Abstract
Background
Although there has been much debate over the fate of the gallbladder (GB) after endoscopic common bile duct (CBD) stone removal, subsequent cholecystectomy is generally recommended in patients with GB stones to prevent further biliary complications. The aims of this study were to assess the natural course of the patients with GB in situ after endoscopic CBD stone removal and to evaluate the necessity of prophylactic cholecystectomy.
Methods
Four hundred sixty-one patients who had undergone CBD stone removal at Yeungnam University Hospital between January 2000 and December 2004 were retrospectively analyzed, and 232 patients were ultimately enrolled in this study.
Results
The mean duration of follow-up was 73 (range = 7–126) months in the cholecystectomy group and 66 (6–127) months in the GB in situ group (p = 0.168). Ten patients (14.7 %) in the cholecystectomy group and 31 patients (18.9 %) in the GB in situ group developed recurrent CBD stones (p = 0.295). The highest percentage of recurrent CBD stones in both groups was that for brown stones (80 and 80.6 %). In the GB in situ group, cumulative recurrence rates of CBD stones were not significantly different between patients with GB stones and without GB stones (15.9 vs. 20 %, p = 0.798). However, the incidence of acute cholecystitis was significantly higher in patients with GB stones compared to patients without GB stones (13.6 vs. 2.5 %, p = 0.003).
Conclusions
Prophylactic cholecystectomy seems to be unnecessary in patients without GB stones after endoscopic sphincterotomy. However, in patients with GB stones, elective cholecystectomy or close observation is recommended due to the higher risk of cholecystitis.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Choledocholithiasis is defined as a presence or formation of gallstones in the common bile duct (CBD), which can be caused by either primary stones that originated from the bile duct or by secondary stones that migrated from the gallbladder (GB), and can lead to obstructive jaundice, cholangitis, or pancreatitis.
With the development of endoscopic technology, endoscopic CBD stone removal has been widely accepted as a safe and effective method for the treatment of choledocholithiasis since the first successful procedure of endoscopic sphincterotomy (ES) in 1974 [1, 2]. After endoscopic CBD stone removal, prophylactic cholecystectomy is generally recommended in patients with an intact GB to prevent further complications such as acute cholecystitis, recurrent CBD stones, or cholangitis.
However, the subsequent management strategy for patients with GB in situ after endoscopic bile duct stone removal still remains controversial. In a prospective study, laparoscopic cholecystectomy was recommended in patients with GB stones after ES [3]. In contrast to that study, it has been suggested that elective cholecystectomy after ES did not reduce the recurrence of biliary complications [4]. Late biliary complications did not always occur even if a calculous GB was left in situ. The components of CBD stones in Korea, which are almost pigment stones, are different from those in Western countries. Therefore, the natural course of Korean patients with GB in situ is likely to be different from that of patients in Western countries. Most previous studies had a relatively short follow-up duration while long-term follow-up studies were insufficient.
The aims of this study were to assess the long-term follow-up results of patients with GB in situ after ES for removal of CBD stones to identify further biliary complications and to evaluate the necessity for prophylactic cholecystectomy after ES.
Patients and methods
A total of 461 patients who underwent successful endoscopic CBD stone removal at Yeungnam University Hospital from January 2000 to December 2004 were analyzed retrospectively. Endoscopic CBD stone removal was attempted after ES. All endoscopic retrograde cholangiopancreatography (ERCP) procedures were performed by using side-viewing endoscopes (TJF-240; Olympus Optical Corporation, Tokyo, Japan). Stones were extracted by using retrieval baskets and/or balloon-tipped catheters after ES in all patients. ES was done as large as possible with a pull-type sphincterotome (Papillotome, MTW® Endoskopie, Wesel, Germany) in patients with a normal anatomy or with a needle knife sphincterotome (TW 1/23; Medizin-Technische-Werkstte, Endoskopie, Sebastianusstrabe, Wesel, Germany) over a previously inserted plastic stent into the bile duct in cases with Billroth II gastrojejunostomy. An endoscopic mechanical lithotripsy was attempted to fragment the stones if the stones were too big to remove intact. After successful endoscopic removal of CBD stones in patients with an intact GB, cholecystectomy was recommended in all patients if possible. Cholecystectomy was not performed in patients of advanced age, patients with multiple comorbidities, or in patients who refused surgery. Patients were excluded from the study if they had a history of previous cholecystectomy (147 patients), concomitant intrahepatic stones (16 patients), pancreaticobiliary malignancies (20 patients), and insufficient follow-up of less than at least 6 months (46 patients).
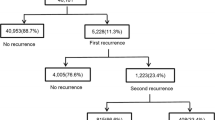
A total of 232 patients with an intact GB at the time of endoscopic CBD stone removal were enrolled in this study. Patients were divided into a cholecystectomy group (n = 68; 63.6 ± 14.8 years of age, 36 males), in which prophylactic cholecystectomy after endoscopic CBD stone removal was performed, and a GB in situ group (n = 164, 71.6 ± 13.6 years of age, 84 males). The cholecystectomy group was divided into two groups according to the presence or absence of GB stones. Diagnosis of GB stones was made by ultrasonography which was performed on all patients.
Follow-up evaluations were conducted using chart reviews and personal interviews at our outpatient clinic or by phone calls. Patients’ demographic details, the characteristics of the CBD stones, the presence of GB stones, development of biliary complications, time and indications of cholecystectomy, and time and cause of death (if applicable) were collected. Recurrence of CBD stones was arbitrarily defined as reappearance 6 months after ES. We regarded CBD stones that appeared within 6 months after endoscopic stone removal as residual stones. All recurrent CBD stones were confirmed by ERCP. The protocol was approved by the institutional review board of our hospital.
Statistical analysis
Statistical analysis was performed using SPSS for Windows (SPSS, Inc., Chicago, IL, USA). Data were expressed as the mean ± SD or median with range. Differences with a p < 0.05 were considered statistically significant.
Results
After endoscopic CBD stone removal, 68 patients (30.6 %) underwent subsequent cholecystectomy and 164 patients (60.4 %) did not. Of the GB in situ group, 44 patients had GB stones and 120 patients did not. The baseline characteristics are summarized in Table 1. Of the 68 patients who had elective cholecystectomy after endoscopic CBD stone removal, 57 patients (83.3 %) underwent laparoscopic cholecystectomy and 11 patients (16.2 %) underwent open cholecystectomy. The average interval between ERCP and cholecystectomy was 16.7 ± 24.4 days (range = 2–147). The GB in situ group was significantly older compared to the cholecystectomy group (71.6 ± 13.6 vs. 63.6 ± 14.8, p = 0.000). The percentage of stones that were brown was higher in the cholecystectomy group and the GB in situ group (61.8 and 56.1 %) compared with that of cholesterol and black stones. Besides age, there were no significant differences in the patients’ baseline characteristics between the cholecystectomy group and the GB in situ group.
The mean duration of follow-up was 73 (7–126) months in the cholecystectomy group and 66 (6–127) months in the GB in situ group (p = 0.168). In the GB in situ group, there was no significant difference in follow-up duration between patients with GB stones and those without GB stones [60 (6–124) vs. 69 (6–127) months, p = 0.369].
During a median 5.7 years of follow-up, 10 patients (14.7 %) in the cholecystectomy group and 31 patients (18.9 %) in the GB in situ group developed recurrent CBD stones (Table 2). Papillary stenosis was found in 40.0 and 51.6 % of patients with recurrent CBD stones in the cholecystectomy and the GB in situ group, respectively. Either endoscopic sphincterotomy or endoscopic papillary large-balloon dilation was done to remove the recurrent CBD stones in these patients. A higher percentage of the recurrent CBD stones were brown stones (80 % and 80.6 %) compared with cholesterol and black stones in the cholecystectomy group and the GB in situ group. The time to recurrence of CBD stones after ES was 39.2 ± 25.1 and 32.7 ± 30.1 months in the cholecystectomy group and the GB in situ group, respectively (p = 0.525). In the GB in situ group, 7 (15.9 %) of the patients with GB stones and 24 (20.0 %) of the patients without GB stones had recurrent CBD stones (p = 0.798). The time to recurrence of CBD stones was 27.5 ± 19.6 months for patients with GB stones and 35.5 ± 31.8 months for patients without GB stones (p = 0.415). The recurrence rates of CBD stones were not significantly different between the cholecystectomy group and the GB in situ group (p = 0.295) and between those with and without GB stones within the GB in situ group (p = 0.798). There was no relationship between recurrence of stones and delayed onset of cholecystectomy in the cholecystectomy group (Table 3).
Acute cholecystitis developed in six patients (13.6 %) in the GB in situ group with GB stones and in three patients (2.5 %) in the GB in situ group without GB stones, and there was a significant difference between these two groups (p = 0.003). Of the three patients in GB in situ group with no GB stones who developed cholecystitis, gallstones were found in two patients at the time of cholecystitis. Of the nine patients who required cholecystectomy during follow-up in GB in situ group, three (37.5 %) and five (62.5 %) underwent laparoscopic and open cholecystectomy, respectively. The proportion of open cholecystectomy was significantly higher in GB in situ group than in the cholecystectomy group (62.5 vs. 16.2 %, p = 0.002) (Table 4).
Discussion
Since Classen and Demling [1] and Kawai et al. [2] performed the first ES in 1974, endoscopic CBD stone removal has been widely accepted as a safe and principal procedure for the treatment of bile duct stones and is often performed in patients with an intact GB. Although prophylactic cholecystectomy after endoscopic CBD stone removal is commonly recommended for patients with GB in situ to prevent further biliary complications, the necessity for cholecystectomy is still controversial, especially in patients without GB stones or elderly patients.
The rate of subsequent cholecystectomy was in the range of 4.8–22 % in various studies [5–7]. The incidence of recurrent biliary symptoms with a wait-and-see policy after ES was shown to be about 10 % in many retrospective and nonrandomized studies [4, 5, 8–10]. In a retrospective study, a higher mortality rate was found in patients in whom cholecystectomy after ES was deferred compared to that of patients who had their GB removed electively [11]. In contrast, other studies suggested that prophylactic cholecystectomy after ES did not reduce the incidence of recurrent biliary complications [4, 7]. Late complications after ES include cholecystitis, recurrent CBD stones, and cholangitis. In the present study, during a mean follow-up of 73 months in the cholecystectomy group and 66 months in the GB in situ group, there was no significant difference in the incidence of overall biliary complications between the two groups. Our results support the wait-and-see policy for the management of patients with intact GB after ES.
Choledocholithiasis can be caused by either primary bile duct stones originating in the bile duct or by secondary bile duct stones that migrated from the GB. Primary CBD stones consist mainly of brown pigment stones and secondary CBD stones consist of a high percentage of cholesterol stones. It is believed that there are still many differences in the pathogenesis of the formation of CBD stones, i.e., the majority of CBD stones are secondary stones that originated in the GB in Western countries, whereas primary stones are likely to be formed in the bile duct in Korean patients. This can explain the very high percentage of patients with no GB stones in GB in situ group in this study.
In this study, a higher proportion of brown stones at the initial ERCP (61.8 % in the cholecystectomy group and 56.1 % in the GB in situ group) indicated that CBD stones were likely to be formed in the bile duct, and ascending infection seemed to be an important factor in the formation of CBD stones in our patients. Therefore, the role of the GB in the formation of CBD stones was not important, and the need for subsequent cholecystectomy after ES to prevent recurrent CBD stones might be low in our patients.
The recurrence rate of CBD stones after ES was reported to be in the range of 6.5–17.4 % in patients with GB in situ [12–14]. Recurrent CBD stones are usually found in the CBD within several years after cholecystectomy and most often are brown pigment stones [15]. In this study, with a median follow-up of almost 6 years, 10 patients (14.7 %) in the cholecystectomy group and 31 patients (18.9 %) in the GB in situ group developed recurrent CBD stones (p = 0.295). This result was consistent with another study [16]. Recurrent CBD stones occurred within 3 years after ES in both groups and the majority of recurrent CBD stones were brown stones. Papillary stenosis occurred in almost half of the patients with recurrent CBD stones in both the cholecystectomy and GB in situ groups. Lack of good bile flow may in part contribute to the formation of recurrent bile duct stones. However, the pathogenesis of recurrent bile duct stones after ES is multifactorial. Stricture at the sphincterotomy site or a dilated CBD with consequent bile stasis and sludge formation, bacterial infection of the bile duct, and duodenocholedochal reflux are known to play important roles in the formation of CBD stones after ES. Although migration of the GB stone into the CBD is another potential mechanism of CBD stone formation, the number of secondary CBD stones was low in this study because the majority of recurrent CBD stones were brown pigment stones. Furthermore, the presence of GB stones in the GB in situ group did not increase the risk of recurrent CBD stones. In theory, the presence of a GB stone is thought to be a risk factor for secondary CBD stones. However, according to this study and the other previously mentioned study [14], there was no significant difference between patients with and without GB stones. It is thought that the formation of a new GB stone is the major cause of recurrent CBD stones. Therefore, prophylactic cholecystectomy to reduce the risk of CBD stone recurrence is not necessary in patients without GB stones after ES.
Acute cholecystitis is important concern in patients with GB in situ after ES, especially in patients with a GB stone. The risk of acute cholecystitis might be increased after ES in patients with the GB in situ, because dysfunction of the Oddi sphincter could lead to biliary infection secondary to reflux of duodenal contents into the bile duct and subsequently increase the risk of ascending infection of the GB and cholecystitis. The incidence of cholecystitis after ES in previous studies was 19 and 22 % in patients with GB stones [17, 18], and there were no cases of cholecystitis in patients without GB stones until the formation of new GB stones occurred [17, 19]. In the present study, six patients (13.6 %) in the GB in situ group with GB stones and three patients (2.5 %) in the GB in situ group without GB stones developed acute cholecystitis during a median follow-up of almost 6 years. The cause of the relatively lower incidence of acute cholecystitis in the present study compared to the other study [17, 18] was not clear. Discrepancies in the incidence of cholecystitis in different studies might be explained by heterogeneity in factors such as age, sex, size and number of GB stones, diameter of the cystic duct, and follow-up duration. In this study, the incidence of cholecystitis was 2.5 % in the GB in situ group without GB stones. Of the three patients in GB in situ group with no GB stones who developed cholecystitis, gallstones were found in two patients at the time of cholecystitis. So the actual incidence of acalculous cholecystitis was not high. The formation of GB stones might be related to the long-term follow-up period or the higher percentage of elderly patients included in the study.
Another important aspect is the conversion rate to open cholecystectomy. In the present study, there was almost a fourfold increase of conversion to open cholecystectomy in the GB in situ group compared to the cholecystectomy group (62.5 vs. 16.2 %, p = 0.002). This high conversion rate may support the necessity of prophylactic cholecystectomy in patients with GB in situ after ES.
In summary, GB in situ did not increase the formation of recurrent CBD stones after CBD stone removal by ES. Considering the relatively lower incidence of cholecystitis and no increase in the risk of CBD stones, a wait-and-see policy may be recommended for patients with GB in situ without GB stones after ES. However, in patients with GB stones, elective cholecystectomy or close observation is recommended due to a higher incidence of acute cholecystitis and a higher rate of conversion to open cholecystectomy.
References
Classen M, Demling L (1974) Endoscopic sphincterotomy of the papilla of vater and extraction of stones from the choledochal duct (author’s transl). Dtsch Med Wochenschr 99:496–497
Kawai K, Akasaka Y, Murakami K, Tada M, Koli Y (1974) Endoscopic sphincterotomy of the ampulla of Vater. Gastrointest Endosc 20:148–151
Boerma D, Rauws EA, Keulemans YC, Janssen IM, Bolwerk CJ, Timmer R, Boerma EJ, Obertop H, Huibregtse K, Gouma DJ (2002) Wait-and-see policy or laparoscopic cholecystectomy after endoscopic sphincterotomy for bile-duct stones: a randomised trial. Lancet 360:761–765
Lai KH, Lin LF, Lo GH, Cheng JS, Huang RL, Lin CK, Huang JS, Hsu PI, Peng NJ, Ger LP (1999) Does cholecystectomy after endoscopic sphincterotomy prevent the recurrence of biliary complications? Gastrointest Endosc 49:483–487
Hill J, Martin DF, Tweedle DE (1991) Risks of leaving the gallbladder in situ after endoscopic sphincterotomy for bile duct stones. Br J Surg 78:554–557
Kullman E, Borch K, Dahlin LG, Liedberg G (1991) Long-term follow-up of patients with gallbladder in situ after endoscopic sphincterotomy for choledocholithiasis. Eur J Surg 157:131–135
Kwon SK, Lee BS, Kim NJ, Lee HY, Chae HB, Youn SJ, Park SM (2001) Is cholecystectomy necessary after ERCP for bile duct stones in patients with gallbladder in situ? Korean J Intern Med 16:254–259
Hammarstrom LE, Holmin T, Stridbeck H (1996) Endoscopic treatment of bile duct calculi in patients with gallbladder in situ: long-term outcome and factors. Scand J Gastroenterol 31:294–301
Neoptolemos JP, Carr-Locke DL, Fraser I, Fossard DP (1984) The management of common bile duct calculi by endoscopic sphincterotomy in patients with gallbladders in situ. Br J Surg 71:69–71
Welbourn CR, Beckly DE, Eyre-Brook IA (1995) Endoscopic sphincterotomy without cholecystectomy for gall stone pancreatitis. Gut 37:119–120
Archibald JD, Love JR, McAlister VC (2007) The role of prophylactic cholecystectomy versus deferral in the care of patients after endoscopic sphincterotomy. Can J Surg 50:19–23
Kang EH, Na YS, Lee SH, Choi TY, Shin WC, Lee JH, Choi WC, Kim KY (2000) Endoscopic treatment of bile duct calculi in patients with gallbladder in situ. Korean J Gastrointest Endosc 20:21–25
Kang JK, Park IS, Chung JB, Moon YM, Kim HG, Song SY, Lee JH, Cheong JY, Jung BG (1999) Factor influencing the recurrence of CBD stones after an endoscopic sphincteromy. Korean J Gastrointest Endosc 19:581–587
Park CW, Kim JH, Lee DJ, Kim KY, Suh JI, Kim TN, Chung MK (1997) A study of necessity for cholecystectomy after endoscopic common bile duct stone removal. Korean J Gastroenterol 29:659–666
Kim MH, Lim BC, Myung SJ, Lee SK, Ohrr HC, Kim YT, Roe IH, Kim JH, Chung JB, Kim CD, Shim CS, Yun YB, Min YI, Yang US, Kang JK (1999) Epidemiological study on Korean gallstone disease: a nationwide cooperative study. Dig Dis Sci 44:1674–1683
Yasui T, Takahata S, Kono H, Nagayoshi Y, Mori Y, Tsutsumi K, Sadakari Y, Ohtsuka T, Nakamura M, Tanaka M (2012) Is cholecystectomy necessary after endoscopic treatment of bile duct stones in patients older than 80 years of age? J Gastroenterol 47:65–70
Tanaka M, Takahata S, Konomi H, Matsunaga H, Yokohata K, Takeda T, Utsunomiya N, Ikeda S (1998) Long-term consequence of endoscopic sphincterotomy for bile duct stones. Gastrointest Endosc 48:465–469
Yi SY (2000) Recurrence of biliary symptoms after endoscopic sphincterotomy for choledocholithiasis in patients with gall bladder stones. J Gastroenterol Hepatol 15:661–664
Kageoka M, Watanabe F, Maruyama Y, Nagata K, Ohata A, Noda Y, Miwa I, Ikeya K (2009) Long-term prognosis of patients after endoscopic sphincterotomy for choledocholithiasis. Dig Endosc 21:170–175
Disclosures
Drs. Mei Lan Cui, Joon Hyun Cho, and Tae Nyeun Kim have no conflicts of interest or financial ties to disclose.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Cui, M.L., Cho, J.H. & Kim, T.N. Long-term follow-up study of gallbladder in situ after endoscopic common duct stone removal in Korean patients. Surg Endosc 27, 1711–1716 (2013). https://doi.org/10.1007/s00464-012-2662-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00464-012-2662-0