Abstract
Background
Hydatid recurrence after surgery is about 10 %. It still constitutes a problem both in terms of pathophysiology and management of recurrence.
Aim
The aim of this study was to assess the management of abdominal hydatid recurrence after surgical treatment for liver hydatid cyst and to identify the predictive factors of recurrence.
Methods
We retrospectively included all the patients operated on between January 1, 2008, and December 31, 2012, in the Department “B” of Charles Nicolle Hospital (Tunisia), for abdominal hydatid recurrence. Sixteen men and 33 women, with a median age of 45 years, were included. For all patients, clinical variables and morphological and intra-operative characteristics concerning both the hydatid cysts previously treated and the recurrent cysts were collected. Surgical procedures were recorded as well as the immediate and long-term outcomes. Comparative studies were performed: “extrahepatic recurrence versus No,” “peritoneal recurrence versus No,” and “open approach versus laparoscopic approach.” A univariate analysis followed by a multivariate analysis was carried out to determine predictive factors of hydatid recurrence.
Results
Comparative analysis showed that laparoscopic approach, segments II and III localization, and postoperative complications during the first intervention were associated with a greater number of both peritoneal and extrahepatic hydatid recurrence. Multivariate analysis retained the laparoscopic approach as a predictive factor of both peritoneal recurrence (OR 5.5; 95 % CI 1.56; p = 0.008) and abdominal extrahepatic recurrence (OR 3.54; 95 % CI 1.08; p = 0.035).
Conclusion
Laparoscopic approach for the treatment of liver hydatid cysts was associated with a higher rate of extrahepatic and peritoneal recurrence than open.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Hydatid recurrence after surgery for hydatid cyst of the liver is around 10 % [1]. This rate is higher after conservative surgery than radical surgery [2–5]. Predictive factors of hydatid recurrence in the medical literature were the following: (1) leaving in place exogenous daughter cyst especially in long-standing cysts, and (2) spillage of the cystic contents [1, 6]. By avoiding these two factors, some authors reported recurrence rate below 10 % independently of the surgical techniques and the surgical approaches (open or laparoscopic) [6, 7]. After introduction of laparoscopy, several articles [8–10] reported surgical treatment of liver hydatid cyst by laparoscopic approach. These articles showed the feasibility of the new laparoscopic approach and reported a lower recurrence rate around 3 % [8, 9].
The aim of this study was to assess the management of abdominal hydatid recurrence after surgical treatment for liver hydatid cyst, operated on in surgical unit B of Charles Nicolle Hospital, and to identify the predictive factors of recurrence.
Methods
Definition of recurrence
Hydatid recurrence is defined as the appearance of new active cysts after therapy of intrahepatic or extrahepatic disease. It manifests as reappearance of live cysts at the site of a previously treated cyst or the appearance of new extrahepatic disease resulting from procedure-related spillage [1].
Eligibility criteria
We evaluated retrospectively the consecutive patients surgically treated for hydatid recurrence at the surgical unit “B” of Charles Nicolle Hospital, Tunis, Tunisia, between January 1, 2008, and December 31, 2012. Forty nine patients were included. All included patients were operated on previously for liver hydatid cyst associated or not with other abdominal localization. Patients who underwent surgery elsewhere for hepatic hydatid disease and referred to our surgical unit for recurrence were included also in this study. For all patients, the diagnosis of hydatid recurrence was made based on abdominal ultrasonography (US) and computed tomography (CT) findings. Echinococcus granulosus serology (ELISA) was not performed for all patients. Indeed, the positivity of this test after hydatid surgery may be confusing [2, 10].
Were excluded two patients with hydatid recurrence treated by the method of Puncture, Aspiration, Injection and Re-aspiration (PAIR) [11].
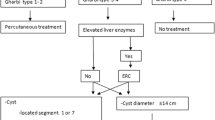
Primary surgical procedures
Two surgical approaches have been used for the primary treatment of hydatid cysts: laparoscopic approach and open approach. Conservative surgery was performed for all patients who had laparoscopic approach. The different steps through laparoscopic approach were carried out in the same; after creation of CO2 pneumoperitoneum, (1) injection of hypertonic saline (9 %) around the liver, (2) aspiration of the cyst via a Monod trocar (Fig. 1), and (3) if the cystic content was not bilious, injection of hypertonic saline via the same trocar was performed. In case of bilious intracystic content, the residual cavity was inspected looking for bilio-cystic fistula. The small bilio-cystic fistulas (<5 mm) were respected, whereas large bilio-cystic fistulas (≥5 mm) were intubated and drained. (4) Hypertonic saline was left into the cyst during 10 min afterward the cyst content was aspirated, and then, (5) unroofing technique was afterward performed.
As regards the open approach, conservative surgery (unroofing ± omentoplasty) [12] was used for all patients except two: one underwent pericystectomy [13] and another one underwent hepatic resection [13].
Data collection
In first step concerning primary intervention, the following variables were culled: age, sex, and medical history of the primary hydatid disease treated (clinical presentation, number, size and location of the hydatid cyst, imaging findings, surgical approach and technique, intra-operative findings, surgical outcomes, and antiparasitic drug treatment intake). Concerning hydatid recurrence, the following variables were culled: delay of recurrence, the number of previous recurrence episodes surgically treated, number, size and location of recurrent hydatid disease, and surgical technique.
Outcome measures after surgery for hydatid recurrence
Two variables were considered: (1) Postoperative mortality was defined as any and all deaths occurring during hospital stay or within 30 days after discharge, and (2) postoperative morbidity was defined according to the Centers for Disease Control and Prevention classification [14] with some modifications. Overall postoperative morbidity was modified to include the following: (1) organ/space surgical site infection [14]; (2) deep bleeding or hematoma, whether infected or not; (3) bile leakage as diagnosed by discharge through drainage, visualization through fistulography, or external bile tract drainage, or by endoscopic retrograde cholangiography.
Statistical analysis
All data were recorded using SPSS software, version 17 for Windows (SPSS Inc.). We conducted a descriptive analysis followed by comparative studies: (1) extrahepatic recurrence versus no recurrence, (2) peritoneal recurrence versus no recurrence, and (3) laparoscopic approach versus open approach. Qualitative variables were mentioned by its percentage and quantitative variables by mean ± standard deviation when distribution was Gaussian and otherwise by median and range values. Statistical comparisons were performed using the χ2 test for categorical variables and Student’s t test for continuous variables. Statistical significance was considered when p value was less than 0.05. Variables identified by univariate analysis were introduced in a logistic regression model to determine predictive factors of hydatid recurrence.
Results
Descriptive analysis (Table 1)
Forty nine patients were treated surgically for hydatid recurrence. The female/male ratio was 33/16 with a median age of 45 (range 23–84) years. Among these patients, 17 were referred with recurrent hydatid disease after previous surgery in other institute.
Concerning the primary hydatid disease, the most common symptom was pain in the right-upper quadrant in 33 patients (67 %), while 13 (27 %) patients showed clinical signs of complicated cyst as fever (2 cases), jaundice (9 cases), chest pain, and irritating cough related to a thoracic complication (one case) or signs of peritoneal irritation (one case). On the other hand, three patients (6 %) were asymptomatic. Hydatid disease was localized only in the liver in 44 cases (90 %), while other organs were also affected in the remaining 5 cases. The liver cyst was unique in 33 cases (67 %) and multiple in 16 cases (33 %). The average size of the larger cyst was 11.1 ± 4.1 (range 4–22) cm. The most common ultrasonographic appearance according to the classification of Gharbi was type III (54 %). Twenty-two patients were treated initially by laparoscopic approach, and open surgery was performed for the remaining 27 patients. In the group of open approach, two patients were treated by radical procedure (pericystectomy = 1, hepatic resection = 1). All the remaining patients underwent conservative treatment by laparoscopic or open approach. Among the 22 laparoscopic approaches, only one case of spillage was noted. There were two preemptive conversions due to difficulties to locate and/or to drain a large bilio-cystic fistula. Overall postoperative complications were made mainly of suppuration of the residual cavity (11 cases). None of the patients received preoperative or postoperative antiparasitic drug treatment. All details of clinical and imaging findings, surgical procedures, and postoperative complications of primary cysts are summarized in Table 1.
The delay of recurrence ranged from 7 months to 28 years with a median of 41 months. Nineteen patients (39 %) have already been treated for hydatid recurrences: Open approach was performed in 14 cases, and laparoscopic approach in 4 cases, and one patient was operated on previously at 3 times for hydatid disease (first by laparotomy and then two times by laparoscopy). The choice of surgical approach was at the discretion of the surgeon. The surgery was conservative in all these cases (Fig. 2).
Concerning the last hydatid recurrence (49 patients), the median number of recurrent cysts was 2 (range 1–12) and the average size of the larger cyst was 8.8 ± 3.9 (range 3–15) cm. The recurrence was localized only in the liver in 26 cases. Other organs were also affected in 14 cases, whereas recurrence occurred on extrahepatic sites only in 9 cases. The main site of extrahepatic recurrence was the peritoneal cavity (19 cases, 39 %). Peritoneal cysts were located mostly under the diaphragm, in the two paracolic gutters or in the pelvis (Fig. 3). Antiparasitic drug treatment has been associated with surgery only in 36 cases (74 %). The remaining patients have not received the antiparasitic drug due to unavailability of this treatment. Open surgery was performed for all 49 patients with hydatid recurrence. Postoperative adhesions were responsible for operative difficulties in 49 % of cases. All the sites of recurrence and the details of surgical procedures are presented in Table 2. One death occurred on postoperative day 2 owing to septic shock after surgery of an infected hydatid cyst complicated by rupture into the biliary tract with acute cholangitis. Postoperative complications included two external biliary fistulas which dried up spontaneously after 2 and 3 weeks, respectively. However, during the follow-up that ranges from 1 to 47 months (median follow-up = 13.5 months), nine patients out of 48 had new recurrence (19 %). Univariate analysis, comparing the nine patients with new recurrence versus the 39 patients without, showed no predictive variables.
(a, b) Peritoneal recurrence under the liver (white arrows), in the paracolic gutter (black arrows) and under the diaphragm (large white arrow) in a 44 year-old-man operated 7 years ago for hydatid cyst of the liver by laparoscopic approach. (c, d) peritoneal recurrence in the right paracolic gutter (black arrow) and the pelvis (white arrows)
Risk factors of peritoneal and extrahepatic recurrence
Three factors were associated with both intra-abdominal hydatid recurrence outside the liver and peritoneal recurrence: laparoscopic approach, segments II and III localization, and postoperative complications (suppuration of the residual cavity and/or external biliary fistula) (Table 3). Indeed, of the 22 patients treated by laparoscopy, 14 developed intra-abdominal recurrence outside the liver (p = 0.035) and 13 developed peritoneal recurrence (p = 0.008). It was the same for the 11 patients treated for cysts localized in segments II and III who developed intra-abdominal recurrence in 8 cases (p = 0.01) and peritoneal recurrence in 8 cases also (p = 0.006). As regards the 12 patients who have presented postoperative complications, 9 developed intra-abdominal recurrence (p = 0.025) and 8 developed peritoneal recurrence (p = 0.039). Multivariate analysis retained the laparoscopic approach as a predictive factor of both peritoneal recurrence with an odds ratio of 5.5 (95 % CI 1.56; p = 0.008) and intra-abdominal recurrence outside the liver with an odds ratio of 3.54 (95 % CI 1.08; p = 0.035).
Laparoscopic approach versus open approach (Table 4)
The comparison between laparoscopic and open approach while respecting the intent to treat and using the method of extreme bias showed that there was tendency to use laparoscopic approach for hydatid cysts of segments II, III, IV, V, VI (p = 0.089) and for single hepatic cysts (p = 0.065) without associated extrahepatic locations (p = 0.056). After open approach, recurrence was much more often located in the same previously treated site than after laparoscopy (p = 0.02). Moreover, postoperative complications were higher after laparoscopic approach (p = 0.002), and the delay of recurrence was shorter after laparoscopic approach (p = 0.004). By contrast, the operating difficulties during the intervention for recurrent hydatid disease were lower after a primary treatment by laparoscopic approach (p = 0.018).
Discussion
This study showed that both intra-abdominal recurrences outside the liver and peritoneal hydatid recurrence were more common after primary laparoscopic approach than a primary open approach (p = 0.01 and p = 0.006).
The proportion of patients with peritoneal recurrence in our study (39 %) was high compared to the series of Prousalidis et al. [7] who reported eight peritoneal recurrences of a total of 51 cases of hydatid recurrence after initial surgical treatment by open approach (recurrence rate = 15.7 %). Furthermore, only one case of peritoneal recurrence was observed by Kapan et al. [6] among the 8 hydatid recurrences of his series. The authors [6] did not specify whether the peritoneal recurrence has occurred after open or laparoscopic approach.
The laparoscopic approach has been identified in our study as the only risk factor for peritoneal recurrence by multivariate analysis. The other two factors identified by univariate analysis (postoperative complications and location of hydatid cysts in segments II and III) were related probably to the laparoscopic approach. Indeed, postoperative complications were higher after laparoscopic approach (p = 0.002), and there was a tendency to treat cysts of segments II, III, IV, V, VI by laparoscopic approach (p = 0.089).
The results of the laparoscopic approach in our series in terms of postoperative complications, extrahepatic recurrence, and delay of recurrence were less favorable than those of open approach although laparoscopy was performed in patients with a lesser number of cyst (p = 0.065) and with no primary extrahepatic hydatid locations (p = 0.056).
In our series, the location of most peritoneal recurrent cysts was in the lowest down areas of the peritoneum such as areas under the diaphragm, the two paracolic gutters, or the pelvis. This fact was in favor of spillage of hydatid material during the manipulation of the primary hydatid cyst.
In our opinion, the risk of spillage and dissemination of hydatid material in the peritoneum during conservative procedures is probably more important in the laparoscopic than open approach. This higher risk can be explained by the combined effect of two factors. First, in open approach, puncture of the hydatid cyst was made after isolation of the cyst and its surrounding areas from the rest of the abdominal cavity by using gauze swabs soaked by scolicidal solution. This procedure prevents hydatid dissemination in the peritoneum even in case of spillage. However, this precaution is not well feasible in laparoscopy. Secondly, in case of spillage, the effect of pneumoperitoneum insufflation would promote the spread of hydatid material throughout the peritoneal cavity. This was demonstrated by the results of our study in which the precautions used (position of an aspirator near the point of puncture and irrigation of the surrounding areas of the cyst by scolicidal solution) were insufficient. How to deal with these disadvantages? Several devices have been used: Seven et al. [8] utilized a special umbrella trocar which allowed to applying the cyst against the abdominal wall and thus reducing the risk of spillage. This study involved 33 patients with one recurrence after an average follow-up of 17 months. Two surgical teams [9, 15] performed an initial decompression of the cyst with a fine needle and then replaced with equal volume of scolicidal solution to sterilize the cyst. However, as explained by Acarli et al. [16], this technique has two drawbacks. First, the fine needle gets obstructed easily by hydatid membranes or by daughter cysts. Second, as demonstrated by Bickel et al. [17] in their experimental study, puncture of cyst under pressure is often accompanied with spillage even when using a fine needle. Three years later, Bickel et al. [18] developed the isolated hypobaric technique in which all the maneuvers on the cyst were carried out through an assembled transparent cannula with vacuum inside, while its tip adhered firmly to the cyst wall. With this method, the same authors [18] treated 52 hydatid cysts. No recurrence was observed after median postoperative follow-up of 47 months. Finally, using a minimum of 4 weeks of preoperative albendazole treatment would reduce both the viability of the cyst and the intracystic pressure, and therefore, it would reduce the consequences of contamination when spillage occurs [19, 20].
Conclusion
Treatment of the hydatid cyst by laparoscopy must take into account the high risk of spillage of hydatid material and the peritoneal contamination. That is why this approach must be used only in the presence of adapted material and must be associated with preoperative antiparasitic drug treatment.
We need randomized trial comparing laparoscopic to open approach using a new adapted device to aspirate cyst content without the risk of spillage.
References
Sielaff TD, Taylor B, Langer B (2001) Recurrence of hydatid disease. World J Surg 25:83–86
Brunetti E, Kern P, Vuitton DA (2010) Writing panel for the WHO-IWGE. Expert consensus for the diagnosis and treatment of cystic and alveolar echinococcosis in humans. Acta Trop 114:1–16
Akbulut S, Senol A, Sezgin A, Cakabay B, Dursun M, Satici O (2010) Radical vs conservative surgery for hydatid liver cysts. Experience from single center. World J Gastroenterol 16:953–959
Motie MR, Ghaemi M, Aliakbarian M, Saremi E (2010) Study of the radical vs. conservative surgical treatment of the hepatic hydatid cyst: a 10-year experience. Indian J Surg 72:448–452
Dziri C, Haouet K, Fingerhut A (2004) Treatment of hydatid cyst of the liver: where is the evidence? World J Surg 28:731–736
Kapan M, Kapan S, Goksoy E, Perek S, Kol E (2006) Postoperative recurrence in hepatic hydatid disease. J Gastrointest Surg 10:734–739
Prousalidis J, Kosmidis C, Anthimidis G, Kapoutzis K, Karamanlis E, Fachantidis E (2012) Postoperative recurrence of cystic hydatidosis. Can J Surg 55:15–20
Seven R, Berber E, Mercan S, Eminoglu L, Budak D (2000) Laparoscopic treatment of hepatic hydatid cysts. Surgery 128:36–40
Khoury G, Abiad F, Geagea T, Nabout G, Jabbour S (2000) Laparoscopic treatment of hydatid cysts of the liver and spleen. Surg Endosc 14:243–245
Galitza Z, Bazarsky E, Sneier R, Peiser J, El-On J (2006) Repeated treatment of cystic echinococcosis in patients with a long-term immunological response after successful surgical cyst removal. Trans R Soc Trop Med Hyg 100:126–133
Gargouri M, Ben Amor N, Ben Chehida F, Hammou A, Gharbi HA, Ben Cheikh M, Kchouk H, Ayachi K, Golvan JY (1990) Percutaneous treatment of hydatid cysts (Echinococcusgranulosus). Cardiovasc Intervent Radiol 13:169–173
Dziri C, Nouira R (2011) Surgical treatment of liver hydatid disease by laparotomy. J Visc Surg 148:103–110
Dervenis C, Delis S, Avgerinos C, Madariaga J, Milicevic M (2005) Changing concepts in the management of liver hydatid disease. J Gastrointest Surg 9:869–877
Horan TC, Andrus M, Dudeck MA (2008) CDC/NHSN surveillance definition of health care-associated infection and criteria for specific types of infections in the acute care setting. Am J Infect Control 36:309–332
Ramachandran CS, Goel D, Arora V (2001) Laparoscopic surgery in hepatic hydatid cysts: a technical improvement. Surg Laparosc Endosc Percutan Tech 11:14–18
Acarli K (2004) Controversies in the laparoscopic treatment of hepatic hydatid disease. HPB 6:213–221
Bickel A, Daud G, Urbach D, Lefler E, Barasch EF, Eitan A (1998) Laparoscopic approach to hydatid liver cysts. Is it logical? Physical, experimental, and practical aspects. Surg Endosc 12:1073–1077
Bickel A, Loberant N, Singer-Jordan J, Goldfeld M, Daud G, Eitan A (2001) The laparoscopic approach to abdominal hydatid cysts: a prospective nonselective study using the isolated hypobaric technique. Arch Surg 136:789–795
Koea JB (2012) Laparoscopic treatment of hepatic hydatid disease. ANZ J Surg 82:499–504
Koul PA, Singh AA, Ahanger AG, Wahid A, Sofi BA (2010) Optimal duration of preoperative anti-helminthic therapy for pulmonary hydatid surgery. ANZ J Surg 80:354–357
Disclosures
Drs. Hichem Jerraya, Mehdi Khalfallah, Samia Ben Osman, Ramzi Nouira, and Chadli Dziri have no conflict of interest or financial ties to disclose.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Jerraya, H., Khalfallah, M., Osman, S.B. et al. Predictive factors of recurrence after surgical treatment for liver hydatid cyst. Surg Endosc 29, 86–93 (2015). https://doi.org/10.1007/s00464-014-3637-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00464-014-3637-0