Abstract
Background
The aim of this study was to evaluate the feasibility and outcomes of endoscopic subtotal thyroidectomy for Graves’ disease.
Methods
From August 1998 to April 2008, a total of 100 patients with benign thyroid diseases underwent endoscopic thyroidectomy via the breast approach. Among these patients, 42 underwent subtotal thyroidectomy for Graves’ disease.
Results
The resection was successfully completed endoscopically in 41 patients (98%). Overall, the mean operating time, mean blood loss, and mean resected thyroid weight were 277 minutes, 76 ml, and 49.9 g, respectively. As the resected thyroid weight increased, the operating time was significantly prolonged and the blood loss significantly increased. Morbidities included one permanent and one temporary case of recurrent laryngeal nerve palsy with hypocalcemia. A hypertrophic scar was seen in the right breast medial margin in three men. Thyroid function was classified as euthyroidism, hypothyroidism, and recurrent hyperthyroidism in 5, 34, and 3 patients, respectively. At 92 months of median follow-up, two patients had modest operation-associated symptoms: one with swallowing discomfort and another with paresthesia in the anterior chest wall at the time of discharge. However, both patients’ symptoms disappeared within 36 months after surgery. Young women were highly satisfied, with an overall mean satisfaction rating of 9.3 points.
Conclusions
Although the endoscopic approach may be relatively contraindicated for large thyroid glands, endoscopic subtotal thyroidectomy via the breast approach is a safe, feasible procedure with excellent cosmetic benefits, and it may be the procedure of choice in carefully selected patients with Graves’ disease.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Radioiodine therapy for Graves’ disease has been considered first-line therapy in the United States [1]. Previous reports from the United States have also emphasized the advantages of thyroidectomy for Graves’ disease and recommended this treatment for selected patients [2, 3]. In Asian countries, thyroidectomy is a common option for Graves’ patients with a large goiter or concomitant thyroid nodule or in those who have failed to respond to antithyroid drugs [4–10]. When surgical treatment is indicated for Graves’ disease, a bilateral subtotal thyroidectomy has been recommended as the standard procedure [5, 7].
Technological innovations have rapidly improved minimally invasive thyroid surgery; however, endoscopic thyroidectomy has rarely been used to treat Graves’ disease because of its highly vascular pattern [3]. The aim of this study was to evaluate the feasibility and outcomes of endoscopic subtotal thyroidectomy for patients with Graves’ disease via the breast approach.
Patients and methods
Patients
From August 1998 to April 2008, a total of 100 patients with benign thyroid diseases underwent endoscopic thyroidectomy via the breast approach (completely closed approach) at Iwate Medical University Hospital. Among the patients, 42 underwent subtotal thyroidectomy for Graves’ disease. These patients included 35 women (83%) with a mean age of 27.6 years (range 11–62 years), 9 (21%) of whom were children under 18 years of age. Endoscopic subtotal thyroidectomy was selected only if patients gave informed consent and desired a procedure that would leave no operative scar on the neck. The indications for this procedure in the Graves’ disease patients were as follows: Antithyroid drugs were contraindicated because of adverse drug reactions or no desire for radioiodine therapy; there was a large goiter refractory to antithyroid drugs; it was the patient’s preference; and the expected thyroid volume was < 100 ml as measured by computed tomography (CT) volumetry. All patients were euthyroid at the time of operation and had been given Lugol’s iodine 7 to 10 days before surgery.
All patients were assessed by a retrospective review of a prospective database. To evaluate the feasibility and cosmetic results of the authors’ endoscopic procedure, a questionnaire was conducted by telephone for patients more than 1 year postoperative. The questionnaire was applied by independent surgeons (not those operating on the patients). Surveyed information included the presence or absence of swallowing discomfort, hypesthesia or paresthesia in the anterior chest or neck, the presence or absence of hypertrophic scarring, and a cosmetic satisfaction score that ranged from 0 to 10 (extremely dissatisfied to extremely satisfied, respectively).
Statistical analysis
Statistical analysis was performed using Fisher’s exact test for categoric variables. Differences in the continuous variables were tested by Student’s t-test and checked by the Mann-Whitney U-test using StatView software (SAS Institute, Cary, NC, USA). Values are expressed as the mean and standard deviation. A value of p < 0·05 was considered statistically significant.
Surgical technique
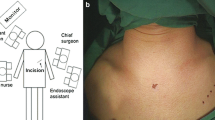
Endoscopic thyroidectomy via the breast approach was undertaken as described in previous reports [5, 9]. The subcutaneous space from the breast area to the subplatysmal space in the neck was bluntly dissected through the right breast medial margin using a dressing forceps. Carbon dioxide was insufflated at 5 mmHg to create the operative space. A 5-mm trocar for the operator was endoscopically inserted into the bilateral areola superior margin, and the working space was completely created from the anterior chest to the cervical region using a Harmonic Scalpel (Johnson-Johnson Medical, Cincinnati, OH, USA). The thyroid vessels were divided using the Harmonic Scalpel. The thyroid around Berry’s ligament was resected by moving from the inferior pole toward the superior pole, leaving the thyroid dorsal capsule intact in the superior position, which prevents damage to blood flow from the inferior thyroid artery to the parathyroid as well as damage to the recurrent laryngeal nerve (RLN) (Fig. 1). To avoid recurrent hyperthyroidism due to erroneous estimation of the thyroid remnant weight, a 1-g sponge model measuring the thyroid remnant weight was placed adjacent to the gland, and the thyroid parenchyma was resected in comparison with the thyroid model (Fig. 2).
Results
Altogether, 41 (98%) patients’ operations were successfully completed endoscopically. Overall, the mean operating time, mean blood loss, and mean resected thyroid weight were 277 minutes, 76 ml, and 49.9 g, respectively. Comparison of outcomes between early (n = 21) and late (n = 21) periods revealed equal operating time (276.6 vs. 277.4 minutes) in more patients with enlarged thyroids (48.5 vs. 51.2 g) but a tendency for a reduction in blood loss (93.7 vs. 59.1 ml) when the surgeon had more experience in the procedure. There was one case of a female patient for whom conversion to an open procedure had to be made because bleeding from the thyroid prevented us from performing the pyramidal portion removal procedure. We attempted to complete the operation endoscopically, but we had to convert the approach when the amount of bleeding reached 400 ml. Univariate analysis of variance (ANOVA) showed a statistically significant difference in operating time and blood loss among the three groups of resected thyroid weight. The operating time was significantly prolonged (Fig. 3) and the blood loss significantly increased as the resected thyroid weight increased (Fig. 4).
Morbidities included one permanent RLN palsy and one temporary RLN palsy with hypocalcemia. A mild hypertrophic scar was seen in the right breast medial margin in three men 1 year after surgery. The temporary RLN palsy and the hypocalcemia resolved 2 months and 3 days postoperatively, respectively.
Following endoscopic subtotal thyroidectomy, thyroid function was classified as euthyroidism, hypothyroidism, and recurrent hyperthyroidism in 5, 34, and 3 patients, respectively. Treatment for the three patients with recurrence was radioiodine therapy for two and medical therapy (antithyroid drug) for a 15-year-old girl (Table 1).
A questionnaire was conducted for 42 patients more than 1 year postoperatively, with a response rate of 95%. The median follow-up period of the questionnaire was 92 months. Two patients had modest operation-associated symptoms: one had swallowing discomfort, and the other had paresthesia in the anterior chest wall at the time of discharge. Both patients’ symptoms disappeared within 36 months after surgery.
Overall, the level of satisfaction with endoscopic thyroidectomy was “satisfied,” “equivocal,” and “unsatisfied” in 39, 1, and 0 patients, respectively. Young women were highly satisfied, with an overall mean satisfaction rating of 9.3 points; one man with relapse was less satisfied (Table 2).
Discussion
Assessing the activity of autoimmune mechanisms by measuring thyroid-stimulating hormone receptor antibody (TRAb) levels and the use of radioiodine therapy in the treatment of Graves’ disease have increased, with the result that surgical procedures—with their risk of complications such as prominent scars, permanent RLN palsy, and hypoparathyroidism—have been used less frequently. Nonetheless, surgical procedures providing the earliest, most reliable efficacy are still required and performed in carefully selected patients worldwide [11]. Since the authors developed a safe endoscopic subtotal thyroidectomy procedure for Graves’ disease and reported the first case in 1999, we have improved the procedure through clinical experience [5, 9].
During surgery for Graves’ disease, it is important to prevent complications and stop bleeding associated with dissection of the thyroid gland, where blood flow is high. Bipolar coagulation forceps are greatly effective for hemostasis of parenchymal organs such as the liver, spleen, and thyroid gland. In patients with markedly enlarged thyroid glands, a good field of view can be obtained by fractional resection of the lower thyroid gland before thyroidectomy is performed on the upper pole of the thyroid gland and Berry’s ligament, effectively reducing the operating time and preventing complications.
Thyroid function is most closely correlated with the weight of the thyroid remnant, which is determined depending on the purpose of the surgery [12]. Whereas approximately 6 g of the gland is left behind to normalize postoperative thyroid function, as is less than 2 g to prevent relapse, total thyroidectomy is selected to normalize the TRAb level [6, 7, 13]. Sugino et al. [14] reported that less than 3 g of the thyroid gland should be left behind in children with highly active Graves’ disease. We attempted to leave behind 2 g of thyroid remnant [15]. Hypothyroidism was seen at a high percentage; however, the aim of this procedure is to keep thyroid function lower to prevent recurrence. It is challenging to determine an appropriate functional remnant volume of thyroid prior to operation as the autoimmune status may change during the operation. For these reasons, we believe that follow-up substitution-thyroid medication is the key to acquiring a better prognosis. However, the safety and advantages should be carefully assessed for endoscopic subtotal thyroidectomy in cosmetically concerned patients because the risk of complications is increased if less thyroid gland is left behind.
Sugino et al. [7] reported the recurrence rate of hyperthyroidism to be 12.6% among 1897 patients who underwent open subtotal thyroidectomy when the surgeons left behind 3 to 8 g of thyroid gland; 5.2% of the 1897 patients had overt hyperthyroidism, requiring a therapeutic option. Palit et al. [16] a reported 7.9% recurrence rate in a meta-analysis of 6703 and 538 patients who underwent open subtotal thyroidectomy and total thyroidectomy, respectively. In the present study, the recurrence rate was 7.1%, but all of these were the early period of the study (March 2000 to March 2001). No recurrences occurred in the most recent 22 patients.
Permanent RLN palsy occurred in 0.9% of the open total thyroidectomy patients and hypoparathyroidism in 1.6%, whereas the corresponding figures for the open subtotal thyroidectomy patients were 0.7% and 1.0%, respectively [16]. In the present study, the incidence of permanent RLN palsy was 2.4% and that of hypoparathyroidism 0%, showing no significant difference from the previous literature [17, 18]. Although the rate of RLN palsy may seem to be higher than usual, the denominator was only 42; hence one case gives a rate of 2.4%. It should also be noted that we have not experienced any cases of RLN palsy since the first case; we speculate that the cause of the palsy was heat damage from a Harmonic Scalpel around Berry’s ligament. We now use a Harmonic Scalpel at least 1 cm away from Berry’s ligament to avoid unnecessary nerve injuries.
There are patients who require surgery for treatment of their Graves’ disease, and it remains the most appropriate therapeutic option for carefully selected patients [19]. With conventional procedures cervical skin and platysma are divided to create a skin flap, whereas during endoscopic procedures they are not separated, with the aim of preventing postoperative complaints [20–22].
At 92 months of median follow-up, no swallowing discomfort, hypesthesia, or paresthesia in the anterior chest or neck has been reported, providing evidence of the long-term safety of this procedure. Allowing that the evaluation of satisfaction with endoscopic thyroidectomy via the breast approach was subjective and biased, the results still show extremely high patient satisfaction with the operative wound and appearance of the neck. Because thyroid surgery is performed near the body surface, it is unlikely that endoscopic subtotal thyroidectomy, even with prolonged operating time, is excessively invasive.
The authors believe that endoscopic subtotal thyroidectomy, which offers a cosmetic advantage because the procedure leaves no operative wound in the neck and reduces complaints of sensory disorder and swallowing discomfort associated with cervical incisions, is useful for improving postoperative quality of life if selected exclusively for patients with a high risk of relapse or in whom relapse must be avoided. Although it is important to be careful when selecting endoscopic subtotal thyroidectomy to treat patients for whom surgery is indicated, this procedure is highly recommended for young women. In patients with a thyroid weight > 60 g, the cervical approach is safer than endoscopic approaches, as the latter is associated with increased surgical difficulty, prolonged operating time, and increased blood loss.
It should also be noted that we performed the endoscopic subtotal thyroidectomies with the support of the Japanese Advanced Medical Treatment system, with which the cost is lower than open subtotal thyroidectomy (¥ 124,000 vs. ¥ 160,000) regardless of the time length of the operation. In addition, although there was no statistically significant difference, the cost for postoperative treatment was lower in the endoscopic group than in the open procedure group.
Conclusion
Although the endoscopic approach may be relatively contradicted for large thyroid glands, endoscopic subtotal thyroidectomy via the breast approach is a safe, feasible procedure, with excellent cosmetic benefits. It may be the procedure of choice in carefully selected patients with Graves’ disease.
References
Duh QY (1999) Thyroidectomy for the treatment of Graves’ disease. Thyroid 9:259–261
Feliciano DV (1992) Everything you wanted to know about Graves’ disease. Am J Surg 164:404–411
Alsanea O, Clark OH (2000) Treatment of Graves’ disease: the advantages of surgery. Endocrinol Metab Clin North Am 29:321–337
Yamamoto M, Sasaki A, Asahi H et al (1999) Endoscopic subtotal thyroidectomy for Graves’ disease (in Japanese with English abstract). Naibunpitsugeka (Endocr Surg) 16:117–121
Yamamoto M, Sasaki A, Asahi H et al (2001) Endoscopic subtotal thyroidectomy for patients with Graves’ disease. Surg Today 31:1–4
Maeda S, Uga T, Hayashida N et al (2006) Video-assisted subtotal or near-total thyroidectomy for Graves’ disease. Br J Surg 93:61–66
Sugino K, Ito K, Nagahama M et al (2008) Surgical management of Graves’ disease: 10-year prospective trial at a single institution. Endocr J 55:161–167
Pradeep PV, Agarwal A, Baxi M et al (2007) Safety and efficacy of surgical management of hyperthyroidism: 15-year experience from a tertiary care center in a developing country. World J Surg 31:306–312
Sasaki A, Nakajima J, Ikeda K et al (2008) Endoscopic thyroidectomy by the breast approach: a single institution’s 9-year experience. World J Surg 32:381–385
Shimizu K, Tanaka S (2003) Asian perspective on endoscopic thyroidectomy: a review of 193 cases. Asian J Surg 26:92–100
Berti P, Materazzi G, Galleri D et al (2004) Video-assisted thyroidectomy for Graves’ disease: report of a preliminary experience. Surg Endosc 18:1208–1210
Sugino K, Mimura T, Ozaki O et al (1995) Early recurrence of hyperthyroidism in patients with Graves’ disease treated by subtotal thyroidectomy. World J Surg 19:648–652
Moreno P, Gómez JM, Gómez N et al (2006) Subtotal thyroidectomy: a reliable method to achieve euthyroidism in Graves’ disease—prognostic factors. World J Surg 30:1950–1956
Sugino K, Ito K, Mimura T et al (2004) Surgical treatment of Graves’ disease in children. Thyroid 14:447–452
Kurihara H (2006) Operative treatment of Graves’ disease: supersubtotal resection of the thyroid gland. Vestn Khir Im Grek 165:28–30
Palit TK, Miller CC 3rd, Miltenburg DM (2000) The efficacy of thyroidectomy for Graves’ disease: a meta-analysis. J Surg Res 90:161–165
Bron LP, O’Brien CJ (2004) Total thyroidectomy for clinically benign disease of the thyroid gland. Br J Surg 91:569–574
Bilosi M, Binquet C, Goudet P et al (2002) Is subtotal thyroidectomy still indicated in patients with Graves’ disease? Ann Chir 127:115–120
Tan CTK, Cheah WK, Delbridge L (2008) “Scarless” (in the neck) endoscopic thyroidectomy (SET): an evidence-based review of published techniques. World J Surg 32:1349–1357
Ikeda Y, Takami H, Niimi M et al (2001) Endoscopic thyroidectomy by the axillary approach. Surg Endosc 15:1362–1364
Ikeda Y, Takami H, Sasaki Y et al (2002) Comparative study of thyroidectomies: endoscopic surgery vs conventional open surgery. Surg Endosc 16:1741–1745
Takami H, Ikeda Y (2003) Total endoscopic thyroidectomy. Asian J Surg 26:82–85
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Sasaki, A., Nitta, H., Otsuka, K. et al. Endoscopic Subtotal Thyroidectomy: The Procedure of Choice for Graves’ disease?. World J Surg 33, 67–71 (2009). https://doi.org/10.1007/s00268-008-9783-6
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00268-008-9783-6