Abstract
Background
The use of simulation for laparoscopic training has led to the development of objective tools for skills assessment. Motion analysis represents one area of focus. This study was designed to assess the evidence for the use of motion analysis as a valid tool for laparoscopic skills assessment.
Methods
Embase, MEDLINE and PubMed were searched using the following domains: (1) motion analysis, (2) validation and (3) laparoscopy. Studies investigating motion analysis as a tool for assessment of laparoscopic skill in general surgery were included. Common endpoints in motion analysis metrics were compared between studies according to a modified form of the Oxford Centre for Evidence-Based Medicine levels of evidence and recommendation.
Results
Thirteen studies were included from 2,039 initial papers. Twelve (92.3 %) reported the construct validity of motion analysis across a range of laparoscopic tasks. Of these 12, 5 (41.7 %) evaluated the ProMIS Augmented Reality Simulator, 3 (25 %) the Imperial College Surgical Assessment Device (ICSAD), 2 (16.7 %) the Hiroshima University Endoscopic Surgical Assessment Device (HUESAD), 1 (8.33 %) the Advanced Dundee Endoscopic Psychomotor Tester (ADEPT) and 1 (8.33 %) the Robotic and Video Motion Analysis Software (ROVIMAS). Face validity was reported by 1 (7.7 %) study each for ADEPT and ICSAD. Concurrent validity was reported by 1 (7.7 %) study each for ADEPT, ICSAD and ProMIS. There was no evidence for predictive validity.
Conclusions
Evidence exists to validate motion analysis for use in laparoscopic skills assessment. Valid parameters are time taken, path length and number of hand movements. Future work should concentrate on the conversion of motion data into competency-based scores for trainee feedback.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Subjective methods of trainee assessment are no longer adequate for surgical training [1]. Reduced working hours [2, 3], increased demands from the political sector [4] and financial pressures [5] mean that more objective measures are required. Surgical simulation is an effective tool for training and assessment. Simulators can reduce learning curves outside the operating theatre in a pressure-free environment, without requiring formal supervision [6]. Studies show that skills acquired during simulation training are transferable to the operating room [7]. Simulation in laparoscopic training refers to a wide range of devices from simple box trainers [8], cadaveric models [9], live animals [10], to complex virtual reality (VR) systems (e.g. MIST-VR®, LapSim® ProMIS™, and LapMentor™) [11–14]. This has led to the development of simulator assessment tools which include motion analysis.
Motion analysis allows assessment of surgical dexterity using parameters that are extracted from movement of the hands or laparoscopic instruments [15]. Several different motion analysis systems have been developed (Table 1). This can be inbuilt within a simulator (e.g. ProMIS™) or as a separate device, enabling flexible use (e.g. Imperial College Surgical Assessment Device, ICSAD) [16]. Objective assessment of laparoscopic skill could be carried out using motion analysis if endpoints for each parameter are quantified according to pre-defined levels of experience. The conversion of motion analysis data into competency-based scores or indexes could provide a valuable source of trainee feedback [17]. This is an automatic and instant process [18]. Feedback could be useful on two levels, firstly by providing a quantitative index to define varying levels of experience, which trainees can work towards. Secondly, it could serve as evidence of professional development that is assessed at annual progress reviews. Before motion analysis can be used to assess laparoscopic competence, the technology and metrics measured must first be validated [19].
Validation of any new method for training or assessment is a critical step [20]. This is the extent to which an instrument measures what it was designed to measure [21, 22]. The process should begin by defining a “construct”, which defines the underlying trait for which a new training tool is designed [20]. The more forms of validity (Table 2) that are demonstrated, the stronger the overall argument [20].
The aims of this systematic review are to provide an overview of the different motion analysis technologies available for the assessment of laparoscopic skill, and to identify the evidence for their validity.
Methods
Data resources and search criteria
A systematic review was performed according to the Preferred Reporting Items for Systematic Review and Meta-Analyses (PRISMA) guidelines [23]. The literature search was conducted using the following databases: Embase Classic + Embase (1947 to 2011 week 38), MEDLINE (1947 to present) and PubMed. For each database we searched three domains of exploded MeSH keyword terms. The general terms for each domain were (1) motion analysis, (2) validation and (3) laparoscopy. Where a keyword mapped to further subject headings, those considered relevant were also exploded to maximise coverage of the literature. Studies published in a foreign language were translated into English [24]. The last search date was 29 September 2011. This search strategy was undertaken by two independent reviewers, and articles retrieved according to the inclusion criteria. Articles arising from cross-referencing were also included. Duplicate articles and those clearly unrelated to the inclusion criteria were excluded. Any disagreements between the reviewers were referred to a third party.
Inclusion and exclusion criteria
All studies investigating motion analysis as a valid tool for assessment of laparoscopic skill in general surgery were included. Inclusion criteria included: sufficient detail of motion analysis technology used (including information regarding the precise motion metrics measured), description of the tasks being investigated and the type of validity measured. Studies that validated laparoscopic simulators for which motion analysis did not form the primary method of assessment were excluded. Furthermore, studies were excluded if they were validating assessment tools in specialities other than general surgery and/or if motion analysis was being validated for laparoscopic training rather than assessment. Evidence validating motion analysis for laparoscopic training is limited, and its inclusion would lead to further study design heterogeneity. Review articles and conference abstracts were also excluded.
Outcome measures and analysis
Each of the studies included was rated according to a modified form of the Oxford Centre for Evidence-Based Medicine (CEBM) levels of evidence and recommendation [25, 26]. Information was extracted from each study in accordance to the inclusion criteria. Common endpoints between studies were identified and compared when statistically significant results were reported, the principle summary statistic being the difference in means or medians. It was judged that the data were not suitable for meta-analysis due to study design heterogeneity.
Results
The primary search identified 2,039 records. Three hundred and eighty-eight duplicates were removed, and the remaining 1,651 abstract records screened for relevance. Following this process, 1,522 records were excluded and 129 full-text articles obtained. Full-text review excluded a further 124 studies, while cross-referencing identified 8 studies. At the end of this process, 13 studies were included for review (Fig. 1). These studies investigated four different motion analysis devices: the Advanced Dundee Endoscopic Psychomotor Tester (ADEPT; two studies [27, 28]), the Hiroshima University Endoscopic Surgical Assessment Device (HUESAD; two studies [29, 30]), the Imperial College Surgical Assessment Device (ICSAD; three studies [9, 31, 32]), the ProMIS Augmented Reality Simulator (five studies [13, 33–36]) and the Robotic and Video Motion Analysis Software (ROVIMAS; one study [18]) (Table 3). No randomized controlled trials (RCTs) were identified. Twelve studies were graded at level 2b evidence [9, 13, 18, 28–36], and one study at level 3 [27].
PRISMA [23] flow diagram for selection of studies
Construct validity
Construct validity was examined in 12 (92.3 %) studies [9, 13, 18, 28–36]. There was a large degree of variation between studies, in terms of both group allocation and methodology (Table 4). Comparison between common endpoints (Table 5) was made in order to provide the following levels of recommendation (Table 6):
ADEPT: One study confirmed construct validity for the error score endpoint [28], when comparing novices and experts (level 3 recommendation).
HUESAD: Two studies established construct validity for the following endpoints: time taken to complete task [29, 30] (level 2 recommendation), deviation from ideal vertical and horizontal planes [29] and approaching time [30] (level 3 recommendation) when comparing novices and experts during a navigation task.
ICSAD: Three studies reported construct validity for the following endpoints: time (stage 1, 2 and 4 [9], tasks 1, 2, 3 and 4 [32]), number of hand movements (stage 1, 2 and 4 [9], task 1, 3 and 4 [32]) and path length (stage 1 and 2 [9], task 1 and 4 [32]) when comparing novices, intermediates and experts in the following tasks: laparoscopic cholecystectomy (LC) [9] and fundamentals of laparoscopic surgery (FLS) tasks [32] (all level 2 recommendations). Moorthy et al. [31] reported construct validity for time and path length in their laparoscopic suturing task when novices were compared with intermediates, and intermediates with experts. Two of the studies also demonstrated construct validity of overall expert rating scales that were used alongside motion analysis (level 2 recommendation) [31, 32].
ProMIS: Five studies established construct validity for the following endpoints: time [13, 33–36], path length [13, 34–36], smoothness of movement [13, 34–36] (level 2 recommendation) and number of hand movements [33] (level 3 recommendation) when comparing novices versus experts [13], novices versus intermediates versus experts [34, 35] or medical students/preregistration house officers (PRHOs) versus senior house officers versus surgical trainees versus consultants [33, 36] in various laparoscopic bench tasks. The tasks included suturing [13], orientation [33, 34, 36], object positioning [34, 36], knot tying [34] and sharp dissection [34–36].
ROVIMAS: One study confirmed construct validity for the following endpoints: time (overall, stage 1, 2 and 3), number of hand movements (stage 1) and path length (stage 1), when comparing novices and experts in a real-life LC [18] (level 3 recommendation). Number of hand movements and path length were both unable to distinguish between novices and experts in clipping and cutting the cystic duct (stage 2) and artery (stage 3), or during dissection (stage 4) [18].
Other validity types
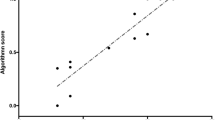
Face validity was reported by one study for ADEPT [27] and one study for ICSAD [9] (no data provided). Three studies reported concurrent validity [9, 27, 35]. Macmillan et al. state that for ADEPT a high correlation was seen between the number of perfect runs and blinded clinical assessments (Spearman’s rho 0.74) [27]. Concurrent validity was also confirmed by one study for ICSAD [31], and ProMIS [35], through the observation that motion analysis metrics correlated with expert and global rating scores (ICSAD: path length, Spearman’s rho –0.78, p = 0.000; ProMIS: time and path length, Spearman’s rho 0.88, p < 0.05) (all level 3 recommendations). None of the 13 studies included in this systematic review investigated content or predictive validity.
Discussion
This study presents the evidence for the use of motion analysis in laparoscopic skills assessment. A previous review by van Hove et al. [15] assessed a range of objective tools available to assess surgical skill, including motion analysis. However, this did not provide information regarding the precise surgical skill assessed, nor did it provide subsequent levels of recommendation. The authors included studies validating the TrEndo Tracking System, which so far has only been studied in obstetrics and gynaecology trainees [37, 38]. These studies have produced promising results, and we recommend further studies investigating its application within general surgery. Carter et al. [26] published consensus guidelines concerning evidence rating and subsequent levels of recommendation for evaluation and implementation of simulators and skills training programmes [25, 26]. The authors produced an alternative system due to the absence of published validation studies that have rigorous experimental methodology [26]. Our review utilises this version of the CEBM system, and actual levels of recommendation for each tool have been provided for the first time (Table 6).
This review reports construct validity for a range of different motion analysis metrics across three different training environments (VR [13, 33–36], laboratory based [9, 28–32] and the operating theatre [18]). The most commonly validated metrics were time to complete a task, path length and number of hand movements. One ICSAD study attempted to establish construct validity for velocity during a simulated porcine LC model [9]. Velocity is a function of time and path length, both of which were also measured. However, while velocity was found to largely lack construct validity, this was not the case for time and path length. Smith et al. explain this by stating that each movement made by experienced surgeons is more efficient, meaning that, while the speed of movements is not significantly quicker, instead they are more goal directed so that tasks are completed in less time [9]. Despite only being a metric measured by the ProMIS simulator, smoothness of movements was also consistently shown to discriminate between different levels of experience [13, 33–36].
Aggarwal et al. [39] state the importance of breaking down training and assessment into basic, intermediate and advanced stages. It could be suggested that ADEPT and HUESAD could be used to assess basic training as they utilise simple orientation and movement skills in a non-anatomical environment. ICSAD, ProMIS and ROVIMAS could be used to assess intermediate competence. There are animal tissue models and virtual reality simulators that exist for a range of general surgery procedures that could be used in conjunction with these motion analysis technologies. This has already been demonstrated in a porcine model for LC [9], and adaptations to the devices may enable their use in endoscopy training. The flexibility of use offered by ICSAD and ROVIMAS means that advanced competency could be assessed. Construct validity during a real-life LC has already been demonstrated for ROVIMAS [18].
This systematic review also showed that very few forms of validity are being examined apart from construct. The more forms of validity that are demonstrated, the stronger the overall argument for the use of a particular technology [20]. While two studies report face validity [9, 27], no expert rating data were provided to support this. It may not be possible to face-validate motion analysis technology, as any attempt to do so would be assessing the realism of the laparoscopic set-up instead. While it is important to establish construct validity for each endpoint and in every procedure that motion analysis may eventually be used to assess, its practical use in real-life assessment is limited. Predictive validity represents a more useful modality to investigate, and it is unfortunate that there have been no studies undertaken to investigate this.
The main limitation of this review is the degree of methodological variation between included studies, which prevented meta-analysis. The largest degree of variation was seen for group allocation, which was largely based on career grades, although most studies used further inclusion criteria within each grade based on varying levels of laparoscopic experience. This limitation is explained by the fact that number of procedures performed is a non-objective measure of experience. A more objective approach to group allocation could have been made on the basis of Objective Structured Assessment of Technical Skills (OSATS) scoring. A further limitation is that the majority of the studies included compared groups across wide ranges of experience (e.g. novice versus intermediate versus expert), where outcomes may be largely dependent on the novice versus expert element of this analysis. Motion analysis must demonstrate the sensitivity to discriminate between all individual grades if it is to be used to assess laparoscopic competence.
Motion analysis does carry some limitations which require discussion. Firstly, many of the devices require calibration to account for individual physiological tremor. This may require technical support during each procedure. Additionally, there is the issue of cost, which may prevent widespread use across all training centres.
In order for motion analysis to be used as an assessment tool it must be shown to work in a real-life environment. While the feasibility of using motion analysis in a real-life operating theatre has been demonstrated for ICSAD [40] and ROVIMAS [18], the correlation between motion analysis assessment in the laboratory and its subsequent use within the operating theatre needs to be evaluated. Quantitative assessment outcomes must be shown to be equivalent between different training environments, otherwise the application of motion analysis to provide trainee feedback is undermined.
Using motion analysis in isolation may remove the user from the context of the operating theatre. As surgical competence is multimodal, it is important that assessment is not only based on specific outcomes (such as dexterity) but also global outcomes, such as task accuracy and outcome. This is made possible through the dual application of motion analysis alongside global checklists [e.g. Global Operative Assessment of Laparoscopic Skills (GOALS) and Objective Structured Assessment of Technical Skills (OSATS)] [41]. Furthermore, procedure-specific rating scales have also been developed to assess specific technical aspects of different operations, including LC [42] and Nissen fundoplication [43]. Using these systems, assessment can either occur “live”, whilst a trainee is undertaking a specific task [44]. Several studies included in this review included global rating scores, which were found to correlate with motion analysis metrics [18, 31, 35].
It has been suggested that surgery is 75 % decision-making and 25 % dexterity [45]. While motion analysis may provide a promising tool to assess dexterity, it cannot provide information on the numerous attributes that contribute to the other three-quarters of a good surgeon’s skill set. Further work is needed to correlate motion analysis against similarly validated measurements of surgical decision-making in different scenarios.
Conclusions
We have demonstrated that there is evidence validating the use of motion analysis to assess laparoscopic skill. The most valid metrics appear to be time, path length and number of hand movements. More work is needed to establish predictive validity for each of these metrics. Future work should concentrate on the conversion of motion analysis data into competency-based scores or indices for trainee feedback.
References
Darzi A, Smith S, Taffinder N (1999) Assessing operative skill. Using these systems, assessment. BMJ 318:887–888
Chesser S, Bowman K, Phillips H (2002) The European Working Time Directive and the training of surgeons. BMJ 325:S69
Donohoe C, Sayana M, Kennedy M, Niall D (2010) European Time Directive: implications for surgical training. Ir Med J 103:57–59
Smith R (1998) All changed, changed utterly: British medicine will be transformed by the Bristol case. BMJ 316:1917–1918
Bridges M, Diamond D (1999) The financial impact of teaching surgical residents in the operating room. Am J Surg 177:28–32
Munz Y, Kumar B, Moorthy K, Bann S, Darzi A (2004) Laparoscopic virtual reality and box trainers. Is one superior to the other? Surg Endosc 18:485–494
Sturm L, Windsor J, Cosman P, Cregan P, Hewett P, Maddern G (2008) A systematic review of skills transfer after surgical simulation training. Ann Surg 248(2):166–179
Chung J, Sackier J (1998) A method of objectively evaluating improvements in laparoscopic skills. Surg Endosc 12:1117–1120
Smith S, Torkington J, Brown T, Taffinder N, Darzi A (2002) Motion analysis. A tool for assessing laparoscopic dexterity in the performance of a laboratory-based laparoscopic cholecystectomy. Surg Endosc 16:640–645
Clayden G (1994) Teaching laparoscopic surgery. Preliminary training on animals is essential. BMJ 309:342
Wilson M, Middlebrooke A, Sutton C, Stone R, McCloy R (1997) MIST-VR: a virtual reality trainer for laparoscopic surgery assesses performance. Ann R Coll Surg Engl 79:403–404
Larson A (2001) An open and flexible framework for computer aided surgical training. Stud Health Technol Inform 81:263–265
Van Sickle K, McClusky DI, Gallagher A, Smith C (2005) Construct validation of the ProMIS simulator using a novel laparoscopic suturing task. Surg Endosc 19:1227–1231
McDougall E, Corica F, Boker J, Sala L, Stoliar G, Borin J, Chu F, Clayman R (2006) Construct validity testing of a laparoscopic surgical simulator. J Am Coll Surg 202(5):779–787
van Hove P, Tuijthof G, Verdaasdonk E, Stassen LP, Dankelman J (2010) Objective assessment of technical surgical skills. Br J Surg 97:972–987
Datta V, Mackay S, Darzi A, Gillies D (2001) Motion analysis in the assessment of surgical skill. Comput Methods Med Biomed Eng 4:515–523
Aggarwal R, Hance J, Darzi A (2004) Surgical education and training in the new millenium. Surg Endosc 18:1409–1410
Aggarwal R, Grantcharov T, Moorthy K, Milland T, Papasavas P, Dosis A, Bello F, Darzi A (2007) An evaluation of the feasibility, validity, and reliability of laparoscopic skills assessment in the operating room. Ann Surg 245(6):992–999
Thijssen A, Schijven M (2010) Contemporary virtual reality laparoscopy simulators: quicksand or solid grounds for assessing surgical trainees? Am J Surg 199:529–541
Sedlack R (2011) Validation process for new endoscopy teaching tools. Tech Gastro Endosc 13:151–154
Feldman L, Sherman V, Fried G (2004) Using simulators to assess laparoscopic competence: ready for widespread use? Surgery 135:28–42
Technical skills education surgery (2011). http://www.facs.org/education/technicalskills/faqs/faqs.html. Accessed 8 Oct 2011
The PRISMA (2011). http://www.prisma-statement.org/index.htm. Accessed 1 Oct 2011
Google Translate (2011). http://translate.google.com/. Accessed 30 Sept 2011
Oxford Centre for Evidence Based Medicine—Levels of Evidence (2011). http://www.cebm.net/index.aspx?o=1025. Accessed 30 Sept 2011
Carter F, Schijven M, Aggarwal R, Grantcharov T, Francis N, Hanna G, Jakimowicz J (2005) Work group for evaluation and implementation of simulators and skills training programmes. Consensus guidelines for validation of virtual reality surgical simulators. Surg Endosc 19:1523–1532
Macmillan A, Cuschieri A (1999) Assessment of innate ability and skills for endoscopic manipulations by the advanced Dundee endoscopic psychomotor tester: predictive and concurrent validity. Am J Surg 177:274–277
Francis N, Hanna G, Cuschieri A (2002) The performance of master surgeons on the advanced Dundee endoscopic psychomotor tester. Arch Surg 137:841–844
Egi H, Okajima M, Yoshimitsu M, Ikeda S, Miyata Y, Masugami H, Kawahara T, Kurita Y, Kaneko M, Asahara T (2008) Objective assessment of endoscopic surgical skills by analyzing direction-dependent dexterity using the Hiroshima University endoscopic surgical assessment device (HUESAD). Surg Today 38:705–710
Tokunaga M, Egi H, Minoru H, Yoshimitsu M, Sumitani D, Kawahara T, Okajima M, Ohdan H (2011) Approaching time is important for assessment of endoscopic surgical skills. Min Invasive Ther Allied Technol 21:142–149
Moorthy K, Munz Y, Doris A, Bello F, Chang A, Darzi A (2004) Bimodal assessment of laparoscopic suturing skills: construct and concurrent validity. Surg Endosc 18:1608–1612
Xeroulis G, Dubrowski A, Leslie K (2009) Simulation in laparoscopic surgery: a concurrent validity study for FLS. Surg Endosc 23:161–165
Broe D, Ridgway P, Johnson S, Tierney K, Conlon K (2006) Construct validation of a novel hybrid surgical simulator. Surg Endosc 20:900–904
Oostema J, Abdel M, Gould J (2008) Time-efficient laparoscopic skills assessment using an augmented-reality simulator. Surg Endosc 22:2621–2624
Pellen M, Horgan L, Barton J, Attwood S (2009) Laparoscopic surgical skills assessment: can simulators replace experts? World J Surg 33:440–447
Pellen M, Horgan L, Barton J, Attwood S (2009) Construct validity of the ProMIS laparoscopic simulator. Surg Endosc 23:130–139
Chmarra M, Kolkman W, Jansen F, Grimbergen C, Dankelman J (2007) The influence of experience and camera holding on laparoscopic instrument movements measured with the TrEndo tracking system. Surg Endosc 21:2069–2075
Chmarra M, Klein S, de Winter J, Jansen F-W, Dankelman J (2010) Objective classification of residents based on their psychomotor laparoscopic skills. Surg Endosc 24:1031–1039
Aggarwal R, Moorthy K, Darzi A (2004) Laparoscopic skills training and assessment. Br J Surg 91:1549–1558
Doris A, Aggarwal R, Bello F, Moorthy K, Munz Y, Gillies D, Darzi A (2005) Synchronized video and motion analysis for the assessment of procedures in the operating theater. Arch Surg 140:293–299
Martin J, Regehr G, Reznick R, MacRae H, Murnaghan J, Hutchinson C, Brown M (1997) Objective Structured Assessment of Technical Skill (OSATS) for surgical residents. Br J Surg 84:273–278
Eubanks T, Clements R, Pohl D, Williams N, Schaad D, Horgan S, Pellegrini C (1999) An objective scoring system for laparoscopic cholecystectomy. J Am Coll Surg 189:566–574
Dath D, Regehr G, Birch D, Schlachta C, Poulin E, Mamazza J, Reznick R, MacRae H (2004) Toward reliable operative assessment: the reliability and feasibility of videotaped assessment of laparoscopic technical skills. Surg Endosc 18(12):1800–1804
Moorthy K, Munz Y, Sarker S, Darzi A (2003) Objective assessment of technical skills in surgery. BMJ 327:1032–1037
Spencer F (1978) Teaching and measuring surgical techniques—the technical evaluation of competence. Bull Am Coll Surg 63:9–12
FLS program (2011). http://www.flsprogram.org. Accessed 9 Oct 2011
Acknowledgments
J. Ansell is currently funded by a Royal College of Surgeons England research fellowship grant.
Disclosures
Authors John D. Mason, James Ansell, Neil Warren and Jared Torkington have no conflicts of interest or financial ties to disclose.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Mason, J.D., Ansell, J., Warren, N. et al. Is motion analysis a valid tool for assessing laparoscopic skill?. Surg Endosc 27, 1468–1477 (2013). https://doi.org/10.1007/s00464-012-2631-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00464-012-2631-7