Abstract
Background
Endoscopic thoracic sympathectomy has been used successfully in the treatment of blushing, excessive sweating, and social phobia. However, the adverse effects of endoscopic thoracic sympathectomy are more severe and frequent than the adverse effects of endoscopic sympathetic block (ESB). The use of different blocking levels for different indications in ESB according to the Lin-Telaranta classification further decreases the postoperative adverse effects. However, there are few data on the long-term results of ESB performed using the Lin-Telaranta classification.
Methods
Ninety-five patients (55 men, 40 women) were interviewed by before the surgery using our routine questionnaire, and the same questionnaire was answered postoperatively by the patients. In addition, a long-term follow-up questionnaire was sent to all patients whose address was known. Forty-seven patients (24 men, 23 women) answered to this questionnaire. The Davidson brief social phobia scale and the Liebowitz quality of life scale were used. Patients were divided to 3 categories: category 1, patients with sweating problems; category 2, patients with blushing; and category 3, and patients with symptoms other than sweating or blushing.
Results
Among patients in category 1, social phobia decreased from 12.43 to 6.71 (p = 0.004), in category 2 from 13.97 to 7.69 (p < 0.001), and in category 3 from 13.18 to 9.64 (p = 0.007) during long-term follow-up. Among patients with severe sweating problems preoperatively, sweating decreased from 2.50 to 1.29 (p = 0.003) among patients in category 1 and from 1.86 to 1.16 (p < 0.001) among patients in category 2. Among patients with unbearable blushing, blushing decreased from 4 to 1.80 (p < 0.001).
Conclusions
Patients got a clear help from ESB performed using the Lin-Telaranta classification to treat blushing, excessive sweating, and social phobia with and without physical symptoms. In addition, compensatory sweating increased only slightly.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Endoscopic thoracic sympathectomy (ETS) has been used successfully in the treatment of blushing, excessive sweating, and recently also social phobia [1–4]. In addition, a prospective, observational, open-label clinical study comparing sympathectomy with sertraline in the treatment of generalized social anxiety disorder with blushing showed that ETS was associated with a greater reduction of blushing and brief social phobia scale scores in comparison to sertraline and to no treatment [5]. Although compensatory sweating (CS) occurred in 99 % of the patients after ETS, high degrees of satisfaction with treatment were reported by 89 % of patients undergoing ETS. CS has also been frequent in other studies on ETS [1–4, 6–10]. Severe adverse effects, mainly reflex sweating, have been less frequent after the use of endoscopic sympathetic block (ESB) by clips than after ETS [11–14]. Interestingly, according to studies comparing ESB to ETS, no differences in CS between these two treatment modalities were found [15–17]. In fact, according to these articles and also to some other studies [18–21], a more important factor to diminishing CS has been found to be the accurate level of blocking.
The same idea has been followed in the Lin-Telaranta classification, which was presented in the year 2001 [22]. According to Lin-Telaranta classification, the sympathetic disorders were classified into three groups: those restricted to the head, such as conflicted type social phobia and conflicted type blushing (group 1); those involving the head and the face, such as sweating with or without blushing (group 2); and those involving the hands and the underarms (group 3). The selection of different surgical procedures for different disorders of the sympathetic system was performed as follows: ESB 2 for group 1, ESB 3 for group 2, and ESB 4 for group 3.
Social phobia is one form of anxiety syndromes. Typical to the syndrome are the following symptoms: stage fright, fear of embarrassment, fear of social situations, fear of being scrutinized, blushing, heart racing, sometimes trembling, and avoidance of direct gaze contact. We have scored social phobia from 1 to 4 (1 = normal, 2 = slight, 3 = bad, 4 = unbearable) for five of these symptoms: stage fright, fear of embarrassment, fear of social situations, avoidance of gaze contact, and fear of being scrutinized. These we have called the modified Davidson social phobia score [23, 24].
There are few data on long-term results of ESB performed using the Lin-Telaranta classification. This study assessed the long-term results of ESB using the Lin-Telaranta classification in the treatment of blushing, sweating, and social phobia.
Patients and methods
Ninety-five patients (55 men, 40 women; mean age, 38 years; range, 17–71 years) underwent single- or double-sided ESB with clips (Ethicon Ligaclip medium) (ESB) between 1998 and 2005. The surgical procedure was conducted endoscopically under single lumen tube general anesthesia. The patients were placed supine with abduction of both arms for bilateral access. Two intercostal ports between the third and fifth ribs were used to gain access to the chest. The ganglia were always identified at their real anatomical location, based on the junction of intercostal nerve to the ganglion. The procedure was performed mainly bilaterally. The technique included clipping of the thoracic sympathetic ganglia at the selected levels of thoracic 2–4 ganglia with metallic clips according to the principles of the Lin-Telaranta classification [22].
The Lin-Telaranta classification has formed the basis of level selection; however, there may have been individual properties in the patients (e.g., overweight) that always has an effect of adding CS, and thus the level selected has been one lower than the symptom otherwise would have indicated. A unilateral sympathetic block was deemed a good alternative when there was no blushing but still some grounds to expect reflex sweating should the bilateral procedure be selected. A postoperative chest X-ray was obtained to rule out pneumothorax or other complications.
Patients provided written consent to surgery after having been fully informed about the procedure and the possible adverse effects and complications.
Patients were interviewed by e-mail prospectively before the surgery using our routine questionnaire, and also during an appointment with one of us (TT). The same questionnaire was answered postoperatively by every patient. In addition, a long-term questionnaire was sent to all patients whose address was known (n = 80) by a person (TR) who had not been involved in their care. Forty-seven patients (58.8 %) answered the questionnaire on long-term satisfaction.
The modified versions of the Davidson brief social phobia scale and the Liebowitz quality of life scale [23, 24] were used. The severity of the patients’ psychic (performance anxiety, fear of observation, embarrassment, coffee cup neurosis, alertness) and physical (sweating of head, hand or trunk, palpitation, trembling of hands, blushing) symptoms was scored from 1 to 4 (1 = normal, 2 = mild, 3 = moderate, 4 = unbearable). The diagnosis of social phobia was made according to DSM-IV [25]. The patients who were operated to treat social phobia had experienced social phobia for more than 5 years, and medication and/or psychotherapy had not helped; or the patients preferred not to use medication or to undergo psychotherapy, mainly as a result of their felt lack of need for psychiatric treatment.
The mean follow-up was 30.8 months (range, 2–114 months) for all patients, and 51.7 months (range, 34–114 months) for patients who responded to the long-term questionnaire.
Patients were divided into 3 categories: category 1, patients with sweating problems; category 2, patients with blushing; and category 3, patients with symptoms other than sweating or blushing (social phobia in 14 patients, social phobia and trembling of hands in 3, and trembling of hands and palpitation in 1).
Statistical analysis
Student’s t test was used for statistical comparisons. A p value of <0.05 was considered to be statistically significant, and a p value of <0.001 was considered to be statistically highly significant. Statistical comparison were made to all patients and also separately to those 47 patients with long-term follow-up.
Ethics
This study was reviewed and approved by the ethics committee of the Privatix Clinic.
Results
There were no postoperative complications.
The level of ESB was 2 in 41 (43.2 %), 3 in 25 (26.3 %), and 4 in 5 (5.3 %) patients. A left-sided procedure was performed in 19 (20 %) patients. In 5 (5.3 %) patients, the exact level of ESB was not recorded. Among long-term responses the level of ESB was 2 in 24 (51.1 %), 3 in 12 (25.5 %), and 4 in 2 (4.3 %). Only left-sided procedure was performed in 7 (14.9 %) patients. In 2 (4.3 %) patients, the exact level of ESB was not recorded.
The levels of ESB among long-term responses with the different patient categories are shown in Table 1.
Among long-term responses, social phobia decreased from 12.43 to 6.71 (p = 0.004) in category 1, from 13.97 to 7.69 (p < 0.001), and from 13.18 to 79.64 (p = 0.007) in category 3.
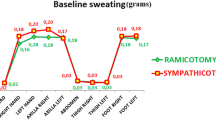
Among all patients with long-term responses, in categories 1 and 2, sweating decreased postoperatively in body areas outside the trunk (facial, palmar, axillary), where it increased slightly from 21.92 to 2.17 (not statistically significant) among patients in category 1 and from 1.83 to 2.34 (p = 0.029) among patients in category 2.
When all the long-term patients were included, sweating in the trunk preoperatively was as follows: normal in 18 (38.3 %) patients, mild in 18 (38.3 %) patients, moderate in 10 (21.3 %) patients, and severe in 1 (2.1 %) patients. Postoperative sweating in the trunk was normal in 9 (19.1 %) patients, mild in 18 (38.3 %) patients, moderate in 15 (31.9 %) patients, and severe in 5 (10.6 %) patients.
Among patients with severe blushing (4 = unbearable), the blushing decreased highly significantly, from 4 to 1.65 (p < 0.001).
Forty-one (87.2 %) patients benefited either clearly (n = 35; 74.5 %) or somewhat (n = 6; 12.7 %) from ESB, while 6 patients (12.8 %) reported no help from the procedure. Thirty (63.8 %) patients expressed a willingness to have the same operation again for the same symptoms. Five (10.6 %) patients expressed that they might have the same operation again for the same symptoms, and 12 (25.5 %) patients expressed that they would not have the same operation again for the same symptoms.
No differences were found in the success rate between the early and late follow-up among patients who also answered the long-term questionnaire.
Clips were removed after a mean of 13 months (range, 7–24 months) from 6 patients as a result of asymmetric blushing or sweating in the face (3 patients), excessive sweating in the trunk (2 patients), or back pain (1 patient). Only two (33.3 %; 1 patient with asymmetric sweating in the face and 1 with excessive sweating in the trunk) patients got help from the removal of the clips.
Discussion
In this long-term prospective study, we found that patients received clear help from ESB performed using the Lin-Telaranta classification to treat blushing, excessive sweating, and social phobia with and without physical symptoms, with a lower incidence of CS compared to that reported for ETS. In addition, no diminishing effect during the follow-up period was found.
In a systematic review of ETS [26], the evidence of the effectiveness of ETS was found to be weak as a result of a lack of randomized trials. A prospective, observational, open-label clinical study comparing ETS with sertraline and no treatment for generalized social anxiety disorder with blushing complaints was later published by Jadresic et al. [5]. In that study, 220 of 330 (66 %) patients seeking treatment for their blushing were eligible to take part. Compared to sertraline, ETS was associated with a significantly greater reduction in the number of patients reporting severe or extreme blushing. As to the individual physiological symptoms, differences between the treatment methods favored ETS in all cases, but these differences were not statistically significant. ETS-treated patients exhibited a greater, statistically significant decline in fear compared to sertraline-treated patients. In addition, the superiority of ETS was statistically significant according to the Liebowitz social anxiety scale. This was the first study comparing the effect of ETS to the only medicine, sertraline, which has been found to have placebo-controlled evidence of efficacy in the treatment of blushing [27]. The mean follow-up in the study of Jadresic et al. [5] was only 11 months, while in our study the mean follow-up was 51.7 months for those patients who completed the long-term follow-up. We did not find any diminishing effect during the follow-up period, suggesting that the results of sympathetic surgery may be permanent. In this respect, our results are in accordance with our previous study, in which the effect of ESB (shorter follow-up) and ETS (longer follow-up) was long-standing [12]. Although our results after sympathic block and after sympathectomy in the article of Zacherl et al. [4] seem to be permanent, the opposite findings have also been reported [28].
We did not compare ESB to medical treatment, but all of our patients had either tried various medicines or psychotherapy before ESB without sufficient results, or patients were not willing to try these treatment methods. However, our patients got clear help from ESB for blushing, sweating, and social phobia. Social phobia alone without physical symptoms decreased a little less. This may be due to left-sided operation among patients with social phobia, but the number of patients with left-sided operation was too small to draw reliable conclusions.
Although the study of Jadresic et al. [5] found ETS to be superior to sertraline, CS was found among most of the patients. Strong evidence for CS as an adverse effect was also found in the review article of Malmivaara et al. [26], in which CS was reported in up to 90 % of the patients operated using ETS. According to the study of Smidfelt and Drott [2], CS was found in 80 % of patients during long-term follow-up. According to study of Currie et al. [29], only 11.6 % of the patients with CS improved with time. Therefore, patients need to be carefully counseled before committing to surgery. In our study, CS of the trunk increased only slightly when all the patients were included, and only in a few patients was the sweating severe. This gives extra support to the previously reported findings of literature that there are clearly reduced frequencies of CS after ESB than after ETS [1–4, 6–14], which is important to enable satisfactory treatment of more patients with sympathetic surgery. In addition, it has been shown that there are no differences in the results concerning preoperative symptoms after ESB compared to ETS [12]. It is likely that the reduced frequency of CS in our study compared to other studies on ESB resulted from the use of the Lin-Telaranta classification [22]. This classification method has been shown by Lin and Telaranta [22] to benefit patients in all groups, as shown by relief in their presenting symptoms and by the lower incidence of unacceptable reflex sweating compared to ETS. Accordingly, a Society of Thoracic Surgeons expert consensus for the surgical treatment of hyperhidrosis was created using the same recommendations as in Lin-Telaranta classification [30].
An additional benefit of ESB has been believed to be the reversibility of adverse effects by removing the clips. In our study, clips were removed from 6 patients, mostly due to CS. However, only 2 patients experienced relief from the adverse effect after clip removal. In other studies, CS either decreased substantially in 48 % of the patients [14] or recovered in 80 % of the patients [11] after clips were removed. Recently two animal studies have been performed that studied the effect of clipping on the sympathetic chain as well as the possibility of regeneration after removal of the clips [31, 32]. In the study by Candas et al. [31], the clips were shown to cause a degeneration of neural structures within 2 days. By 45 days after the removal of the clips, progressive, degenerative changes along the axons of the sympathetic cells were observed [31]. In the study of Loscertales et al. [32], a few residual myelinated and nonmyelinated fibers were visible by 30 days after operation and 20 days after clip removal. The conclusions of these two studies were that clipping cannot be considered a reversible technique [31, 32]. Reliable conclusions from animal studies, which should be followed among humans, cannot be drawn because the decrease of CS occurred in 48 % of the patients after clip removal after a median of 11 months after ESB in the study of Sugimura et al. [14] and 33 % after median of 13 months in the study presented here. However, if severe adverse effects do occur after ESB, the clips should be removed during the first month after ESB to improve the recovery of the sympathetic nerves. This is now our current policy at the Privatix Clinic.
Conclusions
In this long-term prospective study, we found that patients clearly benefited from ESB performed using the Lin-Telaranta classification to treat blushing, excessive sweating, and social phobia with or without physical symptoms. We found no diminishing effect during the follow-up period. In addition, the incidence of unacceptable CS was very low. However, if severe adverse effects do occur, clips should be removed during the first month after ESB to ensure the recovery of the sympathetic nerves.
References
Coveliers H, Atif S, Rauwerda J, Wisselink W (2011) Endoscopic thoracic sympathectomy: long-term results for treatment of upper limb hyperhidrosis and facial blushing. Acta Chir Belg 111:293–297
Smidfelt K, Drott C (2011) Late results of endoscopic thoracic sympathectomy for hyperhidrosis and facial blushing. Br J Surg 98:1719–1724
Telaranta T (1998) Treatment of social phobia by endoscopic thoracic sympathicotomy. Eur J Surg Suppl 580:27–32
Zacherl J, Huber ER, Imhof M, Plas EG, Herbst F, Függer R (1998) Long-term results of 630 thoracoscopic sympathicotomies for primary hyperhidrosis: the Vienna experience. Eur J Surg Suppl 580:43–46
Jadresic E, Súarez C, Palacios E, Palacios F, Matus P (2011) Evaluating the efficacy of endoscopic thoracic sympathectomy for generalized social anxiety disorder with blushing complaints: a comparison with Sertraline and no treatment—Santiago de Chile, 2003–2009. Innov Clin Neurosci 8:24–35
Gossot D, Galetta D, Pascal A, Debrosse D, Caliandro R, Girard P, Stern J, Grunenwald D (2003) Long-term results of endoscopic thoracic sympathectomy for upper limb hyperhidrosis. Ann Thorac Surg 75:1075–1079
Dumont P, Denoyer A, Robin P (2004) Long-term results of thoracoscopic sympathectomy for hyperhidrosis. Ann Thorac Surg 78:1801–1807
Licht P, Ladegaard L, Pilegaard H (2006) Thoracoscopic sympathectomy for isolated facial blushing. Ann Thorac Surg 81:1863–1866
Libson S, Kirstein B, Mizrahi S, Lantsberg L (2007) Evaluation of compensatory sweating after bilateral thoracoscopic sympathectomy for palmar hyperhidrosis. Surg Laparosc Endosc Percutan Tech 17:511–513
Bachmann K, Standl N, Kaifi J, Busch P, Winkler E, Mann O, Izbicki J, Strate T (2009) Thoracoscopic sympathectomy for palmar and axillary hyperhidrosis: four-year outcome and quality of life after bilateral 5-mm dual port approach. Surg Endosc 23:1587–1593
Lin CC, Mo LR, Lee LS, Ng SM, Hwang MH (1998) Thoracoscopic T2-sympathetic block by clipping—a better and reversible operation for treatment of hyperhidrosis palmaris: experience with 326 cases. Eur J Surg Suppl 580:13–16
Pohjavaara P, Telaranta T (2005) Endoscopic sympathetic block as treatment of social phobia. Eur Surg 37:137–142
Pohjavaara P, Telaranta T, Väisänen E (2001) Endoscopic sympathetic block—new treatment of choice for social phobia? Ann Chir Gynaecol 90:177–184
Sugimura H, Spratt E, Compeau C, Kattail D, Shargall Y (2009) Thoracoscopic sympathetic clipping for hyperhidrosis: long-term results and reversibility. J Thorac Cardiovasc Surg 137:1370–1376
Whitson B, Andrade R, Dahlberg P, Maddaus M (2007) Evolution of clipping for thoracoscopic sympathectomy in symptomatic hyperhidrosis. Surg Laparosc Endosc Percutan Tech 17:287–290
Coelho Mde S, Silva RF, Mezzalira G, Bergonse Neto N, Stori Wde S Jr, dos Santos AF, El Haje S (2009) T3–T4 endoscopic sympathetic blockade versus T3T4 video thoracoscopic sympathectomy in the treatment of axillary hyperhidrosis. Ann Thorac Surg 88:1780–1785
Yanagihara T, Ibrahimiye A, Harris C, Hirsch J, Gorenstein L (2010) Analysis of clamping versus cutting of T3 sympathetic nerve for severe palmar hyperhidrosis. J Thorac Cardiovasc Surg 140:984–989
Neumayer C, Zacherl J, Holak G, Függer R, Jakesz R, Herbst F, Bischof G (2004) Limited endoscopic thoracic sympathetic block for hyperhidrosis of the upper limb: reduction of compensatory sweating by clipping T4. Surg Endosc 18:152–156
Reisfield R (2006) Sympathectomy for hyperhidrosis: should we place the clamps at T2–T3 or T3–T4? Clin Auton Res 16:384–389
Schmidt J, Bechara F, Altmeyer P, Zirngibl H (2006) Endoscopic thoracic sympathectomy for severe hyperhidrosis: impact of restrictive denervation on compensatory sweating. Ann Thorac Surg 81:1048–1055
Li X, Tu Y, Lin M, Lai F, Chen J, Dai Z (2008) Endoscopic thoracic sympathectomy for palmar hyperhidrosis: a randomized control trial comparing T3 and T2–4 ablation. Ann Thorac Surg 85:1747–1751
Lin CC, Telaranta T (2001) Lin-Telaranta classification: the importance of different procedures for different indications in sympathetic surgery. Ann Chir Gynaecol 90:161–166
Davidson JR, Miner CM, De Veaugh-Geiss J, Tupler LA, Colket JT, Potts NL (1997) The brief social phobia scale: a psychometric evaluation. Psychol Med 27:161–166
Taiminen T (1998) Sosiaalisten tilanteiden pelon hoito. Duodecim 114:73–79
American Psychiatric Association (2000) Diagnostic statistical manual of mental disorders. DSM-IV-TR, 4th edn. American Psychiatric Press, Washington
Malmivaara A, Kuukasjärvi P, Autti-Rämö I, Kovanen N, Mäkelä M (2007) Effectiveness and safety of endoscopic thoracic sympathectomy for excessive sweating and facial blushing: a systematic review. Int J Technol Assess Health Care 23:54–62
Connor KM, Davidson JRT, Chung H, Yang R, Clary CM (2006) Multidimensional effects of sertraline in social anxiety disorder. Depress Anxiety 23:6–10
Hasmonai M, Assalia A, Kopelman D (2001) Thoracoscopic sympathectomy for palmar hyperhidrosis. Ablate or resect? Surg Endosc 15:435–441
Currie A, Evans J, Thomas P (2011) An analysis of the natural course of compensatory sweating following thoracoscopic sympathectomy. Int J Surg 9:437–439
Cerfolio R, De Campos J, Bryant C, Miller D, DeCamp M, McKenna R, Krasna M (2011) The society of thoracic surgeons expert consensus for the surgical treatment of hyperhidrosis. Ann Thorac Surg 91:1642–1648
Candas F, Gorur R, Haholu A, Yiyit N, Yildizhan A, Gezer S, Sen H, Isitmangil T (2012) The effects of clipping on thoracic sympathetic nerve in rabbits: early and late histopathological findings. Thorac Cardiovasc Surg 60:280–284
Loscertales J, Congregado M, Jimenez-Merchan R, Gallardo G, Trivino A, Moreno S, Loscertales B, Galera-Ruiz H (2012) Sympathetic chain clipping for hyperhidrosis is not a reversible procedure. Surg Endosc 26:1258–1263
Disclosures
Tuomo Rantanen and Timo Telaranta have no conflicts of interest or financial ties to disclose.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Rantanen, T., Telaranta, T. Long-term results of endoscopic symphathetic block using the Lin-Telaranta classification. Surg Endosc 27, 3860–3864 (2013). https://doi.org/10.1007/s00464-013-2995-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00464-013-2995-3