Abstract
Background
Several studies have assessed feasibility and early outcomes of the laparoscopic approach for complicated appendicitis (CA). However, these studies suffer from limitations due to the heterogeneous definitions used for CA. No studies have assessed feasibility and early post-operative outcomes of the laparoscopic approach in the specific management of diffuse appendicular peritonitis (DAP). Consequently, outcomes of the laparoscopic approach for the management of DAP are poorly documented.
Methods
The laparoscopic approach is the first-line standardised procedure used by our team for the management of DAP. All patients (aged >16 years) who underwent laparoscopy for DAP (CA with the presence of purulent fluid with or without fibrin membranes in at least a hemi abdomen) between 2004 and 2012 were prospectively included. Post-operative outcomes were analysed according to the Clavien–Dindo classification.
Results
Laparoscopy for DAP was performed for 141 patients. Mean age was 39.6 ± 20 (16–92) years. A total of 45 patients (31.9 %) had pre-operative contracture. The mean pre-operative leukocyte count was 14,900 ± 4,380 mm−3. The mean pre-operative C-reactive protein (CRP) serum concentration was 135 ± 112 (2–418) mg/dl. The conversion rate was 3.5 %. The mean operative time was 80 ± 27 (20–180) min. There were no deaths. The rate of grade III morbidity was 6.5 %. Ten patients (7.1 %) experienced intra-abdominal abscess (IAA); seven of these cases were treated conservatively. The mean length of hospital stay was 6.9 ± 5 (2–36) days. A pre-operative leukocyte count >17,000 mm−3, and CRP serum concentration >200 mg/dl were significant predictive factors for IAA in multivariate analyses [odds ratio (OR) 25.0, 95 % confidence interval (CI) 2.4–250, p = 0.007 and OR 16.4, 95 % CI 1.6–166, p = 0.02, respectively].
Conclusion
The laparoscopic approach for DAP is a safe and feasible procedure with a low conversion rate and an acceptable rate of IAA in view of the severity of the disease. Pre-operative leukocyte counts >17,000 mm−3 and pre-operative CRP serum concentrations >200 mg/dl indicate a high risk of IAA.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
About 71,245 patients underwent surgery for acute appendicitis (AA) in France in 2012 [1]; 38 % presented with a complicated disease defined as localised (27 %) or diffuse (11 %) peritonitis. The vast majority of these patients (84 % for uncomplicated appendicitis [UA] and 75 % for complicated appendicitis [CA]) were operated on via a laparoscopic approach. A European multicentre observational study over the same period reported that 30 % of AA patients presented with diffuse appendicular peritonitis (DAP) and only 49 % of these patients were treated via a laparoscopic approach [2]. This suggests heterogeneity in surgical approaches and indicates that laparoscopic surgery has not become the standard approach to the management of CA.
The first description of laparoscopic appendectomy was published by Semm [3] in 1983, and this approach was rapidly accepted as an adequate option for UA. However, initial reports of a laparoscopic approach in CA described a conversion rate of 25 % [4] and a higher rate of post-operative intra-abdominal abscess (IAA) (26 %) than with the conventional open approach (OA) [5].
Recently, a retrospective observational study [6] and a meta-analysis of retrospective case control studies [7], in contradiction with previous reports, suggested that the laparoscopic approach was more effective than the OA for the management of CA, with lower morbidity [6] and lower rates of surgical site infection [7] with no higher risk of IAA. In a large recent retrospective study of CA operated on via a laparoscopic approach, Asarias et al. [8] found a rate of IAA of 5.9 %. IAA increases the length of hospital stay and may lead to re-operation, therefore, the prevention and management of IAA remain significant challenges. Twenty years later, the laparoscopic experience has increased such that updated trials evaluating the laparoscopic approach for CA are warranted.
However, in these recent studies, the term ‘CA’ is used for a broad and heterogeneous spectrum of anatomo-clinical conditions (appendix gangrenous and/or perforated, localized or diffuse peritonitis). The post-operative courses of these different situations, and especially DAP—which is the most severe form of CA—could differ substantially.
No study has specifically assessed early post-operative outcomes following the management of DAP with a laparoscopic approach. The purpose of this study was therefore to assess the feasibility and early post-operative outcomes of DAP management with a laparoscopic approach and to determine risk factors for post-operative IAA.
Methods
From January 2004 to December 2012, 141 patients (16 years old or older) underwent a laparoscopic approach for DAP. No patients with DAP had OA as first intention. To identify DAP clearly among cases of CA, we used a strict per-operative definition for DAP: perforated or gangrenous appendicitis with the presence of purulent collections with or without fibrin membranes in at least a hemi-abdomen (necessarily including the pelvis, peri-appendicular and right diaphragmatic areas).
We conducted a retrospective chart review of a prospective database registered with the French national data protection agency (the Commission nationale de l’informatique et des libertés [CNIL], N°1693525) as required by law to ensure patient welfare and correct ethical behaviour. The data collected included pre-operative factors (age, sex, duration of symptoms, clinical exam findings, radiological results and laboratory values), per-operative factors (length of procedure, conversion to OA, number of drains, peritoneal cavity irrigation, method used for stump ligation) and post-operative factors (length of hospital stay, mortality, rehospitalisation and all post-operative events during the 30 days following the intervention). C-reactive protein (CRP) testing is not routinely conducted in emergency situations; consequently, these data are missing for 27 patients.
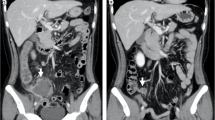
Patients were operated on by a single team in a tertiary care centre. Since 2000, our team has used laparoscopy as the first intention approach for all cases of AA (UA and CA). A standardised operative technique was used for all patients with DAP: it involved an umbilical OA to establish the pneumoperitoneum. In addition to the 10-mm optical trocar, two trocars were used: 5 mm in the suprapubic position and 5 or 10 mm in the left mid-abdomen. A 5-mm supplementary trocar was placed, if required, in the right upper quadrant of the abdomen to facilitate per-operative intra-peritoneal irrigation with saline. The base of the appendix was closed with an Endoloop® (Ethicon, Endo-Surgery, Inc.) or with a linear stapler in cases of inflamed or necrotized caecum. Bacteriological samples were collected from all cases. Peritoneal toilet with saline serum lavage or compress was systematic to obtain a clear abdominal cavity at the end of the operation. All specimens were retrieved using a bag and sent for anatomo-pathological examination. Closed-suction drains were used at the individual surgeon’s discretion. Antibiotic treatment (amoxicillin/clavulanic acid or fluoroquinolone with metronidazol in cases of allergy) was started at anaesthesia induction and continued for 5 days for all patients. Thereafter, antibiotherapy was adapted to antibiogram results as appropriate. All patients with abnormal post-operative courses underwent a computed tomography (CT) scan to diagnose IAA. Depending on the size and localisation of the IAA on CT scan, antibiotic treatment (abscess <5 cm) or percutaneous/surgical drainage (abscess >5 cm) was used.
Post-operative complications were graded according to the Clavien–Dindo classification [9].
The XLSTAT® 2013 program (Addinsoft®, New York, NY, USA) for Windows was used for statistical analysis. Nominal variables are presented as percentages, and continuous data are reported as mean ± standard errors of the mean. Since risk factors for IAA in cases of DAP have never been previously studied, we selected the third quartile values of CRP concentrations and leukocyte counts as cut-off values. We used χ 2 tests and Fisher exact tests for categorical variables as appropriate. For numerical variables, Student’s t-tests were performed. To assess risk factors for IAA, univariate and multivariate logistic regressions were performed, including age, sex and all factors with a p value <0.2 in univariate analyses. The significance threshold was set at p = 0.05.
Results
Between 2004 and 2012, a total of 900 laparoscopic appendectomies were performed and 141 (15.7 %) patients had a per-operative diagnosis of DAP.
Mean age at time of operation was 39.6 ± 20 (16–92) years; 44.0 % were women. Contracture and fever >38 °C were present in 45 (31.9 %) and 83 (58.9 %) patients, respectively. Pre-operative radiological investigations confirmed the diagnosis of appendicitis for 135 patients (95.7 %; 130 CT scans and five abdominal ultrasound scans). The mean leukocyte count was 14,900 ± 4,380 mm−3 (3,400–38,000). The mean CRP concentration (available for 114 patients) was 135 ± 112 mg/dl (2–418) (Table 1). Third quartiles for leukocyte counts and serum CRP concentrations were 17,000 mm−3 and 200 mg/dl, respectively.
Five (3.5 %) patients required a conversion to an open procedure (one for morbid obesity, two for extensive inflammatory adhesions and two for reasons associated with anaesthesia). A total of 19 (13.5 %) patients underwent linear stapler resection of the caecum. Closed-suction drains were used in 124 patients (87.9 %); the mean operative time was 80 ± 27 (20–180) min, and mean length of hospital stay was 6.9 ± 5 (2–36) days.
According to the Clavien–Dindo classification [9], nine patients (6.5 %) had grade III and two (1.4 %) had grade IV complications. Ten (7.1 %) patients experienced post-operative IAA; seven of these cases did not require reoperation, and the initial treatment for IAA was successful in all cases. Details of post-operative complications (IIA and Clavien–Dindo grade ≥III) are listed in Table 2. There were no deaths. The 30-day readmission rate was 4.3 % (N = 6).
Univariate analyses and multivariate analyses identified only leukocyte count >17,000 mm−3 (odds ratio [OR] 25.0, 95 % confidence interval [CI] 2.4–250, p = 0.007) and serum CRP concentration >200 mg/dl (OR 16.4, 95 % CI 1.6–166, p = 0.02) as predictive factors for post-operative IAA (Table 3).
Discussion
Since the first description by Semm [3] in 1983, the laparoscopic approach has been increasingly used for AA. The initial reports concerning the laparoscopic approach for CA or UA gave poor results, with higher post-operative morbidity, particularly a higher risk of post-operative IAA [4, 5, 10, 11] than open appendectomies. Despite these poor results and because of its theoretical advantages, the use of the laparoscopic approach for AA has continued to increase and it is now widely performed [2, 12]. Recent observational or randomised studies indicate significant benefits for the laparoscopic approach compared with the OA for UA [6, 13, 14] and also for CA [6, 7, 15, 16] in terms of length of hospital stay, morbidity and wound abscess.
In most studies, AA is divided into two groups: UA and CA. However, the reported series assessing the laparoscopic approach for CA uses heterogeneous definitions of CA; it has been defined according to per-operative status (gangrenous/perforated appendicitis with one abscess [17] or with/without localised/diffuse peritonitis [15, 18–20] ) or histological findings (gangrenous or perforated appendicitis with histological peritonitis) irrespective of per-operative reports [21–24] and according to the International Classification of Diseases, Ninth Revision, Clinical Modification (ICD-9-CM) of a health system database (codes 540.0 and 540.01: perforated appendicitis) [6]. Some series excluded DAP from their analysis [25, 26] and there is no consensus definition for DAP in the literature. Only Navez et al. [4] reported outcomes of the laparoscopic approach for DAP (gangrenous/perforated appendicitis with purulent fluid in two or more quadrants of the abdomen). However, this study suffers from limitations: a small cohort (N = 32), a high conversion rate (25 %) and use of ‘reverse laparoscopy’ (conversion of a McBurney incision to a laparoscopic approach).
In our study, we used a strict peri-operative definition, consequently excluding from our sample patients with localised peritonitis (pus either in the peri-appendicular area or in the sac of Douglas) as reported in other series [4, 18, 25, 27].
As our paper is, to our knowledge, the first report of a large study of DAP treated with a laparoscopic approach, comparison with previous studies is difficult. The pre-operative characteristics of patients are more severe than in previous reports evaluating CA [28, 29].
The low rate of conversion in our experience is comparable to published values. In the literature, reported conversion rates after a laparoscopic approach for CA varies from 1.7 to 39 % [21]. Our mean operative time is longer than that reported by Cueto et al. [27] with their experience in 1,017 CA cases. This difference is probably due to the time required for peritoneal lavage and insertion of drainage. There is no consensus on the necessity for lavage and drainage after appendectomies for CA. Allemann et al. [25] do not recommend routine drainage in a laparoscopic approach for CA. St Peter et al. [30] found no advantage for irrigation of the peritoneal cavity over suction alone during LA for perforated appendicitis in children. However, these studies excluded cases of DAP, and as peritoneal lavage and drainage were not found by univariate analysis to be risk factors for IAA in our study, we still recommend their use.
CA is a risk factor for increased post-operative morbidity [6, 8, 31] and (according to Asarias et al. [8]) for IAA with an OR of 6.1 (95 % CI 3.4–11.1, p < 0.01). The rate of IAA in our series of 141 DAP (excluding all other CA) was 7.2 %. No other study has reported or assessed risk factors for IAA after a laparoscopic approach with DAP. In the literature, the reported rates of IAA for all types of CA vary from 2.8 to 14 % [8, 15, 16, 20, 27]. The limitations of our study include that it was a retrospective review of a prospective database, and the large CI for our OR could be explained by the rarity of IAA in our study population. Multivariate analyses identified pre-operative leukocyte counts >17,000 mm−3 and serum CRP concentrations >200 mg/dl as significant predictive risk factors for IAA. This suggests that surgeons should be warned about the risk of IAA after a laparoscopic approach for DAP in patients presenting with values above these cut-offs.
Occurrence of IAA often requires intravenous antibiotherapy and lengthens the hospital stay. Hence, the mean length of stay of our patients was higher than that in other large previous studies of CA [6, 27]. However, with reference to other studies assessing only CA, our results, including a low conversion rate, and acceptable grade III complication and IAA rates, suggest that the laparoscopic approach for DAP is feasible and safe.
Conclusion
Our study assessed the feasibility and safety of the laparoscopic approach for DAP and we recommend it in these situations. Surgeons and patients should be aware of the risk of post-operative IAA if the pre-operative leukocyte count is higher than 17,000 mm−3 and/or the serum CRP concentration is >200 mg/dl. Prospective randomized studies are needed for rigorous comparison of the laparoscopic approach and the OA for the management of DAP.
References
Agence Technique de l’Information sur l’Hospitalisation (ATIH). French medicare database source
Sartelli M, Catena F, Ansaloni L, Leppaniemi A, Taviloglu K, van Goor H, Viale P, Lazzareschi DV, de Werra C, Marrelli D, Colizza S, Scibe R, Alis H, Torer N, Navarro S, Catani M, Kauhanen S, Augustin G, Sakakushev B, Massalou D, Pletinckx P, Kenig J, Di Saverio S, Guercioni G, Rausei S, Laine S, Major P, Skrovina M, Angst E, Pittet O, Gerych I, Tepp J, Weiss G, Vasquez G, Vladov N, Trana C, Vettoretto N, Delibegovic S, Dziki A, Giraudo G, Pereira J, Poiasina E, Tzerbinis H, Hutan M, Vereczkei A, Krasniqi A, Seretis C, Diaz-Nieto R, Mesina C, Rems M, Campanile FC, Agresta F, Coletta P, Uotila-Nieminen M, Dente M, Bouliaris K, Lasithiotakis K, Khokha V, Zivanovic D, Smirnov D, Marinis A, Negoi I, Ney L, Bini R, Leon M, Aloia S, Huchon C, Moldovanu R, de Melo RB, Giakoustidis D, Ioannidis O, Cucchi M, Pintar T, Jovine E (2012) Complicated intra-abdominal infections in Europe: preliminary data from the first three months of the CIAO Study. World J Emerg Surg 7:15
Semm K (1983) Endoscopic appendectomy. Endoscopy 15:59–64
Navez B, Delgadillo X, Cambier E, Richir C, Guiot P (2001) Laparoscopic approach for acute appendicular peritonitis: efficacy and safety: a report of 96 consecutive cases. Surg Laparosc Endosc Percutan Tech 11:313–316
Frazee RC, Bohannon WT (1996) Laparoscopic appendectomy for complicated appendicitis. Arch Surg 131:509–511 discussion 511–503
Tiwari MM, Reynoso JF, Tsang AW, Oleynikov D (2011) Comparison of outcomes of laparoscopic and open appendectomy in management of uncomplicated and complicated appendicitis. Ann Surg 254:927–932
Markides G, Subar D, Riyad K (2010) Laparoscopic versus open appendectomy in adults with complicated appendicitis: systematic review and meta-analysis. World J Surg 34:2026–2040
Asarias JR, Schlussel AT, Cafasso DE, Carlson TL, Kasprenski MC, Washington EN, Lustik MB, Yamamura MS, Matayoshi EZ, Zagorski SM (2011) Incidence of postoperative intraabdominal abscesses in open versus laparoscopic appendectomies. Surg Endosc 25:2678–2683
Clavien PA, Barkun J, de Oliveira ML, Vauthey JN, Dindo D, Schulick RD, de Santibanes E, Pekolj J, Slankamenac K, Bassi C, Graf R, Vonlanthen R, Padbury R, Cameron JL, Makuuchi M (2009) The Clavien–Dindo classification of surgical complications: five-year experience. Ann Surg 250:187–196
Sauerland S, Lefering R, Neugebauer EA (2002) Laparoscopic versus open surgery for suspected appendicitis. Cochrane Database Syst Rev 1:CD001546
Katkhouda N, Mason RJ, Towfigh S, Gevorgyan A, Essani R (2005) Laparoscopic versus open appendectomy: a prospective randomized double-blind study. Ann Surg 242:439–448 discussion 448–450
Masoomi H, Mills S, Dolich MO, Ketana N, Carmichael JC, Nguyen NT, Stamos MJ (2011) Comparison of outcomes of laparoscopic versus open appendectomy in adults: data from the Nationwide Inpatient Sample (NIS), 2006–2008. J Gastrointest Surg 15:2226–2231
Sauerland S, Jaschinski T, Neugebauer EA (2010) Laparoscopic versus open surgery for suspected appendicitis. Cochrane Database Syst Rev 10:CD001546
Ohtani H, Tamamori Y, Arimoto Y, Nishiguchi Y, Maeda K, Hirakawa K (2012) Meta-analysis of the results of randomized controlled trials that compared laparoscopic and open surgery for acute appendicitis. J Gastrointest Surg 16:1929–1939
Dimitriou I, Reckmann B, Nephuth O, Betzler M (2013) Single institution’s experience in laparoscopic appendectomy as a suitable therapy for complicated appendicitis. Langenbecks Arch Surg 398:147–152
Sleem R, Fisher S, Gestring M, Cheng J, Sangosanya A, Stassen N, Bankey P (2009) Perforated appendicitis: is early laparoscopic appendectomy appropriate? Surgery 146:731–737 discussion 737–738
Kirshtein B, Bayme M, Domchik S, Mizrahi S, Lantsberg L (2007) Complicated appendicitis: laparoscopic or conventional surgery? World J Surg 31:744–749
Katsuno G, Nagakari K, Yoshikawa S, Sugiyama K, Fukunaga M (2009) Laparoscopic appendectomy for complicated appendicitis: a comparison with open appendectomy. World J Surg 33:208–214
Lin YM, Hsieh CH, Cheng CI, Tan BL, Liu HT (2012) Laparoscopic appendectomy for complicated acute appendicitis does not result in increased surgical complications. Asian J Surg 35:113–116
Pokala N, Sadhasivam S, Kiran RP, Parithivel V (2007) Complicated appendicitis—is the laparoscopic approach appropriate? A comparative study with the open approach: outcome in a community hospital setting. Am Surg 73:737–741 discussion 741–732
Mancini GJ, Mancini ML, Nelson HS Jr (2005) Efficacy of laparoscopic appendectomy in appendicitis with peritonitis. Am Surg 71:1–4 discussion 4–5
Kang KJ, Lim TJ, Kim YS (2000) Laparoscopic appendectomy is feasible for the complicated appendicitis. Surg Laparosc Endosc Percutan Tech 10:364–367
Lim SG, Ahn EJ, Kim SY, Chung IY, Park JM, Park SH, Choi KW (2011) A clinical comparison of laparoscopic versus open appendectomy for complicated appendicitis. J Korean Soc Coloproctol 27:293–297
Ball CG, Kortbeek JB, Kirkpatrick AW, Mitchell P (2004) Laparoscopic appendectomy for complicated appendicitis: an evaluation of postoperative factors. Surg Endosc 18:969–973
Allemann P, Probst H, Demartines N, Schäfer M (2011) Prevention of infectious complications after laparoscopic appendectomy for complicated acute appendicitis–the role of routine abdominal drainage. Langenbecks Arch Surg 396:63–68
Yau KK, Siu WT, Tang CN, Yang GP, Li MK (2007) Laparoscopic versus open appendectomy for complicated appendicitis. J Am Coll Surg 205:60–65
Cueto J, D’Allemagne B, Vazquez-Frias JA, Gomez S, Delgado F, Trullenque L, Fajardo R, Valencia S, Poggi L, Balli J, Diaz J, Gonzalez R, Mansur JH, Franklin ME (2006) Morbidity of laparoscopic surgery for complicated appendicitis: an international study. Surg Endosc 20:717–720
Wu JY, Chen HC, Lee SH, Chan RC, Lee CC, Chang SS (2012) Diagnostic role of procalcitonin in patients with suspected appendicitis. World J Surg 36:1744–1749
Andersson RE, Hugander A, Ravn H, Offenbartl K, Ghazi SH, Nystrom PO, Olaison G (2000) Repeated clinical and laboratory examinations in patients with an equivocal diagnosis of appendicitis. World J Surg 24:479–485 discussion 485
St Peter SD, Adibe OO, Iqbal CW, Fike FB, Sharp SW, Juang D, Lanning D, Murphy JP, Andrews WS, Sharp RJ, Snyder CL, Holcomb GW, Ostlie DJ (2012) Irrigation versus suction alone during laparoscopic appendectomy for perforated appendicitis: a prospective randomized trial. Ann Surg 256:581–585
Reid RI, Dobbs BR, Frizelle FA (1999) Risk factors for post-appendicectomy intra-abdominal abscess. Aust N Z J Surg 69:373–374
Disclosure
Jérémie Thereaux, Nicolas Veyrie, Nicola Corigliano, Stéphane Servajean, Sébastien Czernichow and Jean-Luc Bouillot have no conflicts of interest or financial ties to disclose.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Thereaux, J., Veyrie, N., Corigliano, N. et al. Is laparoscopy a safe approach for diffuse appendicular peritonitis? Feasibility and determination of risk factors for post-operative intra-abdominal abscess. Surg Endosc 28, 1908–1913 (2014). https://doi.org/10.1007/s00464-013-3412-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00464-013-3412-7