Abstract
Background
There is no consensus whether patients who underwent endoscopic common bile duct (CBD) stone removal should be followed up periodically and whether patients with gallbladder (GB) stones should undergo cholecystectomy. Thus, this study aimed to investigate the recurrence rate of CBD stones and the difference in recurrence rate according to cholecystectomy.
Methods
We conducted a population-based study using the National Health Insurance database. Patients diagnosed with CBD stones and with procedure registry of endoscopic stone removal were included. The primary outcome was the recurrence rate of CBD stones. The secondary outcome was the difference in recurrence rate of CBD stones according to cholecystectomy.
Results
A total of 46,181 patients were identified. The mean follow-up was 4.2 years. The first CBD stone recurrence occurred in 5228 (11.3%) patients. The cumulative first recurrence rate was low. However, the second and third recurrence rates were 23.4 and 33.4%, respectively. The cumulative second and third recurrence rates were high and gradually increased with time. The recurrence rate in the non-cholecystectomy group was higher than that in the cholecystectomy group (p < 0.0001). The relative risk for CBD stone recurrence in the non-cholecystectomy group was higher in younger patients, with 3.198 in patients < 50 years, 2.371 in 50–59 years, 1.618 in 60–69 years, and 1.262 in ≥ 70 years (p < 0.0001).
Conclusions
Regular follow-up is not routinely recommended for patients with first-time endoscopic stone removal, but is recommended for patients with recurrent stones. Cholecystectomy is recommended for patients with GB stones who are younger than 70 years.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Endoscopic sphincterotomy and stone removal is the standard treatment for common bile duct (CBD) stone and is generally accepted as safe and effective. Common bile duct stone recurrence, as a late complication, is a major concern because it can lead to cholangitis and biliary sepsis. To reduce CBD stone recurrence and/or to detect and treat the recurrence early, two important concerns regarding patient care after successful removal of CBD stones should be addressed: the first is whether patients should be followed up for stone recurrence, and the second is whether to perform prophylactic cholecystectomy in patients with gallbladder (GB) stones.
Follow-up studies have shown that the incidence of CBD stone recurrence after endoscopic treatment was 2–22% [1,2,3,4,5,6,7,8,9,10]. However, most studies included only a few patients and had relatively short follow-up durations. Thus, the recurrence rate of CBD stones should be investigated to determine the need for follow-up. The risk factors for recurrent CBD stones were known as GB stones, dilated CBD, angulation of the CBD, biliary stricture, use of lithotripsy, and periampullary diverticulum [1,2,3, 11,12,13,14]. Although some studies suggested careful follow-up of patients with risk factors, there is no consensus whether patients who underwent CBD stone removal should have follow-up examination, and if follow-up examinations should be performed, it is yet unknown which patients to target as well as the timing and procedure. A comprehensive understanding of CBD stone recurrence would provide better guidance for clinicians in the follow-up of patients.
Prophylactic cholecystectomy is generally considered to prevent biliary complications in patients with GB stones after endoscopic stone removal. In two prospective clinical trials, laparoscopic cholecystectomy was recommended in those patients [15, 16]. However, other studies have shown that cholecystectomy has no effect in reducing biliary complications [13, 17,18,19,20]. The need for subsequent cholecystectomy, particularly in older patients, has been a major issue.
Population-based data have been of interest lately because they can help overcome the underpowered results of small single-center studies, and as far as we know, there are no population-based data on CBD stone recurrence. The aim of this study was to investigate the recurrence rate of CBD stones in patients who have undergone CBD stone removal and the difference in the recurrence rate of CBD stones according to cholecystectomy, using the Korean National Health Insurance Service (NHIS) database.
Methods
Data sources
The NHIS is a mandatory universal health insurance system in Korea that provides comprehensive medical care to more than 98% of all Korean citizens since 1999 [21, 22]. Thus, nearly all of the data in the health system are centralized in large databases. Records from the NHIS database include patients’ sociodemographic information, diagnosis of diseases, procedures, prescription drugs, hospital information, and the direct medical cost of both inpatient and outpatient care. Since Koreans have a single identification number, their health insurance records are not duplicated or omitted. The diagnoses are coded using the Korean Classification of Disease (KCD), which is similar system to the International Classification of Diseases, Tenth Revision. The NHIS database has been used extensively in many epidemiologic studies in Korea [23, 24]. The detailed information for data access of NHIS could be obtained from the NHIS website (https://nhiss.nhis.or.kr). This study design was reviewed and approved by the Institutional Review Board of NHIS Ilsan Hospital.
Study design and population
We were able to extract data from the NHIS database from January 1, 2002, to December 31, 2013. From all individuals of the population in South Korea alive at any given time between January 1, 2004, and December 31, 2012, patients with diagnostic KCD codes of CBD stone diseases (K80.50, K80.51, K80.31, K80.30, K80.41, K80.40) and one or more procedure registry code (Q7764) of endoscopic CBD stone removal were included in this study. To restrict the enrollment to patients with first CBD stone presentation, we excluded patients who had undergone endoscopic CBD stone removal between January 1, 2002, and December 31, 2003. All subjects were monitored until December 31, 2013, or death. Nobody was lost to follow-up.
Common bile duct stone recurrence was defined as another procedure registry of endoscopic stone removal after more than 6 months from the previous procedure. If another CBD stone was removed within 6 months, it was not considered as a recurrence because it was possibly either a subsequent treatment or residual stone. Recurrence was noted as the first, the second, or the third.
To evaluate the difference in the recurrence rate of CBD stones according to cholecystectomy in patients with GB stones, we extracted data on diagnostic KCD codes of GB stone diseases (K80.20, K80.21, K80.00, K80.01, K80.10, K80.11) and procedure registry code (Q7380) of cholecystectomy in all subjects. All subjects were divided into three groups based on GB status: GB stone group, previous cholecystectomy group, and indeterminate GB status group. The GB stone group was defined as having the diagnostic code of GB stone at the time of CBD stone removal. The previous cholecystectomy group was defined as having a registry record of cholecystectomy at least 3 months before CBD stone removal. The indeterminate GB status group was defined as the case without available information on GB status, and this group possibly included patients with intact GB without GB stones, those with previous cholecystectomy before 2002, or those with intact GB with GB stones but were missing registry of diagnostic code of GB stones. Furthermore, the GB stone group was subdivided into those who underwent cholecystectomy within 3 months after or before CBD stone removal (cholecystectomy group) and those who did not undergo cholecystectomy during same period (non-cholecystectomy group). We compared the recurrence rate of CBD stones between the two groups. In the non-cholecystectomy group, patients who underwent cholecystectomy later during the follow-up were analyzed only until that time.
The primary outcome was the recurrence rate of CBD stones in patients with previous endoscopic stone removal. The secondary outcome was the difference in the recurrence rate of CBD stones between the cholecystectomy and non-cholecystectomy groups in patients with GB stones.
Statistical analysis
The cumulative recurrence rate of CBD stones was estimated using the Kaplan–Meier method. The log-rank test was used to test the statistical difference in the recurrence rate of CBD stones between groups. Cox proportional hazard regression with 95% confidence intervals (CIs) was used to determine the hazard risk for CBD stone recurrence in different groups. A p value < 0.05 was considered significant. All statistical analyses were performed using SAS software (version 9.4; SAS Institute Inc., Cary, NC, USA).
Results
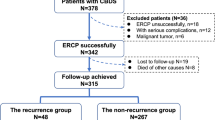
We extracted the data of patients who were diagnosed with CBD stones and who received endoscopic CBD stone removal between 2004 and 2012. After excluding patients who underwent CBD stone removal between 2002 and 2003, a total of 46,181 patients were included in this study. The mean age was 64.65 years, and the male/female ratio was 1:0.91. The age distribution of the patients was as follows: < 50 years, 16.3%; 50–59 years, 14.9%; 60–69 years, 23.6%; ≥ 70 years, 44.7%. The mean follow-up duration was 4.2 years. During follow-up, 4758 patients were dead.
Recurrence rate of CBD stones
Of 46,181 patients, 40,953 (88.7%) never had CBD stone recurrence. However, 5228 (11.3%) patients had CBD stone recurrence, and among these patients, 1223 (23.4%) had a second CBD stone recurrence. Furthermore, among these patients with second CBD stone recurrence, 408 (33.4%) had a third CBD stone recurrence (Fig. 1.) The maximum number of recurrence was ten in one patient, nine in three patients, eight in four patients, seven in eight patients, six in 14 patients, five in 37 patients, and four in 128 patients. The cumulative first recurrence rate was relatively low: 2.2% at 1 year, 6.0% at 2 years, 9.0% at 3 years, 11.3% at 4 years, and 13.1% at 5 years. The cumulative second recurrence rate was 3.2% at 1 year, 12.6% at 2 years, 22.7% at 3 years, 31.2% at 4 years, and 38.0% at 5 years. The cumulative third recurrence rate was 4.8% at 1 year, 20.3% at 2 years, 39.1% at 3 years, 54.6% at 4 years, and 64.9% at 5 years. The cumulative second and third recurrence rates were relatively high and gradually increased with time (Fig. 2.) As age increased, the rate of CBD stone recurrence increased proportionally (p < 0.0001) (Fig. 3.) Based on age of under 50 years, the relative risk (RR) for CBD stone recurrence was 3.175 in patients in their 50–59 years, 4.558 in patients in their 60–69 years, and 5.762 in patients ≥ 70 years (Table 1.) Common bile duct stone recurrence occurred in 10.64% (2572/24,170) of male patients and 12.07% (2656/22,011) of female patients, with the latter showing a higher recurrence rate (RR 1.121, p < 0.0001.)
Difference in the recurrence rate of CBD stones according to cholecystectomy in patients with GB stones
The GB stone group had 16,910 patients, the previous cholecystectomy group had 2244 patients, and the indeterminate GB group had 27,027 patients. In the GB stone group, 11,617 (68.7%) patients underwent cholecystectomy less than 3 months before or after CBD stone removal, whereas 5293 (31.3%) patients did not undergo cholecystectomy at the same period. In the GB stone group, the rate of cholecystectomy was 83.1% in patients < 50 years, 74.3% in patients in their 50–59 years, 72.1% in patients in their 60–69 years, and 55.2% in patients ≥ 70 years. Fewer cholecystectomies were performed in older patients (Table 2.)
During the follow-up period, CBD stone recurrence occurred in 7.92% (920/11,617) in the cholecystectomy group and in 14.60% (773/5293) in the non-cholecystectomy group. The recurrence rate of CBD stones was significantly higher in the non-cholecystectomy group than in the cholecystectomy group, based on the Kaplan–Meier survival curve (RR 1.961, 95% CI 1.783–2.158, log-rank test p < 0.0001) (Fig. 4.) In the analysis according to age, the cumulative recurrence rate at all ages was significantly higher in the non-cholecystectomy group (p < 0.001 at all ages) (Fig. 4.) The RR for CBD stone recurrence in the non-cholecystectomy group compared with the cholecystectomy group was 3.198 in patients < 50 years, 2.371 in patients in their 50–59 years, 1.618 in patients in their 60–69 years, and 1.262 in patients ≥ 70 years. In the non-cholecystectomy group, younger age was associated with higher RR for CBD stone recurrence (Table 3.)
Kaplan–Meier curves showed the 1-recurrence rate of CBD stones in the cholecystectomy and non-cholecystectomy groups of the GB stone group (cholecystectomy group, solid line; non-cholecystectomy group, dashed line): a all ages (log-rank p < 0.0001), b < 50 years (log-rank p < 0.0001), c 50–59 years (log-rank p < 0.0001), d 60–69 years (log-rank p < 0.0001), and e ≥ 70 years (log-rank p = 0.0002)
Discussion
In this study using a national database of health insurance claims in Korea, we demonstrated the recurrence rate of CBD stones after endoscopic stone removal and the difference in the recurrence rate of CBD stones according to cholecystectomy in patients with GB stones.
Several studies reported recurrence rates of CBD stones ranging from 2 to 22% [1,2,3,4,5,6,7,8,9]. The difference in recurrence rate may be due to sample size, follow-up duration, and study design. There was no consensus as to whether the patients should be followed up after CBD stone removal. Although careful follow-up for recurrence was suggested for high-risk patients [1, 2, 13], there was a lack of evidence for this recommendation. Whether patients with risk factors for recurrence should be managed differently is uncertain [11]. Thus, before deciding whether to perform follow-up for recurrence, an accurate understanding of the recurrence rate should be made first.
Until now, the study of CBD stone recurrence was considered difficult. Because most patients are asymptomatic after stone removal, long-term follow-up is impossible. Furthermore, some patients may leave the hospital during follow-up. Most of all, a very large number of patients must be followed up for a fairly long period to show statistically significant results. Most of the previous studies have shown short-term follow-up results in a relatively small number of patients. For these reasons, we believed that a population-based database, using national health insurance database, would be very useful in the study of CBD stone recurrence. The NHIS database represents the entire Korean population and can be used as a population-based database [25].
Our study included 46,181 patients, with a mean follow-up duration of 4.2 years. This patient number is much higher compared with that of previous studies. Our results showed that the overall recurrence rate of CBD stones was 11.3%. The recurrence rate of CBD stones increased more with the number of recurrences. In this study, the cumulative recurrence rate of CBD stones was 2.2% at 1 year and 6.0% at 2 years. The recurrence rate within 2 years was very low, and there was no period when the recurrence rate increased distinctly. Although older age was associated with increased risk for CBD stone recurrence, the cumulative recurrence rate at 2 years in patients ≥ 70 years was only 7.7%. With these results, a regular follow-up within 2 years seems to have low clinical benefit. Practically, regular follow-up after 2 years or more would be difficult to be perceived by patients who are almost asymptomatic. Moreover, although the recurrence rate after 3–5 years had been increasing, it was very low. Therefore, we do not recommend regular follow-up for CBD stone recurrence in patients who have undergone removal of CBD stones for the first time regardless of age, but patients should be advised to return if symptoms recur.
Ando et al. [1] reported that in patients with recurrent CBD stones, CBD stones developed three or more times in 44%, and they recommended careful follow-up in these patients. In addition, Cheon et al. [11] only recommended periodic follow-up in patients with recurrence. In our studies, once CBD stones recurred, the next recurrence rate increased in proportion to the number of recurrence. Moreover, the recurrence rates increased steadily over time. Therefore, after CBD stone recurrence, we recommend follow-up the patients periodically. It would be advisable to follow-up every 1–2 years. The methods of follow-up may include serum liver test, non-invasive imaging study such as ultrasonography, computed tomography, and/or endoscopic retrograde cholangiopancreatography, with the follow-up method being decided by the institution or physician.
After CBD stone removal, another problem that has to be considered is whether to perform cholecystectomy in patients with intact GB with or without GB stones. Patients without GB stones have a lower recurrence rate than in patients with GB stones. The GB is helpful in washing away bile, in preventing new stone formation, and/or in flushing out newly produced stones [26]. Therefore, prophylactic cholecystectomy in patients without GB stones is generally not recommended [1, 27, 28]. Although cholecystectomy has often been recommended in younger or middle-aged patients with GB stones, prophylactic cholecystectomy in patients with GB stones after CBD stone removal remains controversial.
In a prospective study, recurrent biliary symptoms were mainly biliary pain and cholecystitis, which were more common in the wait-and-see group than in the cholecystectomy group (47 vs. 2%) and for whom the authors recommended cholecystectomy [15]. In another prospective study, further biliary events after CBD stone removal developed more frequently in patients with GB in situ than in patients receiving cholecystectomy (24 vs. 7%) [16]. The most common biliary event in both groups was cholangitis, for which the authors recommended cholecystectomy after CBD stone removal, such as in the previous report. However, in a recent prospective study, cholecystectomy after CBD stone removal failed to reduce additional recurrent cholangitis, and the authors suggested that cholecystectomy should be limited to patients with symptomatic GB stones [18]. Furthermore, several retrospective studies have shown different results on this issue [12, 13, 17, 19, 20, 28].
In this analysis of the difference in the recurrence rate of CBD stones according to cholecystectomy in patients with GB stones, the recurrence rate in the non-cholecystectomy group was higher than that in the cholecystectomy group. The RR for CBD stone recurrence in the non-cholecystectomy group was higher at younger ages. Thus, increasing age was associated with decreased RR. In general, the risk of developing typical biliary pain in asymptomatic patients with GB stones was 10–25% (2.0–2.6% per year) [29,30,31,32,33]. Considering the risk for CBD stone recurrence and the duration of life possibly developing biliary pain or cholecystitis, we recommend cholecystectomy in patients < 70 years with GB stones to reduce the possibility of CBD stone recurrence as well as cholecystitis, and it is strongly recommended for relatively younger patients. However, since the RR in over 70 years was only 1.2, it would be reasonable to decide the cholecystectomy at age over 70 years considering the risk of operation and the comorbid illness of the patient. Our findings were similar to the report of Yasui et al. [34] that cholecystectomy does not decrease biliary events and should not be recommended in very elderly patients.
Our study is the first nationwide population-based assessment of recurrent CBD stones. The strength of this study is the use of a very large and high-quality data set. Because most recurrent CBD stones were removed by endoscopic procedure, the recurrence of CBD stones defined as having undergone this procedure was able to represent almost all cases. Our study also had several limitations. Previous studies reported the risk factors for CBD stone recurrence after endoscopic stone removal. The risk factors were stone size and number, use of lithotripsy, presence of periampullary diverticulum, CBD diameter, and bile duct stenosis [1,2,3, 11,12,13,14]. Careful regular follow-up has been often recommended in patients with risk factors. However, the risk factors for recurrence of CBD stones are not thoroughly defined and the results were different for each study. In case of CBD diameter, the criterion for dilated CBD varied from 10 to 15 mm depending on the study [2, 12,13,14]. The detailed medical records of the patients are not included in the NHIS database, unfortunately. Hence, the medical information for these risk factors was unavailable. The inability to analyze the risk factors for CBD stone recurrence could be an important limitation of this study. Further studies are needed to determine whether regular follow-up is required in selected groups with high-risk factors.
Another limitation was that the diagnosis of CBD stone recurrence was based on the insurance database for procedure registry of endoscopic stone removal. Although endoscopic stone removal would be performed in most patients after detection of CBD stone recurrence, there might be some patients who did not receive this procedure due to several reasons. Therefore, it is possible that the recurrence rate of CBD stones might be slightly underestimated. Another limitation was our inability to obtain information on GB status in many patients. Among 46,181 patients, the indeterminate GB group had 27,027 patients. The lack of information on GB might be mostly in patients without GB stones. However, we have to consider the possibility of missing the registry of GB stone diagnosis, especially if it was not the main issue. Nevertheless, the GB stone group included 16,910 patients, which was high enough to yield significant results. Finally, Koreans have a higher rate of primary pigment stones than Westerners; thus, the applicability of our finding to the Western population is limited.
In conclusion, since the first recurrence rate of CBD stones was relatively low at all ages, regular follow-up in patients with endoscopic stone removal for the first time is not routinely recommended. However, once CBD stones recurred, the next recurrence rate increased with the number of recurrence, and we recommend regular follow-up for patients with recurrent stones. Cholecystectomy is recommended in patients < 70 years with GB stones after CBD stone removal to reduce CBD stone recurrence; however, cholecystectomy in patients ≥ 70 years must be considered carefully because they have relatively low RR for stone recurrence and possible high surgical comorbidity.
Abbreviations
- CBD:
-
Common bile duct
- CI:
-
Confidence interval
- GB:
-
Gallbladder
- KCD:
-
Korean Classification of Disease
- NHIS:
-
National Health Insurance Service
- RR:
-
Relative risk
References
Ando T, Tsuyuguchi T, Okugawa T, et al. Risk factors for recurrent bile duct stones after endoscopic papillotomy. Gut. 2003;52:116–21.
Sugiyama M, Atomi Y. Risk factors predictive of late complications after endoscopic sphincterotomy for bile duct stones: long-term (more than 10 years) follow-up study. Am J Gastroenterol. 2002;97:2763–7.
Jakobs R, Hartmann D, Kudis V, et al. Risk factors for symptomatic stone recurrence after transpapillary laser lithotripsy for difficult bile duct stones using a laser with a stone recognition system. Eur J Gastroenterol Hepatol. 2006;18:469–73.
Bergman JJGHM, van der Mey S, Rauws EAJ, et al. Long-term follow-up after endoscopic sphincterotomy for bile duct stones in patients younger than 60 years of age. Gastrointest Endosc. 1996;44:643.
Costamagna G, Tringali A, Shah S, et al. Long-term follow-up of patients after endoscopic sphincterotomy for choledocholithiasis, and risk factors for recurrence. Endoscopy. 2002;34:273–9.
Keizman D, Shalom MI, Konikoff FM. Recurrent symptomatic common bile duct stones after endoscopic stone extraction in elderly patients. Gastrointest Endosc. 2006;64:60–5.
Lai K, Lo G, Lin C, et al. Do patients with recurrent choledocholithiasis after endoscopic sphincterotomy benefit from regular follow-up? Gastrointest Endosc. 2002;55:523–6.
Prat F, Malak N, Pelletier G, et al. Biliary symptoms and complications more than 8 years after endoscopic sphincterotomy for choledocholithiasis. Gastroenterology. 1996;110:894–9.
Tanaka M, Takahata S, Konomi H, et al. Long-term consequence of endoscopic sphincterotomy for bile duct stones. Gastrointest Endosc. 1998;48:465–9.
Kim KY, Han J, Kim HG, et al. Late complications and stone recurrence rates after bile duct stone removal by endoscopic sphincterotomy and large balloon dilation are similar to those after endoscopic shincterotomy alone. Clin Endosc. 2013;46:637–42.
Cheon Y, Lehman G. Identification of risk factors for stone recurrence after endoscopic treatment of bile duct stones. Eur J Gastroenterol Hepatol. 2006;18:461–4.
Pereira-Lima JC, Jakobs R, Winter UH, et al. Long-term results (7–10 years) of endoscopic papillotomy for choledocholithiasis. Multivariate analysis of prognostic factors for the recurrence of biliary symptoms. Gastrointest Endosc. 1998;48:457–64.
Song ME, Chung MJ, Lee DJ, et al. Cholecystectomy for prevention of recurrence after endoscopic clearance of bile duct stones in Korea. Yonsei Med J. 2016;57:132–7.
Kim DI, Kim MH, Lee SK, et al. Risk factors for recurrence of primary bile duct stones after endoscopic biliary sphincterotomy. Gastrointest Endosc. 2001;54:42–8.
Boerma EJ, Boerma D, Rauws EA, et al. Wait-and-see policy or laparoscopic cholecystectomy after endoscopic sphincterotomy for bile-duct stones: a randomised trial. Lancet. 2002;360:761–5.
Lau JYW, Leow CK, Fung TM, et al. Cholecystectomy or gallbladder in situ after endoscopic sphincterotomy and bile duct stone removal in chinese patients. Gastroenterology. 2006;130:96–103.
Hammarström LE, Holmin T, Stridbeck H. Endoscopic treatment of bile duct calculi in patients with gallbladder in situ long-term outcome and factors predictive of recurrent symptoms. Scand J Gastroenterol. 1996;31:294–301.
Heo J, Jung M, Cho C. Should prophylactic cholecystectomy be performed in patients with concomitant gallstones after endoscopic sphincterotomy for bile duct stones? Surg Endosc. 2015;29:1574–9.
Lai K, Lin L, Lin C, et al. Does cholecystectomy after endoscopic sphincterotomy prevent the recurrence of biliary complications? Gastrointest Endosc. 1999;49:483–7.
Cui M, Cho J, Kim T. Long-term follow-up study of gallbladder in situ after endoscopic common duct stone removal in Korean patients. Surg Endosc. 2013;27:1711–6.
Kim DS. Introduction: health of the health care system in Korea. Soc Work Public Health. 2010;25:127–41.
Kim DS. Special issue on the national health care system of South Korea. Soc Work Public Health. 2010;25:125–6.
Park SY, Lee JY, Lim NG, et al. Incidence and prevalence of myasthenia gravis in Korea: a population-based study using the National Health Insurance Claims database. J Clin Neurol. 2016;12:340–4.
Kim KA, Ki M, Choi HY, et al. Population-based epidemiology of primary biliary cirrhosis in South Korea. Aliment Pharmacol Ther. 2016;43:154–62.
Song SO, Jung CH, Song YD, et al. Background and data configuration process of a nationwide population-based study using the Korean national health insurance system. Diabetes Metab J. 2014;38:395–403.
Frossard JL, Hadengue A, Amouyal P, et al. Choledocholithiasis: a prospective study of spontaneous common bile duct stone migration. Gastrointest Endosc. 2000;51:175–9.
Tanaka M, Ikeda S, Yoshimoto H, et al. The long-term fate of the gallbladder after endoscopic sphincterotomy. Complete follow-up study of 122 patients. Am J Surg. 1987;154:505–9.
Kageoka M, Watanabe F, Maruyama Y, et al. Long-term prognosis of patients after endoscopic sphincterotomy for choledocholithiasis. Dig Endosc. 2009;21:170–5.
McSherry CK, Ferstenberg H, Calhoun WF, et al. The natural history of diagnosed gallstone disease in symptomatic and asymptomatic patients. Ann Surg. 1985;202:59–63.
Gracie WA, Ransohoff DF. The natural history of silent gallstones: the innocent gallstone is not a myth. N Engl J Med. 1982;307:798–800.
Friedman GD, Raviola CA, Fireman B. Prognosis of gallstones with mild or no symptoms: 25 years of follow-up in a health maintenance organization. J Clin Epidemiol. 1989;42:127–36.
Cucchiaro G, Rossitch JC, Bowie J, et al. Clinical significance of ultrasonographically detected coincidental gallstones. Dig Dis Sci. 1990;35:417–21.
Thistle JL, Cleary PA, Lachin JM, et al. The natural history of cholelithiasis: the National Cooperative Gallstone Study. Ann Intern Med. 1984;101:171–5.
Yasui T, Takahata S, Kono H, et al. Is cholecystectomy necessary after endoscopic treatment of bile duct stones in patients older than 80 years of age? J Gastroenterol. 2012;47:65–70.
Acknowledgements
This study used the National Health Insurance Service (NHIS) 2002–2013 database (NHIS-2017-1-022). The authors alone are responsible for the content and writing of the article.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
All authors have no conflicts of interest or financial ties to disclose.
Rights and permissions
About this article
Cite this article
Park, B.K., Seo, J.H., Jeon, H.H. et al. A nationwide population-based study of common bile duct stone recurrence after endoscopic stone removal in Korea. J Gastroenterol 53, 670–678 (2018). https://doi.org/10.1007/s00535-017-1419-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00535-017-1419-x