Abstract
Background
Single-site laparoscopic colectomy (SLC) is increasingly performed for colon cancer. There are few reports on invasiveness in SLC. This study aimed to evaluate the postoperative pain from SLC, as compared to conventional multiport laparoscopic colectomy (MLC).
Methods
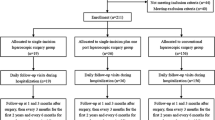
We compared postoperative pain among patients from the SLC group (n = 11) with those from the MLC group (n = 11) who underwent laparoscopic surgery for colon cancer at our institution between May and October 2013. Patients were specifically matched for gender, age, body mass index, tumor size, and performance status. Postoperative pain was evaluated at rest and during mobilization, using a visual analog scale (VAS) on postoperative days (PODs) 1–7, and by postoperative frequency of analgesics; pain intensity was evaluated at rest, using the Pain Vision™ system on PODs 1–7. Other operative outcomes of the two groups were also recorded.
Results
Patient demographics, operative outcomes, time duration before first flatus, and C-reactive protein and WBC count on POD 1 showed no significant differences between groups. Results of sequential VAS during mobilization until POD 7 were significantly less in the SLC group than in the MLC group (p = 0.009). However, sequential VAS at rest did not differ between the two groups (p = 0.11). Measured with the Pain Vision™ system, the difference in pain intensity at rest was statistically significant for the postoperative period (p = 0.003). Total requests for analgesics until POD 7 were reduced in the SLC group compared to that in the MLC group, but lacked statistical significance (three vs. seven, respectively, p = 0.07).
Conclusions
In both quantitative and objective measurements using the Pain Vision™ system, SLC significantly reduced postoperative pain. SLC is a promising procedure, associated with less invasiveness than MLC.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Jacobs et al. [1] performed the first laparoscopic surgery for colorectal cancer (right hemicolectomy) in 1991. Advantages of laparoscopic surgery over conventional open surgery include decreased invasiveness, earlier recovery of postoperative intestinal functions, and shorter hospital stay [2, 3, 4]. In randomized controlled clinical studies of laparoscopic surgery and open surgery for advanced colon cancer, the frequencies of intraoperative and postoperative complications (short-term outcomes) were comparable. In addition, the non-inferiority of laparoscopic surgery, in terms of long-term outcomes, such as overall survival and disease-free survival, was also demonstrated [5, 6, 7]. Furthermore, single-site laparoscopic surgery for low invasiveness and improvement in cosmesis (by eliminating the port on the flank and centralizing wounds of the abdominal wall onto the umbilical region) has attracted attention; single-site laparoscopic surgery has also been gaining in popularity by addressing social needs in the field of gastroenterological surgery.
Due to its success, the application of laparoscopic surgery has been extended. Remzi [8] and Bucher et al. [9], first performed single-site laparoscopic colectomy (SLC) in 2008. Subsequently, reports have shown that SLC is comparable to conventional multiport laparoscopic colectomy (MLC), in terms of short-term outcomes, including safety and oncologic clearance [10, 11].
The surgical instruments and techniques of SLC cause some limitations. Because several forceps gather at the access site, they tend to clash; in addition, because the operator manipulates two straight forceps, which are positioned in parallel to the endoscope, the movement of the operator is limited, and they interfere with the movement of the endoscope. In addition, it is difficult to remove or resect intestines because of insufficient triangulation with the tissue [12]. Although SLC is associated with difficult surgical procedures and great stress for the operator, it is clear that SLC is advantageous for improving cosmesis, and brings patients satisfaction; however, concerns over low invasiveness of SLC, including reduced postoperative pain, have not been clearly demonstrated.
There have been some studies comparing postoperative pain in three-port or two-port with four-port laparoscopic cholecystectomy [13, 14, 15, 16, 17]; in most of these studies, there were no differences in postoperative pain. Several studies, which compared SLC and MLC, reported reduced postoperative pain in SLC [11, 18, 19]. On the other hand, a systematic review showed conflicting views on whether SLC reduces postoperative pain [20]; thus, the evaluation of SLC remains controversial.
The Visual Analog Scale (VAS) [21] is one of the most common methods used for the evaluation of pain. The Numerical Rating Scale and the 4-point Verbal Rating Scale are difficult methods to use for the evaluation of postoperative pain because they cannot distinguish small changes in pain, while VAS can distinguish changes in pain with the highest sensitivity [22]. On the other hand, VAS is a subjective evaluation method of grading the pain, which the patient is currently experiencing, in comparison with the most intense pain that patient has ever experienced [23].
Determination of pain by VAS is associated with a margin of error of about ±20 mm, and at least one report questioned VAS as an appropriate method to measure postoperative pain [24]. The controversy over the low invasiveness of SLC may be caused by the use of different evaluation methods to compare pain, including a variety of factors. Thus, the establishment of an appropriate evaluation method of pain is required.
Recently, a device called Pain Vision™ PS-2100 (Nipro CO., Osaka, Japan), which quantitatively measures the degree of pain using painless electrical stimulation [25, 26], was developed and introduced in clinical practices. In addition to the advantage that Pain Vision™ can evaluate pain in a relatively short time, it can evaluate pain without giving additional pain to patients. In clinical practices, this method has been used in not only studies of chronic pain such as fibromyalgia [27], low back pain due to spondylolisthesis [28] but also that of acute pain caused by the removal of adhesive wound dressing materials [29]. As for abdominal pain, Ota et al. [30] applied Pain Vision™ to pharmacological challenges tests of local anesthetics to compare the pain in patients before and after treatment and reported that Pain Vision™ was a device which enabled a more objective measurement of pain including lower abdominal pain and body pain. These studies have shown that Pain Vision™ is a useful device, which can evaluate pain objectively in various fields. However, there is no report of postoperative acute pain.
In this study, we investigated the invasiveness of SLC, compared with that of MLC, by objectively and quantitatively evaluating pain, using this new device, Pain Vision™, in addition to VAS.
Materials and methods
Study design
We compared the SLC group (n = 11) with the MLC group (n = 11) among patients who underwent laparoscopic surgery for colon cancer at our institution between May and October 2013. Informed consent was received from all patients. Patients were specifically matched by gender, age, body mass index (BMI), tumor size, and performance status (PS). Exclusion criteria were: advanced T4 tumor, perforated tumor or tumor exceeding 60 mm on preoperative evaluations, PS 2 or 3 or 4, severe obesity (defined as a BMI > 35 kg/m2), dementia, previous abdominal polysurgery, indication for an emergency colectomy, and participation refusal.
Outcome
Patient and tumor characteristics data, such as gender, age, BMI, tumor size, and PS, were recorded. Before surgery, all patients were taught how to score pain on the VAS (0 mm, no pain; 100 mm, maximal pain) and measure pain intensity, using the Pain Vision™ system. Surgical data, including operative time, estimated blood loss, length of umbilical incision, number of lymph nodes harvested, and length of resected specimen were also recorded.
Postoperative data focused on the VAS (100 mm) at rest and during mobilization on each postoperative day (POD) 1–7, the Pain Vision™ system for pain intensity at rest on each POD 1–7, postoperative frequency of analgesics, time duration before first flatus, and C-reactive protein and WBC count on POD 1.
Visual analog scale (VAS)
The VAS is a simple and often used method for evaluating variations in pain intensity. Subjects are instructed to indicate the intensity of the pain at rest and during mobilization by marking a 100-mm horizontal line, anchored with “0 (no pain)” at the left edge and “100 (worst imaginable pain)” at the right edge.
Pain vision™
Principle of pain determination
The Pain Vision™ system was developed as a medical device, which can determine pain intensity as a numerical value. The principle of measurement of this system is to compare a unique electrical stimulation with the pain that the patient is experiencing. That is to say, an electrical stimulation without pain, whose intensity is equivalent to that of the pain experienced by the patient, is applied, and the current value of this electrical stimulation is defined as the “pain equivalent current”. The sensitivity (threshold) of the patient for the electrical stimulation is defined as the “minimum perceived current”, which is intended to eliminate variations between individuals.
Using these two values, pain intensity is defined by the following formula:
Pain intensity = (pain equivalent current−minimum perceived current)/minimum perceived current × 100.
Methods of measurement
An electrode is attached to the medial side of the upper arm (Fig. 1). An electrical current is applied (50 Hz; 0–150 μA rms; pulse width: 0.3 ms), and the stimulation is increased. The patient is instructed to press a button when s/he perceives this stimulation for the first time; the current at this point is defined as the “minimum perceived current” value. As the stimulation current is increased, the patient is instructed to press the switch when s/he feels the intensity of the stimulation current is equivalent to that of the pain s/he is experiencing (i.e., when the patient is more annoyed by the stimulation current than by the pain s/he is experiencing), the current at this point is defined as the “pain equivalent current” value. Using the values obtained, “pain intensity” is calculated by the aforementioned formula.
Procedure technique
SLC was introduced to our hospital in 2009 to further improve cosmesis and lower invasiveness, and now the operation technique is routine [11, 31]. In SLC, a small incision of 2.5 cm is first made in the umbilical region, then the multichannel access device, one 12 mm camera port, and two 5 mm instrument ports are inserted, and intra-abdominal manipulation is performed; the final incision is extended as short as possible, depending on the situation, where a specimen is extracted through the mini-laparotomy umbilical incision. In MLC, a small incision of 2.5 cm is made in the umbilical region, and the access device and one 12 mm camera port are inserted into the umbilical region. In addition, one 12 mm port and three 5 mm ports are inserted into the flank. The incision is extended when a specimen is removed, in a manner similar to SLC. In other words, SLC and MLC have the same length of midline wound in the umbilical region.
Statistical analyses
Data were collected and analyzed using JMP 9.0 (SAS Institute Inc.). Numeric data are presented as medians. Continuous variables were compared using the Mann–Whitney U test, whereas categorical variables were compared using Fisher’s exact test. The sequential VAS and pain intensity until POD 7 were analyzed using two-way ANOVA for repeated measures. p values of 0.05 or less were considered statistically significant differences.
Results
The SLC group and the MLC group had similar patient characteristics, regarding gender, age (63 vs. 69 years, respectively, p = 0.45), BMI (23 vs. 22 kg/m2, respectively, p = 0.34), tumor size (30 vs. 30 mm, respectively, p = 0.39), and PS (Table 1).
Operative and perioperative outcomes
The surgical results were compared between the SLC group and the MLC group. Operative time (177 vs. 182 min, respectively, p = 0.82), estimated blood loss (20 vs. 20 mL, respectively, p = 0.95), length of umbilical incision (35 vs. 35 mm, respectively, p = 0.71), number of lymph nodes harvested (26 vs. 21, respectively, p = 0.67), length of resected specimen (270 vs. 265 mm, respectively, p = 0.87), time duration before first flatus (2 vs. 2 days, respectively, p = 0.83), C-reactive protein on POD 1 (2.6 vs. 4.1 mg/dL, respectively, p = 0.18), and WBC count on POD 1 (7760 vs. 7540 per μL, respectively, p = 0.87) were not significantly different between the two groups (Table 2).
Total requests for analgesics until POD 7 were reduced in the SLC group, but the difference between the SLC and MLC group was not statistically significant (three vs. seven, respectively, p = 0.07).
Postoperative pain outcomes
In both the SLC and MLC groups, VAS during mobilization was consistently significantly higher than VAS at rest until POD 7 (Fig. 2). The reduction of postoperative pain during mobilization until POD 7, evaluated by VAS, was significantly greater in the SLC group than that in the MLC group (p = 0.009; two-way ANOVA) (Fig. 3).
For evaluation by VAS at rest, there was a tendency for postoperative pain to be reduced in the SLC group, but no significant difference was observed (p = 0.11; two-way ANOVA) (Fig. 4).
For the quantitative evaluation of pain at rest, using the Pain Vision™ system, pain intensity after surgery in the SLC group was consistently lower than that in the MLC group, and reduction of pain until POD 7 in the SLC group was significantly greater than that in the MLC group (p = 0.003; two-way ANOVA) (Fig. 5). In the MLC group, high pain intensity was observed in the early postoperative period that gradually decreased. In the SLC group, on the other hand, pain intensity did not increase greatly, even in the early postoperative period, and remained at a low level on POD 3 and thereafter.
Discussion
Penetration of laparoscopic surgery has become popular in the field of surgery, due to its extended indication for colon cancer. Compared with open surgery, laparoscopic surgery has demonstrated low invasiveness, as well as several other advantages, including reduction in postoperative pain, earlier recovery of intestinal functions after surgery, and shorter hospital stay [4]. Against the background of increasing social needs for lower invasiveness and improved cosmesis, single-site laparoscopic surgery has gained attention as the ultimate minimally invasive surgery.
Trocars are inserted in laparoscopic surgery. These instruments can increase damage to the abdominal wall, resulting in bleeding from this wall, the abdominal cavity, and the retroperitoneal organs. Additionally, abdominal wall hernia and surgical site infection may occur in the port site. An increasing number of ports are associated with a higher risk of these conditions [32]. Therefore, it would be beneficial for patients to reduce the number of ports, size of the trocars, and incision length as much as possible, to the extent that safety and oncologic clearance would not be compromised.
Oncologic clearance and technical safety are important in the surgical treatment of cancer. In these respects, SLC is similar to MLC, regarding operative time, perioperative blood loss, incidence of complications, the number of lymph nodes harvested, and the length of resected margin, while the feasibility is also maintained to some degree [10, 11, 19, 33, 34]. If cosmesis and low invasiveness are demonstrated, the significance of SLC as a superior technique to MLC will be determined.
This study evaluated pain over seven consecutive days after surgery, employing VAS at rest and during mobilization, as well as Pain Vision™. In previous studies, postoperative pain for SLC has frequently been measured by a pain score on POD 1 [11, 18, 35, 36]. Since patients experience the most intense pain on this day, we can evaluate pain. However, evaluation of temporal changes in pain, when patients eat meals and move their body to use the toilet after leaving their sickbed, enables further comparison and investigation. Thus, we measured pain until POD 7 in this study.
Our data confirmed that pain on the VAS, both at rest and during mobilization, was almost completely resolved by POD 7. By controlling postoperative pain during mobilization, patients can leave their sickbed earlier and discharge the sputum. In addition, this may reduce the incidence of postoperative respiratory complications and the risk of postoperative cardiovascular events [37]. In this study, the VAS pain scores during mobilization showed significantly reduced pain in the SLC group, as compared to those in the MLC group. Since patients experience pain at rest for a long time after surgery, we can prevent nocturnal sleep problems and reduce postoperative dissatisfaction/discomfort by controlling the pain at rest. Although the VAS scores at rest in this study showed a trend toward reduction in postoperative pain for the SLC group, there was no statistically significant difference between the groups.
Wolthuis et al. [38], compared postoperative pain using “pain scores”, such as VAS, between the SLC (14 patients) and MLC (14 patients) groups. Similarly, Chew et al. [35], compared postoperative pain between the SLC (40 patients) and MLC (104 patients) groups. Both studies reported similar intensities of pain between both groups. On the contrary, Takemasa et al. [11], evaluated the feasibility of the SLC group (150 patients) compared with the MLC group (150 patients), and reported that VAS scores on POD 1 were significantly lower in the SLC group than in the MLC group. Champagne et al. [18], also compared postoperative pain between the SLC (165 patients) and MLC (165 patients) groups, and reported a significant reduction in postoperative pain in the SLC group. These results suggest that studies using larger sample sizes demonstrate higher reliability of pain scores, such as VAS.
Since our study involved comparison using a smaller number of patients (11 patients in the SLC group and 11 patients in the MLC group), we did not observe a significant difference in the VAS scores at rest, despite case-matching patient characteristics and operative factors. Thus, we measured the scores of pain at rest using Pain Vision™, which quantitatively and objectively evaluates pain. As a result, we confirmed that the SLC group showed a significant reduction in postoperative pain, as compared with the MLC group. This indicates that, given the equivalent length of umbilical incision between both groups, the lateral port sites in the abdominal wall may be responsible for the difference in postoperative pain. By reducing early postoperative pain of the highest intensity, we may minimize anxiety or fear relating to body movement, and, in turn, patients may be able to leave their sickbeds without trouble sooner, and possibly accelerate postoperative recovery. These results provide evidence supporting the low invasiveness of SLC.
Prior to Pain Vision™, Pain Matcher® (Cefar Medical AB, Lund, Sweden), which compared the intensity of pain with that of pain that is artificially produced by applying stimulation to the skin, was developed [39]. However, such electrical stimulation on the skin may damage tissue in some way [40], and it is impractical to make patients experience additional pain. Another disadvantage of Pain Matcher® is its inability to measure the threshold level of pain in subjects.
Based on the results of our study, we confirmed, in the smaller number of patients, that, while subjective evaluation based on the VAS scores revealed no difference, quantitative evaluation, employing Pain Vision™, showed a significant reduction of postoperative pain in the SLC group, as compared to that in the MLC group. However, there remain some limitations of this study. First, Pain Vision™ cannot evaluate pain during mobilization, which is an important measure of postoperative pain. Second, it takes time for patients to get accustomed to Pain Vision™, because it is slightly complicated and not straightforward. Thus, it may be difficult to introduce Pain Vision™ as routine protocol in clinical practices. Third, this study was a case control study in a smaller number of patients. A prospective randomized controlled trial, involving a larger number of patients, would provide greater significance.
We confirmed that SLC not only controls pain during mobilization, but it also reduces pain at rest. These advantages of SLC are in addition to its apparent superiority over MLC, regarding cosmesis. This study provides additional evidence to support the low invasiveness of SLC by evaluating pain, using Pain Vision™. Thus, SLC may be a promising procedure with many advantages for patients.
In conclusion, using the quantitative and objective measurements, employed by the Pain Vision™ system, we show that SLC significantly reduces postoperative pain for a selected group of patients, in comparison to MLC. These results support that SLC is less invasive. Larger-scale, prospective studies are required to confirm our results.
References
Jacobs M, Verdeja JC, Goldstein HS (1991) Minimally invasive colon resection (laparoscopic colectomy). Surg Laparosc Endosc 1:144–150
Veldkamp R, Kuhry E, Hop WC, Jeekel J, Kazemier G, Bonjer HJ, Haglind E, Pahlman L, Cuesta MA, Msika S, Morino M, Lacy AM (2005) Laparoscopic surgery versus open surgery for colon cancer: short-term outcomes of a randomised trial. Lancet Oncol 6:477–484
Schwenk W, Haase O, Neudecker J, Muller JM (2005) Short term benefits for laparoscopic colorectal resection. Cochrane Database Syst Rev 20(3):CD003145
Tjandra JJ, Chan MK (2006) Systematic review on the short-term outcome of laparoscopic resection for colon and rectosigmoid cancer. Colorectal Dis 8:375–388
Fleshman J, Sargent DJ, Green E, Anvari M, Stryker SJ, Beart RW, Hellinger M Jr, Flanagan R Jr, Peters W, Nelson H (2007) Laparoscopic colectomy for cancer is not inferior to open surgery based on 5 year data from the COST Study Group trial. Ann Surg 246:655–662; discussion 662–654
Buunen M, Veldkamp R, Hop WC, Kuhry E, Jeekel J, Haglind E, Pahlman L, Cuesta MA, Msika S, Morino M, Lacy A, Bonjer HJ (2009) Survival after laparoscopic surgery versus open surgery for colon cancer: long-term outcome of a randomised clinical trial. Lancet Oncol 10:44–52
Jayne DG, Thorpe HC, Copeland J, Quirke P, Brown JM, Guillou PJ (2010) Five-year follow-up of the Medical Research Council CLASICC trial of laparoscopically assisted versus open surgery for colorectal cancer. BJS 97:1638–1645
Remzi FH, Kirat HT, Kaouk JH, Geisler DP (2008) Single-port laparoscopy in colorectal surgery. Colorectal Dis 10:823–826
Bucher P, Pugin F, Morel P (2008) Single port access laparoscopic right hemicolectomy. Int J Colorectal Dis 23:1013–1016
Kim SJ, Ryu GO, Choi BJ, Kim JG, Lee KJ, Lee SC, Oh ST (2011) The short-term outcomes of conventional and single-port laparoscopic surgery for colorectal cancer. Ann Surg 254:933–940
Takemasa I, Uemura M, Nishimura J, Mizushima T, Yamamoto H, Ikeda M, Sekimoto M, Doki Y, Mori M (2013) Feasibility of single-site laparoscopic colectomy with complete mesocolic excision for colon cancer: a prospective case-control comparison. Surg endosc 28(4):1110–1118
Leblanc F, Champagne BJ, Augestad KM, Stein SL, Marderstein E, Reynolds HL, Delaney CP (2010) Single incision laparoscopic colectomy: technical aspects, feasibility, and expected benefits. Diagn Ther Endosc 2010:913216
Trichak S (2003) Three-port vs standard four-port laparoscopic cholecystectomy. Surg Endosc 17:1434–1436
Poon CM, Chan KW, Lee DW, Chan KC, Ko CW, Cheung HY, Lee KW (2003) Two-port versus four-port laparoscopic cholecystectomy. Surg Endosc 17:1624–1627
Gupta A, Shrivastava UK, Kumar P, Burman D (2005) Minilaparoscopic versus laparoscopic cholecystectomy: a randomised controlled trial. Trop Gastroenterol 26:149–151
Kumar M, Agrawal CS, Gupta RK (2007) Three-port versus standard four-port laparoscopic cholecystectomy: a randomized controlled clinical trial in a community-based teaching hospital in eastern Nepal. JSLS 11:358–362
Cerci C, Tarhan OR, Barut I, Bulbul M (2007) Three-port versus four-port laparoscopic cholecystectomy. Hepatogastroenterology 54:15–16
Champagne BJ, Papaconstantinou HT, Parmar SS, Nagle DA, Young-Fadok TM, Lee EC, Delaney CP (2012) Single-incision versus standard multiport laparoscopic colectomy: a multicenter, case-controlled comparison. Ann Surg 255:66–69
Poon JT, Cheung CW, Fan JK, Lo OS, Law WL (2012) Single-incision versus conventional laparoscopic colectomy for colonic neoplasm: a randomized, controlled trial. Surg Endosc 26:2729–2734
Fung AK, Aly EH (2012) Systematic review of single-incision laparoscopic colonic surgery. BJS 99:1353–1364
McCormack HM, Horne DJ, Sheather S (1988) Clinical applications of visual analogue scales: a critical review. Psychol Med 18:1007–1019
Seymour RA (1982) The use of pain scales in assessing the efficacy of analgesics in post-operative dental pain. Eur J Clin Pharmacol 23:441–444
Babul N, Darke AC, Johnson DH, Charron-Vincent K (1993) Using memory for pain in analgesic research. Ann Pharmacother 27:9–12
DeLoach LJ, Higgins MS, Caplan AB, Stiff JL (1998) The visual analog scale in the immediate postoperative period: intrasubject variability and correlation with a numeric scale. Anesth Analg 86:102–106
Jefferson JK (1998) Electrodiagnostic functional sensory evaluation of the patient with pain: a review of the neuroselective current perception threshold and pain tolerance threshold. Pain Digest 8:219–230
Shimazu H, Kobayashi H, Seno S, Kato S, Akimoto M, Aizawa S et al (2004) Quantitative Analysis of the Degree of Pain Using Pain-less Electrical Stimuli. 11th International Pain Clinic World Society of Pain Clinicians 451–455
Osada K, Oka H, Isomura T, Nakamura I, Tominaga K, Takahashi S, Kojima A, Nishioka K (2011) Development of the Japanese version of the fibromyalgia impact questionnaire (JFIQ): psychometric assessments of reliability and validity. Int J Rheum dis 14:74–80
Lee HJ, Seo JC, Kwak MA, Park SH, Min BM, Cho MS, Shin I, Jung JY, Roh WS (2014) Acupuncture for low back pain due to spondylolisthesis: study protocol for a randomized controlled pilot trial. Trials 15:105
Matsumura H, Imai R, Gondo M, Watanabe K (2012) Evaluation of pain intensity measurement during the removal of wound dressing material using ‘the PainVision system’ for quantitative analysis of perception and pain sensation in healthy subjects. Int Wound J 9:451–455
Ota S, Ogawa K, Shimbori H, Oki H, Nakahashi Y, Goto T (2009) Application quantitative measurement device for perception and pain (Pain Vision) to pharmacological challenges. Pain Clin 30:209–214
Takemasa I, Sekimoto M, Ikeda M, Mizushima T, Yamamoto H, Doki Y, Mori M (2010) Video. Transumbilical single-incision laparoscopic surgery for sigmoid colon cancer. Surg Endosc 24:2321
Makino T, Milsom JW, Lee SW (2012) Feasibility and safety of single-incision laparoscopic colectomy: a systematic review. Ann Surg 255:667–676
Papaconstantinou HT, Sharp N, Thomas JS (2011) Single-incision laparoscopic right colectomy: a case-matched comparison with standard laparoscopic and hand-assisted laparoscopic techniques. J Am Coll Surg 213:72–80; discussion 80–72
Chen WT, Chang SC, Chiang HC, Lo WY, Jeng LB, Wu C, Ke TW (2011) Single-incision laparoscopic versus conventional laparoscopic right hemicolectomy: a comparison of short-term surgical results. Surg Endosc 25:1887–1892
Chew MH, Chang MH, Tan WS, Wong MT, Tang CL (2013) Conventional laparoscopic versus single-incision laparoscopic right hemicolectomy: a case cohort comparison of short-term outcomes in 144 consecutive cases. Surg Endosc 27:471–477
Lu CC, Lin SE, Chung KC, Rau KM (2012) Comparison of clinical outcome of single-incision laparoscopic surgery using a simplified access system with conventional laparoscopic surgery for malignant colorectal disease. Colorectal Dis 14:e171–e176
Moraca RJ, Sheldon DG, Thirlby RC (2003) The role of epidural anesthesia and analgesia in surgical practice. Ann Surg 238:663–673
Wolthuis AM, Penninckx F, Fieuws S, D’Hoore A (2012) Outcomes for case-matched single-port colectomy are comparable with conventional laparoscopic colectomy. Colorectal Dis 14:634–641
Stener-Victorin E, Kowalski J, Lundeberg T (2002) A new highly reliable instrument for the assessment of pre- and postoperative gynecological pain. Anesth Analg 95:151–157, table of contents
Lahoda R, Stacher G, Bauer P (1977) Experimentally induced pain: measurement of pain threshold and pain tolerance using a new apparatus for electrical stimulation of the skin. Int J Clin Pharmacol Biopharm 15:51–56
Disclosures
The authors have declared that they have no competing interests.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Hiraki, M., Takemasa, I., Uemura, M. et al. Evaluation of invasiveness in single-site laparoscopic colectomy, using “the PainVision™ system” for quantitative analysis of pain sensation. Surg Endosc 28, 3216–3223 (2014). https://doi.org/10.1007/s00464-014-3594-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00464-014-3594-7