Abstract
In the era of multimodal management of liver metastases, surgical resection remains the only curative option, with open approach still being referred to as the standard of care. Currently, the feasibility and benefits of the laparoscopic approach for liver resection have been largely demonstrated. However, its oncologic adequacy remains to be confirmed. The aim of this study is to report the oncological results of laparoscopic liver resection for metastatic disease in a single-centre experience. A single-centre database of 413 laparoscopic liver resections was reviewed and procedures for liver metastases were selected. The assessment of oncologic outcomes included analysis of minimal tumour-free margin, R1 resection rate and 3-year survival. The feasibility and safety of the procedures were also evaluated through analysis of perioperative outcomes. The study comprised 209 patients (294 procedures). Colorectal liver metastases were the commonest indication (67.9 %). Fourteen patients had conversion (6.7 %) and oncological concern was the commonest reason for conversion (42.8 %). Median tumour-free margin was 10 mm and complete radical resections were achieved in 211 of 218 curative-intent procedures (96.7 %). For patients affected by colorectal liver metastases, 1- and 3-year OS resulted 85.9 and 66.7 %. For patients affected by neuroendocrine liver metastases, 1- and 3-year OS resulted 93 and 77.8 %. Among the patients with metastases from other primaries, 1- and 3-year OS were 83.3 and 70.5 %. The laparoscopic approach is a safe and valid option in the treatment of patients with metastatic liver disease undergoing curative resection. It does offer significant perioperative benefits without compromise of oncologic outcomes.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Liver metastatic disease is a relevant clinical problem. Nevertheless, liver metastases are associated with a poor prognosis and reduction in survival, which may range from only a few months to many years depending on different prognostic factors [1–3].
In the modern era, availability of loco-regional treatments and systemic therapies have led to significant improvement in survival, and multimodality strategies have now been established as the mainstay for the management of patients with liver metastases [4–6]. However, only surgical resection is associated with a survival plateau, thus being the only potentially curative option in appropriately selected patients [7]. Moreover, advances in surgical techniques and perioperative managements have reduced the contraindications for liver surgery and many surgeons would consider an aggressive approach in the management of metastatic liver disease [8]. Also, survival advantage has been documented after repeated resection for recurrent liver metastases. As a result, many patients are considered candidates for multiple potentially curative liver resections [9].
Over the last decades, the feasibility and safety of laparoscopy for liver resections have been documented for both minor and major hepatectomies along with its benefits in terms of lower postoperative morbidity and decreased hospital stay [10–13]. As a reflection, laparoscopic liver resections have undergone a gradual spread and have become a valid alternative to the traditional open approach in expert centres. However, this expansion has been relatively slow due to the perceived technical difficulties and concerns regarding the oncologic efficiency [14].
Randomized controlled trials are considered the peak of evidence-based medicine and, as such, have been advocated to confirm the validity of laparoscopic liver resection over the traditional open approach. On the other hand, these are hardly applicable owing to the difficulty in recruiting patients to be allocated to differently invasive procedures [15]. In this setting, further evidence may be provided by alternative levels of evidence, such as meta-analysis, comparative studies and large case-series reports [16–19].
The aim of this study is to report the results of laparoscopic liver resection for metastatic disease in a large single-centre experience to confirm the oncological adequacy of the minimally invasive approach in this challenging oncologic setting.
Methods
Study design
A prospectively collected single-centre database of 413 consecutive patients undergoing laparoscopic liver resections (August 2003–July 2013) at Southampton University Hospital was reviewed. Laparoscopic liver resections for benign and primary malignant tumours (i.e., hepatocellular carcinoma, cholangiocellular carcinoma, other primaries) were excluded. As a result, in this manuscript only laparoscopic liver resections for metastatic liver disease were considered.
The main endpoint of the study was the assessment of oncologic short- and mid-term outcomes in this series. This included analysis of surrogate endpoints (minimal tumour-free margin, R1 resection rate) and of 3-year survival. Mid-term survival analysis was calculated separately for patients affected by colorectal liver metastases (CRLM), neuroendocrine tumour liver metastases (NETLM) and metastases from other primaries, as the majority of patients affected by NETLM underwent palliative surgery with the intent of controlling secretory symptoms.
Resection margins were defined into R0 (microscopically more than 1 mm from resection margin) and R1 (microscopically less than 1 mm from resection margin). R2 resections were defined as partial resections with grossly visible tumour left behind (in the setting of debulking surgery for NETLM). Overall survival (OS) was estimated from laparoscopic liver resection until death, recurrence-free survival (RFS) from laparoscopic liver resection until the first documented recurrence of disease, and disease-free survival (DFS) defined as survival from laparoscopic liver resection until incurable recurrence. Actuarial survival was analysed in 1- and 3-year time interval for time-defined survival.
The feasibility and safety of the procedures were also evaluated through analysis of perioperative outcomes. These included conversion rate, reasons for conversion to open, duration of surgery, intraoperative blood loss, adoption and duration of Pringle Manoeuver, length of high dependency unit (HDU)/intensive care unit (ICU) stay, postoperative length of stay, morbidity and mortality rates within 90 days from surgery. Perioperative morbidity was classified according to the Accordion Severity Grading System of Surgical Complications [20].
The following variables were also analysed: demographics, indication for surgery, tumour size and type of liver resection (according to the Brisbane 2000 Nomenclature) [21].
Perioperative management
Routine blood tests, computed tomography of the abdomen with triphasic liver contrast enhancement or liver-specific double-contrast magnetic resonance imaging scanning were performed in all patients. All patients were discussed at an open multidisciplinary team (MDT) meeting attended by surgeons, pathologists, oncologists, gastroenterologists, and radiologists. The extent of the liver resection was decided in the MDT without any adjustment based on the surgical approach (laparoscopic/open). Initially, the criteria for considering a liver lesion unsuitable for laparoscopic resection were: tumours located within 2 cm from the portal vein bifurcation, inferior vena cava or hepatocaval vein confluence, and tumours involving the common bile duct. However, later with increasing experience, lesions near to major structures were approached as long as R0 resection was considered achievable.
Pure laparoscopic procedures were attempted in all patients. Our group has previously described in detail the techniques for left lateral sectionectomies, major hemi-hepatectomies and liver resections over the posterosuperior segments [22–25]. Intermittent Pringle Maneuver is performed during transection in the majority of cases, as described elsewhere [26].
Statistics
Statistical analysis was performed through SPSS ver. 16 (SPSS Inc., Chicago, IL, USA). Continuous variables were expressed as mean or median according to their values’ distribution (Shapiro–Wilk Test). The Kaplan–Meier method and life tables were adopted for survival analyses. RFS, DFS and OS were expressed as median number of months (95 % confidence interval) and actuarial survival as percentage. Statistical significance was set at p < 0.05.
Results
The study comprised 209 patients undergoing attempted laparoscopic liver resections within the study period. The median patients’ age resulted 66 years (range 32–85), with 54.6 % males (n = 114).
Indications for surgery and management approach
Colorectal liver metastases were the commonest indication (n = 142, 67.9 %), followed by NETLM (n = 43, 20.6 %). Remaining 24 patients were affected by non-colorectal, non-neuroendocrine liver metastases (11.5 %).
Patients affected by NETLM received liver resection with cytoreductive/palliative intent. All other patients were resected with a curative intent (n = 166, 79.4 %).
CRLM
Ninety of 142 patients were affected by metachronous metastases (63.4 %). Median time interval between diagnosis of primary tumour and liver metastases resulted 22 months (range 7–120). Neoadjuvant and adjuvant chemotherapy were administered in 26 (28.9 %) and 28 (31.1 %) patients, respectively.
Among patients presenting with synchronous CRLM (n = 52, 36.6 %), the majority was elected to a “colon first” approach, that is a two-stage procedure with colorectal resection performed firstly (n = 47, 90.4 %). “Liver first” approach and synchronous colorectal/liver resection were carried out in 5.8 % (n = 3) and 3.8 % (n = 2) of patients, respectively.
Management of metastatic liver disease consisted in one-stage approach for the majority of patients (n = 136, 95.8 %). The remaining 6 patients were elected to a two-stage approach (totally laparoscopic: 2 patients; 1st stage laparoscopic and 2nd stage open: 4 patients). One patient dropped out after the 1st stage hepatectomy since evidence of unresectable liver disease was documented at restaging.
NETLM
Midgut origin of NET primary was documented for the majority of patients (n = 25, 58.1 %), either located in the ileum or the ascending colon, while 8 patients were diagnosed with a pancreatic NET primary (18.6 %). The origin remained unknown for the remaining 10 patients (23.2 %).
Synchronous resection of primary tumour and liver metastases was carried out in 36.4 % of patients (n = 12), while a “liver first” approach was adopted for 8 patients (24.2 %).
Liver metastases from other primaries
Indications among this group included: melanoma metastases (7 patients, 3.3 %), metastatic GIST (5 patients, 2.4 %), breast cancer metastases (3 patients, 1.4 %), metastatic renal cancer (3 patients, 1.4 %), lung cancer metastases (2 patient, 0.9 %), ovarian tumour metastases (2 patients, 0.9 %), metastatic Ewing’s sarcoma (1 patient, 0.5 %), and metastatic acinar pancreatic cancer (1 patient, 0.5 %).
The majority of patients were affected by the metachronous disease (87.5 %). Median time interval between diagnosis of primary tumour and liver metastases resulted 36 months (range 12–180). The remaining 3 patients presented with synchronous liver metastases (12.5 %).
“Liver first” approach was adopted for 2 patients (24.2 %), while 91.7 % had a previous surgical procedure to resect the primary tumour (n = 22).
Surgical procedures
Fifty-nine of 209 patients had multiple concomitant liver resections (31.5 %) for a total of 294 procedures documented in this series.
Major hepatectomies accounted for 35.4 % of the liver resections performed (n = 74) including 51 right hepatectomies (24.4 %), 10 left hepatectomies (4.8 %), 7 extended right hepatectomies (3.3 %), 5 extended left hepatectomies (2.4 %) and 1 trisegmentectomy (0.5 %). Minor liver resections (n = 135, 64.6 %) comprised 50 left lateral sectionectomies (23.9 %), 4 right posterior sectionectomies (1.9 %), 9 bisegmentectomies (4.3 %), 13 single segmentectomies (6.2 %), 28 single wedge resections (13.4 %), and 31 multiple wedge resections (14.8 %). Fifteen of 74 major hepatectomies were associated with a concomitant minor liver resection (20.5 %).
Fourteen patients were converted to open (6.7 %). Oncological concerns at intraoperative stage (inability to assess the tumour extent, awkward tumour location at inspection, absence of neoplastic deposit at frozen section) resulted the commonest reason for conversion (n = 6, 42.8 %). Other reasons for conversion included: dense intra-abdominal adhesions (n = 3, 21.4 %), persistent bleeding during or at the end of transection (n = 3, 21.4 %), injury of small intestine at induction of pneumoperitoneum (n = 1, 7.1 %) and finding of bulky hilar nodal metastases at inspection (n = 1, 7.1 %). Data about the 10 patients converted prior to the transection phase were excluded from statistical analysis, as the liver resection was effectively carried out by open approach, for a total of 199 patients ultimately considered for statistics.
Perioperative outcomes
Median operative time resulted 220 min (range 30–710), and median blood loss 250 mL (range 10–3,200). Pringle Maneuver was required in 56 patients (26.7 %) with a median duration of 31 min (range 5–94). Median HDU stay and total stay resulted 1 and 4 days, respectively (range 1–10 and 1–52). Thirty-three patients experienced moderate to severe postoperative complications (15.7 % 90-day morbidity rate) for a total of 41 postoperative adverse events occurred in this series. Liver-related morbidity included 4 bile leaks (1 managed conservatively and 3 requiring Endoscopic Retrograde Cholangiopancreatography stenting) and 8 postoperative intra-abdominal collections treated with ultrasound-guided drainage. No postoperative liver failure was recorded. 90-day mortality rate resulted 1.4 % (n = 3). Causes of death included acute myocardial infarction (n = 1), postoperative portal vein thrombosis leading to liver failure (n = 1) and postoperative thrombosis of inferior vena cava associated with intra-abdominal collection (n = 1). Exhaustive description and classification of postoperative morbidity are provided in Table 1.
Oncological outcomes
Mean number of lesions was 2.1 (±1) and median tumour size 25 mm (range 4–150) on histological exam. Median tumour-free margin resulted 10 mm (range 1–80). Complete radical resections were achieved in 211 of 218 procedures carried out with curative intent (96.7 %) with R1 rate resulting 3.2 %. R1/R2 resections accounted for 32 of 76 procedures performed for NETLM metastases with cytoreductive/palliative indication (42.1 %). No port-site seeding was reported.
CRLM
The mean number of liver lesions in this group resulted 1.79 (SD 1.3, range 1–10) and median size was 26 mm (range 4–105 mm). Eighty-one of 142 patients were diagnosed with recurrence during postoperative follow-up (57.7 %) including 30 new liver recurrences and 1 recurrence at the transection edge (38.3 % of recurrence). Median RFS resulted 21 months (95 % confidence interval 15.6–726.3) and 1- and 3-year RFS were 54.2 and 29.4 %, respectively. Liver recurrence was managed with curative intent in 64.5 % of cases (15 repeated liver resection, 5 ultrasound-guided radiofrequency ablation) with median DFS finally resulting 29 months (95 % confidence interval 9.3–48.6) and 1- and 3-year DFS 56.3 and 43.1 %, respectively.
At follow-up, 53 of 142 patients were dead (37.3 %) with a 55-month median OS documented in this series (95 % confidence interval 33.7–76.3). 1- and 3-year OS resulted 85.9 and 66.7 %, respectively (Fig. 1).
NETLM and liver metastases from other primaries
Median OS for patients affected by NETLM was 74 months (95 % confidence interval 60.7–87.3) with 1- and 3-year OS resulting 93 and 77.8 %, respectively.
Among the 24 patients affected by non-colorectal, non-neuroendocrine liver metastases, 13 were alive at the time of follow-up (54.2 %), and 9 of them disease free. In this group, median OS resulted 48 months (95 % confidence interval 17.5–78.4) with 1- and 3-year OS 83.3 and 70.5 %, respectively.
Discussion
This study provides the outcomes of a single-centre series of laparoscopic liver resections for metastatic disease from different primary tumours. Our results confirm the validity of the laparoscopic approach in the treatment of liver metastatic disease with excellent oncologic outcomes, both in the short and mid term.
Longstanding debates about the oncologic adequacy of laparoscopic liver resection for malignant tumours are still ongoing [27]. These are mainly related to the fear of tumour involvement of resection margins as this is considered of major impact on the recurrence-free survival. Indeed, particularly in complex settings (unfavourable locations, multiple and large lesions), the absence of tactile feedback may represent a major difficulty in laparoscopic surgery, leading to the inadequate assessment of the extent of disease. Although we have previously suggested that the tumour size and distance from major vessels should not be considered an absolute contraindication to the laparoscopic approach, we herein emphasize again that those are complex resection and need of advanced laparoscopic experience before embarking in laparoscopic liver resection [28, 29]. Our findings confirm that oncological concerns at intraoperative stage resulted the commonest reason for conversion to open (42.8 %). Nevertheless, the 10 mm median tumour-free margin and 96.7 % R0 rate recorded in this series were satisfactory and consistent with results previously disclosed by others. A multi-institutional study on laparoscopic resections for colorectal liver metastases reported by Nguyen et al. [30] documented that negative margins were achieved in 94.4 % of resections with a 10 mm median tumour-free margin. Similarly, a more recent comparative study on laparoscopic versus open liver resections for colorectal metastases reported 87 % R0 resection rate and 5.2 mm median tumour-free margin in the laparoscopic group [31]. Although the optimal width of negative margin is still debated, especially for CRLM, complete tumour removal remains the gold standard of the surgical treatment of metastatic liver disease [32, 33]. The results documented in this series show that laparoscopic liver resections can be accomplished in accordance with the oncologic principles of radicality and contribute in supporting their oncological efficiency first of all from a technical standpoint. As in open surgery, intraoperative ultrasound plays a major role in this context [34]. Advanced skills in laparoscopic ultrasonography are essential in overcoming the lack of tactile feedback providing for adequate assessment of the location of disease and also detection of occult metastases. We do strongly advocate its adoption to decrease the rate of intraoperative margin re-resection or conversion to open.
Besides the satisfactory oncologic short-term results herein disclosed, mid-term survival outcomes have been evaluated in this series. Especially for CRLM, excellent long-term results with open surgery have been documented, with several centres reporting 5-year OS over 50 % and open liver resection being referred to as the standard of cure [32, 33]. In consideration of this, the bar for laparoscopic approach has been set relatively high. Nguyen et al. [30] recorded a 1- and 3-year OS of 88 and 69 %, respectively, on their multi-institutional series. More recently, Geller et al. documented comparable results in a meta-analysis including 242 laparoscopic liver resections for CRLM (1- and 3-year OS of 95.4 and 72.7 % respectively) [35]. Similarly, in this series 1- and 3-year OS resulted 85.9 and 66.7 %, respectively, with a median OS of 55 months (Fig. 1). When combined with results previously published by other centres, the survival rates herein reported support the evidence that the oncologic efficiency of laparoscopic liver resections for CRLM is not inferior to open approach and can provide comparable survival outcomes, even when concomitant colonic resection or multiple liver resections are performed.
The high rate of R1 resections for NETLM documented in this study (42.1 %) is due to the cytoreductive intent of surgery; in the majority of patients, surgery was performed in the context of an aggressive multimodality strategy including administration of somatostin analogues, chemoembolization, radioembolization and chemotherapy. In our experience, adequate selection of patients and multidisciplinary team approach are advisable in this setting, with resection being appropriate in the absence of extra hepatic metastases, diffuse bilobar involvement or compromised liver function, particularly for symptomatic disease and low-grade tumours.
Liver metastases from solid non-colorectal and non-neuroendocrine tumours are traditionally managed with chemotherapeutic regimens and local therapies other than surgery (i.e., ablative techniques, cryotherapy, transhepatic arterial chemoembolization, stereotactic radiotherapy). Indeed, the majority of patients who develop metastatic liver disease are incurable, and palliative systemic treatment is considered the most appropriate therapy [36, 37]. However, liver resection has been reported to be associated with long-term survival improvement in appropriately selected subsets of patients. In a systematic review of 19 studies involving 535 patients who underwent liver resection for metastatic breast cancer, median overall survival resulted 40 months (23–77 months) and 5-year OS 40 % [38]. In our experience, the decision to operate was made on a case-by-case basis and directed by a multidisciplinary team in the context of a multimodality strategy aimed to explore all treatment options to improve survival. Ideal candidates had limited number of liver metastases, no evidence of extra hepatic spread, long disease-free interval and biologically indolent disease. In this series, survival analysis performed on this subgroup of patients documented satisfactory outcomes, with 54.2 % of patients being alive at the time of follow-up and 83.3 % 3-year OS.
In addition to oncologic adequacy, we have also documented several short-term benefits of laparoscopic approach for liver resections. Intraoperative findings compared favourably with other series reporting that laparoscopic liver resections can be accomplished with acceptable operative times, blood losses and conversion rate [10–13]. In addition, patients herein included have experienced a favourable postoperative course, as shown by the relatively low morbidity rate (15.7 %) and postoperative length of stay (4 days) reported. These data are even more favourable taking into consideration that laparoscopic major hepatectomies and multiple concomitant liver resections were highly represented in this series (35.4 and 31.5 % respectively). These findings contribute in supporting the evidence that the safety of laparoscopic liver resections is not compromised even when technically demanding procedures are performed, provided being carried out by expert hands. In the modern context of multimodality strategies for the management of metastatic liver disease, faster recovery from surgery represents a major advantage of laparoscopic approach, allowing an early start of adjuvant treatments.
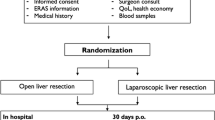
No randomized clinical trials into laparoscopic versus open liver resection have been published so far. The randomized Oslo-CoMet study (NCT01516710) has been planned to provide level 1 evidence on laparoscopic versus open resection for CRLM and is currently recruiting patients [39]. Waiting for its results to be published, the present study contributes with further evidence on this topic. In conclusion, the laparoscopic approach represents a safe and appealing option for patients affected by metastatic liver disease elected to surgical resection, as can provide significant perioperative benefits without compromise of oncologic outcomes.
References
Siegel RL, Miller KD, Jemal A (2015) Cancer statistics. CA Cancer J Clin 65(1):5–29
Stuart-Harris R, Shadbolt B, Palmqvist C, Chaudri Ross HA (2009) The prognostic significance of single hormone receptor positive metastatic breast cancer: an analysis of three randomised phase III trials of aromatase inhibitors. Breast 18(6):351–355
Moltzer RJ, Mazumdar M, Bacik J, Berg W, Amsterdam A, Ferrara J (1999) Survival and prognostic stratification of 670 patients with advanced renal cell carcinoma. J Clin Oncol 17(8):2530–2540
Kopetz S, Chang GJ, Overman MJ, Eng C, Sargent DJ, Larson DW, Grothey A, Vauthey JN, Nargoney DM, McWilliams RR (2009) Improved survival in metastatic colorectal cancer is associated with adoption of hepatic resection and improved chemotherapy. J Clin Oncol 27(22):3677–3683
Reddy SK, Zorzi D, Lum YW, Barbas AS, Pawlik TM, Ribero D, Abdalla EK, Choti MA, Kemp C, Vauthey JN, Morse MA, White RR, Clary BM (2009) Timing of multimodality therapy for resectable synchronous colorectal liver metastases: a retrospective multi-institutional analysis. Ann Surg Oncol 16(7):1809–1819
Gordon AC, Gradishar WJ, Kaklamani VG, Thuluvath AJ, Ryu RK, Sato KT, Gates VL, Salme R, Lewandowski RJ (2014) Yttrium-90 radioembolization stops progression of targeted breast cancer liver metastases after failed chemotherapy. J Vasc Interv Radiol 25(10):1523–1532
Tomlinson JS, Janargin WR, DeMatteo RP, Fong Y, Kornprat P, Gonen M, Kemeny N, Brennan MF, Blumgart LH, D’Angelica M (2007) Actual 10-year survival after resection of colorectal liver metastases defines cure. J Clin Oncol 25(29):4575–4580
Khatri VP, Petrelli NJ, Belghiti J (2005) Extending the frontiers of surgical therapy for hepatic colorectal metastases: is there a limit? J Clin Oncol 23(33):8490–8499
Tuttle TM, Curley SA, Roh MS (1997) Repeat hepatic resection as effective treatment of recurrent colorectal liver metastases. Ann Surg Oncol 4(2):125–130
Tranchart H, Di Giuro G, Lainas P, Pourcher G, Devaquet N, Perlemuter G, Franco D, Dagher I (2013) Laparoscopic liver resection with selective prior vascular control. Am J Surg 205(1):8–14
Kazaryan AM, Rosok BI, Marangos IP, Rosseland AR, Edwin B (2011) Comparative evaluation of laparoscopic liver resection for posterosuperior and anterolateral segments. Surg Endosc 25(12):3881–3889
Aldrighetti L, Guzzetti E, Pulitanò C, Cipriani F, Catena M, Paganelli M, Ferla G (2010) Case-matched analysis of totally laparoscopic versus open liver resection for HCC: short and middle term results. J Surg Oncol 102(1):82–86
Di Fabio F, Samim M, Di Gioia P, Godeseth R, Pearce NW, Abu Hilal M (2014) Laparoscopic major hepatectomies: clinical outcomes and classification. World J Surg 38(12):3169–3174
Gagner M, Rogula T, Seizer D (2004) Laparoscopic liver resection: benefits and controversies. Surg Clin North Am 84(2):451–462
Lassen K, Hoye A, Myrmel T (2012) Randomised trials in surgery: the burden of evidence. Rev Recent Clin Trials 7(3):244–248
Schiffman SC, Kim KH, Tsung A, Marsh JW, Geller DA (2015) Laparoscopic versus open liver resection for metastatic colorectal cancer: a metaanalysis of 610 patients. Surgery 157(2):211–222
Abu Hilal M, Underwood T, Zuccaro M, Primrose J, Pearce N (2010) Short- and medium-term results of totally laparoscopic resection for colorectal liver metastases. Br J Surg 97(6):927–933
Cheung TT, Poon RT, Yuen WK, Chok KS, Tsang SH, Yau T, Chan SC, Lo CM (2013) Outcome of laparoscopic versus open hepatectomy for colorectal liver metastases. ANZ J Surg 83(11):847–852
Hasegawa Y, Nitta H, Sasaki A, Takahara T, Itabashi H, Katagiri H, Otsuka K, Nishizuka S, Wakabayashi G (2015) Long-term outcomes of laparoscopic versus open liver resection for liver metastases from colorectal cancer: a comparative analysis of 168 consecutive cases at a single center. Surgery doi:10.1016/j.surg.2015.01.017 [Epub ahead of print]
Strasberg SM, Linehan DC, Hawkins WG (2009) The accordion severity grading system of surgical complications. Ann Surg 250(2):177–186
Strasberg SM (2005) Nomenclature of hepatic anatomy and resections: a review of the Brisbane 2000 system. J Hepatobiliary Pancreat Surg 12:351–355
Pearce NW, Di Fabio F, Teng MJ, Syed S, Primrose JN, Abu Hilal M (2011) Laparoscopic right hepatectomy: a challenging, but feasible, safe and efficient procedure (How I do it). Am J Surg 202(5):52–58
Abu Hilal M, Pearce NW (2008) Laparoscopic left lateral sectionectomy: a safe, efficient, reproducible technique. Dig Surg 25(4):305–308
Pearce NW, Di Fabio F, Abu Hilal M (2011) Laparoscopic left hepatectomy with extraparenchymal inflow control. J Am Coll Surg 213(5):23–27
Abu Hilal M, Badran A, Di Fabio F, Pearce NW (2011) Pure laparoscopic en bloc left hemihepatectomy and caudate lobe resection in patients with intrahepatic cholangiocarcinoma. J Laparoendosc Adv Surg Tech A 21(9):845–849
Abu Hilal M, Di Fabio F, Abu Salameh M, Pearce NW (2012) Oncological efficiency analysis of laparoscopic liver resection for primary and metastatic cancer. Arch Surg 147(1):42–48
Wakabayashi G et al (2015) Recommendations for laparoscopic liver resection: a report from the second international consensus conference held in morioka. Ann Surg 261(4):619–629
Abu Hilal M, van der Poel MJ, Samim M, Besselink MG, Flowers D, Stedman B, Pearce NW (2015) Laparoscopic liver resection for lesions adjacent to major vasculature: feasibility, safety and oncological efficiency. J Gastrointest Surg 19(4):692–698
Shelat VG, Cipriani F, Basseres T, Armstrong TH, Takhar AS, Pearce NW, Abu Hilal M (2014) Pure laparoscopic liver resection for large malignant tumours: does size matter? Ann Surg Oncol Nov 8 PMID: 25380686
Nguyen KT, Laurent A, Dagher I, Geller DA, Steel J, Thomas MT, Marvin M, Ravindra KV, Mejia A, Lainas P, Franco D, Cherqui D, Buell JF, Gamblin TC (2009) Minimally invasive liver resection for metastatic colorectal cancer: a multi-institutional, international report of safety, feasibility and early outcomes. Ann Surg 250(5):842–848
Montalti R, Berardi G, Laurent S, Sebastiani S, Ferdinande L, Libbrecht LJ, Smeets P, Brescia A, Rogiers X, de Hemptinne B, Geboes K, Troisi R (2014) Laparoscopic liver resection compared to open approach in patients with colorectal liver metastases improves further resectability: oncological outcomes of a case-control matched-pairs analysis. Eur J Surg Oncol 40(5):536–544
Bodingbauer M, Tamandl D, Schmid K, Plank C, Schima W, Gruenberger T (2007) Size of surgical margin does not influence recurrence rates after curative liver resection for colorectal cancer liver metastases. Br J Surg 94:1133–1138
Dhir M, Lyden ER, Wang A, Smith LM, Ullrich F, Are C (2011) Influence of margins on overall survival after hepatic resection for colorectal metastasis: a meta-analysis. Ann Surg 254:234–242
Ferrero A, Lo Tesoriere R, Russolillo N, Viganò L, Forchino F, Capussotti L (2015) Ultrasound-guided laparoscopic liver resections. Surg Endosc 29(4):1002–1005
Schiffman SC, Kim KH, Tsung A, Marsh JW, Geller DA (2015) Laparoscopic versus open liver resection for metastatic colorectal cancer: a metaanalysis of 610 patients. Surgery 157(2):211–222
Samuels BL, Chawla S, Patel S, von Mehren M, Hamm J, Kaiser PE, Schuetze S, Li J, Aymes A, Demetri GD (2013) Clinical outcomes and safety with trabectedin therapy in patients wih advanced soft tissue sarcomas following failure of prior chemotherapy: results of a worldwide expanded access program study. Ann Oncol 24(6):1703–1709
Mauri D, Polyzos NP, Salanti G, Pavlidis N, Ioannidis JP (2008) Multiple-treatements meta-analysis of chemotherapy and targeted therapies in advanced breast cancer. J Natl Cancer Inst 100(24):1780–1791
Chua TC, Saxena A, Liauw W, Chu F, Morris DL (2011) Hepatic resection for metastatic breast cancer: a systematic review. Eur J Cancer 47(15):2282–2290
Fretland AA, Kazaryan AM, Bjornbeth BA, Flatmark K, Andersen MH, Tonnessen TI, Bjornlev GM, Fagerland MW, Kristiansen R, Oyri K, Edwin B (2015) Open versus laparoscopic liver resection for colorectal liver metastases (the Oslo-CoMet study): sudy ptotocol for a randomized controlled trial. Trials 16(1):73
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical Standard
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Research involving human participants and/or animals
This article does not contain any studies with human participants or animals performed by any of the authors.
Informed consent
For this type of study formal consent form is not required.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Cipriani, F., Rawashdeh, M., Ahmed, M. et al. Oncological outcomes of laparoscopic surgery of liver metastases: a single-centre experience. Updates Surg 67, 185–191 (2015). https://doi.org/10.1007/s13304-015-0308-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s13304-015-0308-1