Abstract
Background
Minimally invasive liver resection (MILR) for colorectal liver metastases (CRLM) is gaining widespread acceptance. However, data are still lacking on the feasibility, long- and short-term outcomes of laparoscopic major hepatectomy (i.e., three or more liver segments).
Methods
Between October 2002 and December 2008, prospectively collected data of 117 patients who underwent major liver resection [97 open (OMLR) and 20 laparoscopic (LMLR) procedures] for CRLM were analyzed. Twenty patients in the LMLR group were matched with 20 patients of the OMLR based on 13 parameters. We compared the long- and short-term outcomes between these two groups.
Results
Median duration of surgery was 257.5 (range 75–360) min in LMLR versus 232.5 (range 120–400) min in OMLR (P = 0.228). Median blood loss during surgery was 550 ml in each group (range 100–4,000 vs. 100–2,500 ml, P = 0.884). There was no statistically significant difference in the rate of postoperative complications (both severity and location). Median magnitude of tumor-free resection margin was 7.5 versus 5.5 mm in the laparoscopy versus open group, respectively (P = 0.651). Median disease-free survival (DFS) of the entire study population was 18.4 months [95% confidence interval (CI) 11.9–50.0 months]. Median overall survival (OS) was 50.7 months (95% CI 36.2 months to undetermined). The estimated DFS and OS rates at 1, 2, and 5 years were comparable in the two groups (P = 0.637 and 0.872, respectively).
Conclusion
Laparoscopic MLR for selected CRLM is feasible and might result in comparable oncologic outcomes as in open liver resection.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Along with the use of more effective chemotherapy regimens, advances in surgical techniques have prolonged the survival of patients with colorectal liver metastases (CRLM). At present, liver resection is considered the standard treatment for patients with CRLM and can be performed with low morbidity and minimal mortality rates [1–4]. Since the introduction of minimally invasive techniques, hepatobiliary surgeons from selected expert centers have reported laparoscopic liver resection to be safe and feasible for CRLM [5–7]. Advantages of minimally invasive liver surgery (MILS) over open surgery are reduced tissue damage, surgical trauma, and immunosuppression. Various studies showed the beneficial influence of MILS on the short-term outcome after surgery for CRLM [8–12]. However, studies evaluating the feasibility, long- and short-term outcomes of laparoscopic major liver resection (i.e., resection of three or more liver segments) are limited [8–11].
The aim of the present study is to evaluate the clinical and oncologic outcome of patients who underwent laparoscopic major liver resection (LMLR) for CRLM.
Patients and methods
Patient population
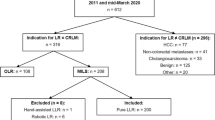
Between October 2002 and December 2008, we prospectively collected data of 117 patients who underwent major liver resection for CRLM. Open major liver resection (OMLR) was performed in 97 patients, while 20 patients underwent LMLR. All patients in the LMLR group were matched with 20 patients in the OMLR group based on 13 parameters: Fong’s Clinical Risk Score (CRS) [1], age, sex, ASA score, location of the liver metastasis (right/left liver), previous liver resection, previous local ablative therapy (LAT), simultaneous colorectal resection, simultaneous local ablative therapy, pre- and postoperative chemotherapy, pre- and postoperative biological therapy. There were no significant differences in patient characteristics between the two groups (Table 1).
Follow-up
Follow-up of patients was ended in September 2011, with median follow-up time after liver surgery of 43.4 months (range 5.5–102 months). After hospital discharge, follow-up information was obtained by way of reviewing patients’ hospital charts that were prospectively recorded in our institution’s electronic database. Patients were assessed for disease recurrence using clinical examination and the following investigations: biochemistry including serum carcinoembryonic antigen level, contrast-enhanced computed tomography (CT) and/or magnetic resonance imaging (MRI) of the abdomen and thorax performed every 3–4 months. Over the last 2 years we performed combined (PET/CT) whole-body positron emission tomography scan with 18-fluoro-2-deoxyglucose instead of conventional CT or MRI scan.
Surgical procedure
One hepatobiliary surgeon (B.T.) performed all laparoscopic major liver resections, while two surgeons (R.A., B.T.) were responsible for open liver resections. All procedures were assisted with intraoperative ultrasonography. Pringle maneuver was used in four patients in each group. Simultaneous colorectal resection was performed in three patients of each group.
All MILR procedures were performed totally laparoscopically, without hand assistance. Anatomical right or left hepatectomy was accomplished using the intrahepatic Glissonian approach, in which the biliary anatomy was verified using intraoperative cholangiography before portal pedicle transection, as described earlier [13]. A six-trocar approach was used combined with a 30° 5-mm laparoscope. A 12-mm trocar was placed at the umbilicus and in the right flank. A 5-mm trocar was positioned in the left flank, the right and left hypochondria, and under the xiphoid process. In all LMLR procedures the precise position of the trocars was determined by the patient’s abdominal constitution. To prevent occurrence of clinically significant gas embolism, intra-abdominal pressure (CO2 pneumoperitoneum) was kept as low as possible, aiming for 6–8 mmHg during liver parenchymal transection. Major vessels were controlled with endoscopic vascular devices or endoclips. Hepatic parenchymal transection was accomplished using bipolar diathermy, a tissue sealing device, and ultrasonic aspirator. The resection specimen was extracted in an endobag through a suprapubic (Pfannenstiel) incision, measuring maximum 10 cm in length, which was also used for the colonic/rectal anastomosis.
Outcome measures
The perioperative outcome was evaluated in terms of duration of surgery, intraoperative blood loss, postoperative complications, postoperative mortality, and length of hospital stay (LOS). Severity of complications was classified according to therapy-oriented severity grading system (TOSGS) score [14]. Complications were allocated to surgical-site (SSC) and non-surgical-site complications (NSSC). The oncological outcome was evaluated through assessment of completeness of tumor removal (pR), magnitude of pathological resection margin (pRM), and overall (OS) and disease-free (DFS) survival rates.
Statistical analysis
Statistical analysis was carried out using JMP software version 9.0.0. Comparisons of continuous variables were performed using the Mann–Whitney U test. For categorical variables, comparisons were made using Fisher’s exact test. Survival rates were analyzed using the Kaplan–Meier method (log-rank test). P values smaller than 0.05 were considered statistically significant.
Results
Clinical outcome
In both LMLR and OMLR groups the median number of tumors was two, and the number of resected liver segments was four. Anatomical resections were performed in 17 patients of the LMLR versus 13 of the OLMR group. Anatomical bisegmentectomies were combined with nonanatomical segmental hepatectomies in three of the LMLR versus seven of the OMLR group. Simultaneous LAT of CRLM was performed in five patients via laparoscopy versus three patients via open surgery (Table 2). No statistically significant differences were observed in perioperative outcome measures between the two groups (Table 3). Median operating time was 238 (range 75–400) min and blood loss 550 ml (range 100–4,000 ml). No postoperative mortality occurred. Seven patients developed postoperative complications in each group. Neither the severity nor the location of complications was different between the two groups. Although statistically not different, most severe complications (TOSGS ≥3) were observed in patients who underwent simultaneous resection of their primary colorectal cancer, i.e., 1/3 in the OMLR and 3/3 in the LMLR group. The median postoperative LOS was 8 days (range 5–51 days).
In all patients, pain medication consisted of patient-controlled intravenous analgesia using opioids by means of an infusion pump during the first 3 days after surgery. Intravenous paracetamol was used on a systematic basis immediately after surgery until no pain medication was needed. Oral liquid or food intake was started when patients felt ready for it. Patients’ pain score was not registered systematically in the current study.
Oncologic outcome
The median of the magnitude of tumor-free resection margin (pRM) was 7.5 mm in the LMLR group versus 5.5 mm in the OMLR group (P = 0.651). Surgical resection margins of the resection specimen showed tumor involvement in one patient of each group (pR1) (Table 3).
Median DFS of the entire study population was 18.4 months [95% confidence interval (CI) 11.9–50.0 months]. Median OS was 50.7 months (95% CI 36.2 months to undetermined). The estimated DFS and OS rates in the LMLR group at 1, 2, and 5 years were 60, 49, and 43 and 90, 80, and 48% respectively. Survival rates did not differ significantly between patients in the OMLR versus LMLR group (P ≥ 0.637) (Figs. 1, 2).
Discussion
The oncologic outcome of patients with CRLM continues to ameliorate as more effective chemotherapy regimens are combined with enhanced surgical techniques. Currently, the preferred treatment of CRLM is open surgical resection. However, laparoscopic surgeons from specialized centers have treated selected patients via minimally invasive techniques. The safety, feasibility, and efficacy of laparoscopically performed major (three or more segments) hepatic resections for CRLM are not clear. Hemorrhage from portal or hepatic veins is the major concern determining the postoperative outcome and is the main reason for conversion to open surgery. Although reported for the first time in 1998, introduction of LMLR has progressed slowly worldwide due to the technically demanding aspect of the procedure and surgeons’ concern about its oncologic aspects [15].
The present study focusing on LMLR in matched patients with CRLM suggests that minimally invasive or laparoscopic major hepatectomy may be a valuable alternative treatment for selected patients. Indeed, both short- and long-term outcomes were similar in the matched patient groups undergoing LMLR versus OMLR. Postoperative complication rate, intraoperative blood loss, duration of surgery, and LOS were comparable in the two groups. Severe postoperative complications (TOSGS grade ≥3) occurred mainly in patients who underwent simultaneous hepatic and colorectal resection, but the current study population is rather small to draw final conclusions with respect to this observation. One would have expected shorter LOS after laparoscopy as compared with open surgery, though in the present study the LOS is mainly determined by the extent of the surgical procedure (major hepatic resection +/− colorectal resection), the absence of any standardized enhanced recovery protocol after surgery, and the patients’ lack of willingness to be discharged from hospital early after a high-risk surgical procedure.
In the current study, completeness of tumor resection (pR and pRM) as well as patient survival seemed to be comparable in the two groups. On histopathological examination the surgical resection margin was not tumor free in one patient from both groups. These two patients had undergone liver resection (one laparoscopic right hepatectomy, one open left hepatectomy) for three metastases that showed major clinical response after neoadjuvant systemic chemotherapy and bevacizumab. Therefore, to obtain complete tumor-free resection margins in patients presenting major tumor shrinkage after systemic chemotherapy, larger macroscopic margins might be necessary whenever possible.
No data are available on the oncologic outcome of only major LLR for CRLM, whereas four retrospective studies analyzed the outcome of CRLM after minor and major LLR together. Of these, the numbers of patients who underwent LMLR in the two single-center studies were 0 and 8 [10, 11]. The two-center study contained 26 and the five-center study 32 patients who underwent LMLR [8, 9]. None of these authors performed separate analysis of this subgroup. As a result, there are no truly comparable studies in the literature. In the present study, we analyzed the immediate postoperative and long-term oncologic outcomes of patients with CRLM who underwent LMLR. These analyses showed that it is possible to perform major hepatectomy laparoscopically with the benefits of minimally invasive surgery and without losing the therapeutic efficacy of hepatic resection for CRLM. Taking into account the difference in the study populations, the 5-year OS and DFS in our series are comparable to those described in the other series [8–11].
Shortcomings of all reported studies so far, including the current one, are the small numbers of patients and their nonrandomized design. Our study is the first to compare the short- and long-term outcomes of matched patient groups undergoing either open or minimally invasive major hepatectomy for CRLM. To date, prospective randomized controlled trials comparing short- and long-term outcomes between laparoscopic and open liver resection do not exist. The reason for this may be the difficulty in enrolling patients into such a trial, because most patients will presumably refuse a potential open procedure as minimally invasive surgery gains increasingly broad acceptance and patients are aware of the immediate postoperative benefits (e.g., less pain) of laparoscopic surgery. Another explanation is the necessity of stratifying the study population for all potentially prognostic factors to evaluate the effect of laparoscopic liver resection on the outcome.
Major LLR may be efficacious in selected patients with CRLM. To make this possible, two points have to be taken into account. First, sufficient experience with minimally invasive liver surgery is needed because of the technically demanding nature of LMLR. Second, adequate patient selection is crucial. Therefore, the criteria for LLR have to be determined beforehand, and prior to any therapy every patient has to be discussed in a multidisciplinary way.
Conclusions
Laparoscopic major liver resection is safe and feasible in patients with colorectal liver metastases. Short- and long-term outcomes are comparable to those of open major liver resection, while patients benefit from the minimally invasive nature of laparoscopy. Multidisciplinary adequate patient selection and sufficient experience with minimally invasive surgery are mandatory. However, to confirm these results, a well-designed randomized controlled trial with larger study population has to be performed.
References
Fong Y, Fortner J, Sun RL, Brennan MF, Blumgart LH (1999) Clinical score for predicting recurrence after hepatic resection for metastatic colorectal cancer: analysis of 1001 consecutive cases. Ann Surg 230:309–318
Choti MA, Sitzmann JV, Tiburi MF, Sumetchotimetha W, Rangsin R, Schulick RD, Lillemoe KD, Yeo CJ, Cameron JL (2002) Trends in long-term survival following liver resection for hepatic colorectal metastases. Ann Surg 235:759–766
Pawlik TM, Scoggins CR, Zorzi D, Abdalla EK, Andres A, Eng C, Curley SA, Loyer EM, Muratore A, Mentha G, Capussotti L, Vauthey JN (2005) Effect of surgical margin status on survival and site of recurrence after hepatic resection for colorectal metastases. Ann Surg 241:715–722
Tomlinson JS, Jarnagin WR, DeMatteo RP, Fong Y, Gonen M, Kemeny N, Brennan MF, Blumagart LH, D’Angelica M (2007) Actual 10-year survival after resection of colorectal liver metastases defines cure. J Clin Oncol 25:4575–4580
Topal B, Fieuws S, Aerst R, Vandeweyer H, Penninckx F (2008) Laparoscopic versus open liver resection of hepatic neoplasms: comparative analysis of short-term results. Surg Endosc 22:2208–2213
Rocha FG, D’Angelica M (2010) Treatment of liver colorectal metastases: role of laparoscopy, radiofrequency ablation, and microwave coagulation. J Surg Oncol 102:968–974
Nguyen KT, Geller DA (2010) Outcomes of laparoscopic hepatic resection for colorectal cancer metastases. J Surg Oncol 102:975–977
Nguyen KT, Laurent A, Dagher I, Geller DA, Steel J, Thomas MT, Marvin M, Ravindra KV, Mejia A, Lainas P, Franco D, Cherqui D, Buell JF, Gamblin TC (2009) Minimally invasive liver resection for metastatic colorectal cancer. Ann Surg 250:842–848
Castaing D, Vibert E, Ricca L, Aoulay D, Adam R, Gayet B (2009) Oncologic results of laparoscopic versus open hepatectomy for colorectal liver metastases in two specialized centers. Ann Surg 250:849–855
Sasaki A, Nitta H, Otsuka K, Takahara T, Nishizuka S, Wakabayashi G (2009) Ten-year experience of totally laparoscopic liver resection in a single institution. Br J Surg 96:274–279
Kazaryan AM, Marangos IP, Røsok BI, Rosseland AR, Villanger O, Fosse E, Mathisen O, Edwin B (2010) Laparoscopic resection of colorectal liver metastases: surgical and long-term oncologic outcome. Ann Surg 252:1005–1012
Mulier S, Ni Y, Jamart J, Michel L, Marchal G, Ruers T (2008) Radiofrequency ablation versus resection for resectable colorectal liver metastases: time for a randomized trial? Ann Surg Oncol 15:144–157
Topal B, Aerts R, Penninckx F (2007) Laparoscopic intrahepatic Glissonian approach for right hepatectomy is safe, simple, and reproducible. Surg Endosc 21:2111
Dindo D, Demartines N, Clavien PA (2004) Classification of surgical complications: a new proposal with evaluation in a cohort of 6336 patients and results of a survey. Ann Surg 240:214–215
Huscher CG, Lirici MM, Chiodini S (1998) Laparoscopic liver resections. Semin Laparosc Surg 5:204–210
Disclosure
Authors H. Topal, J. Tiek, R. Aerts, and B. Topal have no conflicts of interest or financial ties to disclose.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Topal, H., Tiek, J., Aerts, R. et al. Outcome of laparoscopic major liver resection for colorectal metastases. Surg Endosc 26, 2451–2455 (2012). https://doi.org/10.1007/s00464-012-2209-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00464-012-2209-4