Wang, C., Feng, Z., Li, J. et al. Endoscopic thyroidectomy via areola approach: summary of 1,250 cases in a single institution. Surg Endosc 29, 192–201 (2015). https://doi.org/10.1007/s00464-014-3658-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00464-014-3658-8