Abstract
Background
Aggressive treatment of intrahepatic recurrence of hepatocellular carcinoma (HCC) increases patients’ survival. This study aimed to evaluate laparoscopic thermal ablation (TA) in the treatment of intrahepatic HCC recurrences.
Methods
A retrospective analysis was performed on 88 patients (REC group) who underwent laparoscopic TA after prior TA (66 patients.) or partial hepatic resection (HR) (22 patients) as initial local treatment. Another 170 patients with primary HCC tumors (PRIM group) were regarded as the control group.
Results
The postoperative morbidity rates were similar for the patients with prior TA (18%) and those with prior HR (21%) (nonsignificant difference [NS]). The overall survival rates were not significantly different between the two groups (3-year survival rates of 59 and 78%, respectively; P = 0.1662). Moreover, the disease-free survival (DFS) rates did not differ significantly between the patients with prior TA and those with prior HR (3-year DFS of 21 and 8%, respectively; P = 0.1911). The incidences of morbidity in the whole REC (21%) and PRIM (20%) groups were similar (P = NS), and no mortality occurred in either group (0%). The cumulative 3-year survival rate was 63% in the REC group and 59% in the PRIM group (P = 0.5739), whereas the 3-year DFS rate was 17% in the REC group and 22% in the PRIM group (P = 0.5266).
Conclusion
Laparoscopic TA can be performed safely and may be effective for intrahepatic HCC recurrence after prior TA or HR. It leads to survival and DFS rates similar to those obtained using laparoscopic TA for primary HCC without increasing morbidity. Laparoscopic TA could be proposed as first-line treatment of intrahepatic HCC recurrence for selected patients.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Hepatic resection (HR) still is considered the most promising first-choice therapeutic option for hepatocellular carcinoma (HCC) because the application of orthotopic liver transplantation is limited due to a shortage of donor organs and long waiting times [1, 2]. Unfortunately, as many as 50–70% of patients who initially undergo HR or thermal ablation (TA) for HCC will experience a recurrence in the remnant liver within 5 years [3–5]. To date, salvage HR has been the preferred treatment for intrahepatic recurrence, resulting in further prolongation of survival [5, 6]. However, only approximately 20–30% of these patients with intrahepatic recurrence are suitable for HR because of multiple recurrences, reduced liver function reserve, or comorbidities [7–9]. Such patients usually undergo transcatheter arterial chemoembolization, percutaneous ethanol injection therapy, or both [10, 11].
Recently, percutaneous TA has been increasingly performed to treat intrahepatic recurrent HCC after HR or TA [12]. However, as a consequence of previous therapies, unexpected injuries to the adjacent organs or lesions difficult to target remain critical problems after TA using a percutaneous approach [13]. In such cases, on the basis of our experience, the laparoscopic approach could be a suitable alternative therapy [4, 14].
This retrospective study aimed to evaluate the long-term survival results and complications of laparoscopic TA for recurrent HCC after HR or TA and to assess whether its long-term therapeutic results are comparable with those obtained for patients with primary HCC treated by laparoscopic TA.
Methods
We analyzed a prospective database collection of cirrhotic patients with HCC treated by laparoscopic TA at a single institution between December 1997 and November 2010. All the patients referred to our unit with the diagnosis of HCC underwent an assessment of the disease staging with a preestablished protocol until 2000 [4, 15]. The protocol then was updated according to the Barcelona Clinic Liver Cancer (BCLC) criteria [16].
This study analyzed only stage A patients. In stage A, a single lesion with a diameter up to 5 cm and both normal portal pressure and bilirubin is classified as A1. The same lesion with increased portal pressure (hepatic vein pressure gradient >10 mmHg, esophageal varices detectable on endoscopy, or splenomegaly [major diameter > 12 cm] with a platelet count <100,000/mm3) is classified as A2. The same lesion with both increased portal pressure and abnormal bilirubin is classified as A3, and two or three lesions 3 cm in diameter or smaller in a patient with Child-Pugh A-B class cirrhosis with no symptoms or normal performance status is classified as A4.
All patients were discussed in a weekly multidisciplinary meeting at which surgeons, hepatologists, and radiologists exchanged opinions. The diagnosis of HCC was based on appropriate imaging studies including a triple-phase computed tomography (CT) scan, a magnetic resonance scan, or both according to the Barcelona-2000 European Association for the Study of the Liver (EASL) Conference and a histologic assessment when required [17].
Otherwise, the possibility of liver transplantation (when liver function impairment was predominant) or HR was evaluated first. When none of these approaches was feasible (HR was proposed if a resection of fewer than 2 segments was possible), the patients were evaluated for laparoscopic or percutaneous interstitial therapy, the latter for patients at high surgical risk. When the HCC characteristics exceeded these values in nodule size or number, transarterial chemoembolization was preferred. Patients were proposed for laparoscopic TA if they fulfilled all the following criteria at presentation:
-
Large tumors (but with a diameter smaller than 5 cm) or multiple lesions (fewer than 3 nodules with a diameter no greater than 3 cm) requiring repeated punctures
-
Child-Pugh class A-B
-
Superficial lesions adjacent to visceral structures that could be displaced by laparoscopic maneuvers
-
Deep-sited lesions necessitating a very difficult or impossible percutaneous approach
-
Severe impairment of the coagulation tests (platelets <40,000 and/or International Normalized Ratio [INR] > 1.20).
During this period, 298 cirrhotic patients underwent laparoscopic TA. A total of 40 patients were excluded from the analysis for the following reasons: 17 patients due to recurrent HCC after transcatheter arterial chemoembolization, 11 patients due to BCLC stage exceeding stage A, and 12 patients due to treatment for a second or more recurrent HCC. Finally, 88 patients treated for intrahepatic HCC recurrence were enrolled in this study (REC group). Of these 88 patients, 66 had recurrent HCC after prior TA, and 22 had recurrent HCC after partial HR as initial local treatment. The remaining 170 patients (PRIM group) had laparoscopic TA as treatment of primary HCC and represented the control group of the analysis.
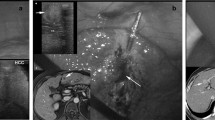
The laparoscopic TA technique has been described already in previous articles [14, 15]. Briefly, with the patient under general anesthesia, a laparoscopic ultrasound (LUS) examination of the liver was performed. All the patients underwent intraoperative ultrasound examination (Aloka SSD 500 [1996–1999], SSD 1700 [2000–2006], Alfa 10 [2006–2010]; Aloka Co, Tokyo).
For 220 patients, a 200-W, 480-KHz monopolar radiofrequency generator (Valleylab, Boulder, CO, USA) was used as the energy source. An insulated 18-gauge internally cooled electrode tip was inserted into the tumor under sonographic guidance. The shaft of this electrode is electrically insulated, with only 3–4 cm of exposed metallic tip from which the radiofrequency emanates. The electrode tips were selected by matching tip exposure to lesion diameter. Under LUS-guidance, the tip of the electrode was advanced until it reached and passed the margin of the lesion opposite the entry point of the needle.
A peristaltic pump was used to infuse 0°C normal saline solution into the cooling lumen of the radiofrequency electrode at a rate sufficient to maintain a tip temperature of 18–25°C. Repeated needle placements into the lesion to obtain maximal lesion coverage were performed when necessary. If the lesion was located near major biliary or portal vessels, a cooling technique was used: continuous infusion/perfusion of gauzes around the hepatic hilum with cold normal saline was performed during the radiofrequency ablation (RFA) procedure to cool the portal inflow and to prevent portal thrombosis and biliary damage.
From February 2009, a 2.45-MHz generator for microwave ablation (MWA) (AMICA-GEN, HS Hospital Service SpA, Aprilia, Italy) was used to deliver energy to 38 patients through a 14- or 16-gauge, internally cooled coaxial antenna. This generator features a miniaturized quarter-wave impedance transformer (referred to as a minichoke) for reflected wave confinement. The minichoke antenna design is protected by an industrial patent (PCT/IB2002/00299) owned by the Italian National Council for Research, which ensures a quasi-spherical radiation pattern while not increasing the probe gauge (14-gauge at the most).
According to the tumor size, a single microwave energy application ranging from 45 to 70 W net power at the applicator end was delivered to the patient for 5–10 min. Liver ultrasound and CT (and/or MRI) were performed within 1 month after treatment to assess the response to TA. The thermal ablation achieved “technique effectiveness” if a hypoattenuating area was seen on CT and this area was not enhanced after administration of contrast material (complete ablation), whereas an incomplete response to TA was defined as persistent nodular or marginal enhancement (partial ablation).
Posttreatment technique effectiveness was further evaluated by spiral CT after 3 months and every 6 months thereafter. Recurrence was defined as local tumor progression if a new enhancing lesion appeared within 2 cm of the treated nodule after complete ablation was confirmed on the first postablation CT scan. It was defined as distant if a new nodule arose at a site distant from the primary tumor. Intrahepatic HCC recurrence was classed as early or late using 9 months as the cutoff. A single experienced radiologist reviewed all the CT scans.
Statistical analysis
Cumulative actuarial curves were analyzed by the Kaplan–Meier method and compared by the log-rank test. Comparison of continuous variables between and within groups was performed with the Mann–Whitney U test and the Wilcoxon matched pairs test. Comparison of proportions was performed with Fisher’s exact probability test. Data following a normal distribution are expressed as mean ± standard deviation. For nonparametric data, the median and range are reported.
All analyses were two-tailed, and P values less than 0.05 were considered significant throughout the study. Initial evaluation and subsequent follow-up data were collected in a dedicated database (FileMaker Pro for Macintosh; FileMaker Inc, Santa Clara, CA, USA) and subsequently analyzed using Intercooled Stata 10.0 for Macintosh (College Station, TX, USA).
The hospital’s Ethics Committee approved the study, and written informed consent for recording and analysis of data was obtained from all the patients.
Results
The baseline characteristics of all the patients included in the study are illustrated in Table 1. In the REC group, only the model for end-stage liver disease (MELD) value and the presence of varices statistically differed between patients with HCC recurrence after either HR or TA, whereas the PRIM group had a higher mean age and larger HCC diameter than the REC group.
Table 2 shows the perioperative results for these patients. Due to the complexity of reoperation, laparoscopic TA required a longer operative time and hospital stay after HR than after TA. However, no differences were found between the REC and PRIM groups.
In the REC group, complete ablation (technique effectiveness) was obtained at 1 month for 57 of the 66 patients in the group after prior TA (86%) and for all patients after prior HR (100%) (nonsignificant difference). No differences were found between the REC group and the PRIM group. Complete ablation was obtained for 79 of 88 REC patients (90%) and 153 of 165 PRIM patients (93%) (nonsignificant difference).
After similar follow-up periods in these groups (median, 16 months after prior TA and 18 months after prior HR; 16 months in the REC group and 22 months in the PRIM group), similar HCC recurrences occurred in all the groups analyzed (Table 3), except that in the REC group, a slight difference was found in early recurrences between TA after HR (50%) and TA after TA (27%). However, local recurrences and the treatment of new HCC recurrences were not influenced by the different HCC or therapeutic groups.
Figures 1 and 2 show the actuarial survival curves. Neither the comparison between TA after HR and TA after TA nor the comparison between the REC group and the PRIM group showed any statistical differences. Similar results were obtained with the actuarial curves of disease-free survival (DFS) (Figs. 3, 4).
Discussion
The incidence of recurrence after treatment for HCC remains high, even with curative resection, thus representing the main cause of death [11, 18]. The remnant liver is the primary site of tumor recurrence, and the recurrence rate is 36.8–78%, as described in a recent systematic review [5].
Treatment for recurrent HCC includes HR, TA treatments, and transarterial therapy such as transcatheter arterial embolization [6–8, 12, 19–21]. Liver transplantation is another option for selected patients with impaired liver function [22, 23].
A few series of results from treatment of HCC recurrence after HR have been reported [5–10, 24]. Re-resection could safely be performed even for cirrhotic patients, with operative mortality and morbidity rates similar to those for a first HR. Re-resection is technically more demanding than primary HR because of anatomic disorientation due to rotation of the liver remnant, modifications in anatomic landmarks, postoperative adhesions causing protracted adhesiolysis, and difficult control of the portal inflow at the hepatoduodenal ligament [5, 9, 24]. This is particularly troublesome in cirrhotic patients, for whom the risk of bleeding is augmented. Therefore, only a few patients with recurrence are suitable for repeat HR, partly due to progressive deterioration of liver function in some patients with cirrhosis [25–27].
There are some reports on percutaneous TA for intrahepatic recurrent HCC. The easy repeatability and good tolerance of TA may help to prolong the survival of patients with recurrent HCC [12, 28–33]. For these patients, RFA is less expensive and less invasive, involving lower complication rates than surgical HR. However, with regard to completeness of tumor ablation, percutaneous TA probably is inferior to repeat HR, but further studies are necessary [34]. As in the case of repeat HR for recurrent HCC, a high incidence of intrahepatic distant recurrence can be expected after TA [35]. In fact, RFA is size dependent, so the upper limits must not exceed 2.5–3.0 cm to ensure complete necrosis. Recently, we have begun to evaluate the clinical application of MWA, with the goal of achieving larger areas of necrosis than with RFA.
On the other hand, if a percutaneous approach is used for patients with recurrent HCC, bowel damage is a potentially fatal condition when the tumor is located adjacent to the bowel due to fibrotic adhesions between the liver and bowel (heat diffusion) [13, 30, 36, 37]. Furthermore, adhesions may prevent good visualization of the recurrent HCC during ultrasound examination. Laparoscopic TA using either RFA or MWA technology could be a valid alternative approach to overcome the limitations of percutaneous access.
Our study indicated that no significant difference exists between the results for patients with recurrent HCC who had undergone previous HR or TA. The presence of several hypervascularized adhesions in cirrhotic patients makes laparoscopic reintervention for recurrent HCC very challenging [27]. The main difficulty with such an iterative approach is adhesiolysis, which has an impact on the total operative time and hospital stay. However, these technical difficulties do not affect intra- or postoperative morbidity, and all laparoscopic procedures were completed successfully without conversion.
Only a slight increase in early HCC recurrences was observed in the group treated after HR, probably because adhesions prevented a complete, accurate LUS exploration during the TA of the recurrence. The 3-year survival curves showed no statistically significant differences between TA (59%) and HR (78%); nor did the DFS curves (8% after HR vs. 24% after TA).
These findings were confirmed by analyzing the appearance of a new recurrent HCC. Once a recurrence had taken place, the two groups did not differ significantly with regard to the most common pattern of recurrence or treatment for recurrence after initial TA or HR for a primary HCC. In other words, laparoscopic TA can be performed successfully for recurrent HCC even after a previous HR, although that approach is more demanding in terms of total operative time and hospital stay after a previous HR than after a previous TA. We observed good long-term survival results comparable with those after previous TA, very low complication rates, and no procedure-related mortality in patients not eligible for repeat hepatectomy, including those treated through laparoscopic access [27] and selected patients with resectable tumors because after an incomplete response to TA, HR may be more technically challenging but still safe and effective [38].
Furthermore, the results for the group treated with laparoscopic TA for recurrent HCC were similar to those for the patients treated for primary HCC. During the hospital stay, no differences were found in terms of morbidity, total operative time, or hospital stay. This study demonstrates that the survival and DFS rates for patients treated with TA for recurrent HCC are similar to those for recurrence-free patients. These findings suggest that repeat laparoscopic TA for recurrent HCC could induce a survival benefit equivalent to that for patients without recurrence. These findings are similar to those obtained by repeat HR. Several studies have demonstrated no marked difference in survival after the initial and repeat hepatectomy [5–9, 21, 24–27], suggesting that repeat HR also is a safe, effective therapy for intrahepatic recurrence.
This study had some limitations. First, the number of patients with recurrent HCC in the study was relatively small, especially for the analysis of subgroups. Second, the mean follow-up period was significantly shorter for the REC group than for the PRIM group. This is secondary to the fact that the REC group involved the treatment of recurrent HCC occurring in the same PRIM group. Third, it was a retrospective study with all the inherent defects of such a study.
In conclusion, laparoscopic TA for recurrent HCC in cirrhotic patients is a safe, feasible procedure with good outcomes, even for patients with previous HR. It is a useful alternative to either percutaneous TA or repeated HR. However, the choice of local treatment for recurrent hepatic lesions should made after discussion by a multidisciplinary group, with the aim of refining the indications for each treatment to obtain the greatest benefit with the lowest risks.
References
Jarnagin WR (2010) Management of small hepatocellular carcinoma: a review of transplantation, resection, and ablation. Ann Surg Oncol 17:1226–1233
Llovet JM, Bruix J (2008) Novel advancements in the management of hepatocellular carcinoma in 2008. J Hepatol 48:S20–S37
Huang J, Yan L, Cheng Z, Hong Wu, Du L, Wang J, Xu Y, Zeng Y (2010) A randomized trial comparing radiofrequency ablation and surgical resection for HCC conforming to Milan criteria. Ann Surg 252:903–912
Santambrogio R, Opocher E, Zuin M, Selmi C, Bertolini E, Costa M, Conti M, Montorsi M (2009) Surgical resection versus laparoscopic radiofrequency ablation in patients with hepatocellular carcinoma and Child-Pugh class a liver cirrhosis. Ann Surg Oncol 16:3289–3298
Zhou Y, Sui C, Li B, Yin Z, Tan Y, Yang J, Liu Z (2010) Repeat hepatectomy for recurrent hepatocellular carcinoma: a local experience and a systematic review. World J Surg Oncol 8:55–65
Portolani N, Baiocchi GL, Coniglio A, Grazioli L, Frassi E, Gheza F, Giulini SM (2009) Sequential multidisciplinary treatment of hepatocellular carcinoma: the role of surgery as rescue therapy for failure of percutaneous ablation therapies. J Surg Oncol 100:580–584
Minagawa M, Makuuchi M, Takayama T, Kokudo N (2003) Selection criteria for repeat hepatectomy in patients with recurrent hepatocellular carcinoma. Arch Surg 238:703–710
Wu CC, Cheng SB, Yeh DC, Wang J, Peng FK (2009) Second and third hepatectomies for recurrent hepatocellular carcinoma are justified. Br J Surg 96:1049–1057
Nagano Y, Shimada H, Ueda M, Matsuo K, Tanaka K, Endo I, Kunisaki C, Togo S (2009) Efficacy of repeat hepatic resection for recurrent hepatocellular carcinomas. ANZ J Surg 79:729–733
Poon RTP, Fan ST, Lo CM, Liu CL, Wong J (1999) Intrahepatic recurrence after curative resection of hepatocellular carcinoma: long-term results of treatment and prognostic factors. Ann Surg 292:216–222
Umeda Y, Matsuda H, Sadamori H, Matsukawa H, Yagi T, Fujiwara T (2011) A prognostic model and treatment strategy for intrahepatic recurrence of hepatocellular carcinoma after curative resection. World J Surg 35:170–177
Okuwaki Y, Nakazawa T, Kokubu S, Hidaka H, Tanaka Y, Takada J, Watanabe M, Shibuya A, Minamino T, Saigenji K (2009) Repeat radiofrequency ablation provides benefit in patients with intrahepatic distant recurrence of hepatocellular carcinoma. Am J Gastroenterol 104:2747–2753
Livraghi T, Solbiati L, Meloni MF, Gazelle GS, Halpern EF, Goldberg SN (2003) Treatment of focal liver tumors with percutaneous radio-frequency ablation: complications encountered in a multicenter study. Radiology 226:441–451
Santambrogio R, Opocher E, Costa M, Cappellani A, Montorsi M (2005) Survival and intrahepatic recurrences after laparoscopic radiofrequency of hepatocellular carcinoma in patients with liver cirrhosis. J Surg Oncol 89:218–226
Santambrogio R, Costa M, Barabino M, Opocher E (2008) Laparoscopic radiofrequency of hepatocellular carcinoma using ultrasound-guided selective intrahepatic vascular occlusion. Surg Endosc 22:2051–2055
Llovet JM, Bru’ C, Bruix J (1999) Prognosis of hepatocellular carcinoma: the BCLC staging classification. Semin Liver Dis 19:329–338
Bruix J, Sherman M, Llovet JM, Beaugrand M, Lencioni R, Burroughs AK, Christensen E, Pagliaro L, Colombo M, Rodés J (2001) Clinical management of hepatocellular carcinoma. Conclusions of the Barcelona-2000 EASL Conference. J Hepatol 35:421–430
Ercolani G, Grazi GL, Ravaioli M, Del Gaudio M, Gardini A, Cescon M, Varotti G, Cetta F, Cavallari A (2003) Liver resection for hepatocellular carcinoma on cirrhosis: univariate and multivariate analysis of risk factors for intrahepatic recurrence. Ann Surg 237:536–543
Covey AM, Maluccio MA, Schubert J, BenPorat L, Brody LA, Sofocleous CT, Getrajdman GI, Fong Y, Brown KT (2006) Particle embolization of recurrent hepatocellular carcinoma after hepatectomy. Cancer 106:2181–2189
Ueno M, Uchiyama K, Ozawa S, Nakase T, Togo N, Hayami S, Yamaue H (2009) Prognostic impact of treatment modalities on patients with single nodular recurrence of hepatocellular carcinoma. Surg Today 39:675–681
Matsuda M, Fujii H, Kono H, Matsumoto Y (2001) Surgical treatment of recurrent hepatocellular carcinoma based on the mode of recurrence: repeat hepatic resection or ablation are good choices for patients with recurrent multicentric cancer. J Hepatobiliary Pancreat Surg 8:353–359
Poon RTP, Fan STF, Lo CM, Liu CL, Wong J (2002) Long-term survival and pattern of recurrence after resection of small hepatocellular carcinoma in patients with preserved liver function: implications for a strategy of salvage transplantation. Ann Surg 235:373–382
Ng KK, Lo CM, Liu CL, Poon RTP, Chan SC, Fan ST (2008) Survival analysis of patients with transplantable recurrent hepatocellular carcinoma: implications for salvage liver transplant. Arch Surg 143:68–74
Kobayashi A, Kawasaki S, Miyagawa S, Miwa S, Noike T, Takagi S, IiJima S, Miyagawa Y (2006) Results of 404 hepatic resections including 80 repeat hepatectomies for hepatocellular carcinoma. Hepatogastroenterology 53:736–741
Kubo S, Takemura S, Uenishi T, Yamamoto T, Ohba K, Ogawa M, Hai S, Ichikawa T, Kodai S, Shinkawa H, Tanaka H (2008) Second hepatic resection for recurrent hepatocellular carcinoma in patients with chronic hepatitis C. World J Surg 32:632–638
Nakajima Y, Ko S, Kanamura T, Nagao M, Kanehiro H, Hisanaga M, Aomatsu Y, Ikeda N, Nakano H (2001) Repeat liver resection for hepatocellular carcinoma. J Am Coll Surg 192:339–344
Belli G, Cioffi L, Fantini C, D’Agostino A, Russo GL, Limongelli P, Belli A (2009) Laparoscopic redo surgery for recurrent hepatocellular carcinoma in cirrhotic patients: feasibility, safety, and results. Surg Endosc 23:1807–1811
Kim H, Rhim H, Choi D, Lim HK, Kim YS (2010) Recurrence and treatment pattern in long-term survivors with hepatocellular carcinoma: a comparison between radiofrequency ablation and surgery as a first-line treatment. World J Surg 8:1881–1886
Kainuma O, Asano T, Aoyama H, Shinohara Y (1999) Recurrent hepatocellular carcinoma successfully treated with radiofrequency thermal ablation. J Hepatobiliary Pancreat Surg 6:190–194
Nicoli N, Casaril A, Marchiori L, Mangiante G, Hasheminia AR (2001) Treatment of recurrent hepatocellular carcinoma by radiofrequency thermal ablation. J Hepatobiliary Pancreat Surg 8:417–421
Schindera ST, Nelson RC, DeLong DM, Clary B (2006) Intrahepatic tumor recurrence after partial hepatectomy: value of percutaneous radiofrequency ablation. J Vasc Interv Radiol 17:1631–1637
Taura K, Ikai I, Hatano E, Fujii H, Uyama N, Shimahara Y (2006) Implication of frequent local ablation therapy for intrahepatic recurrence in prolonged survival of patients with hepatocellular carcinoma undergoing hepatic resection: an analysis of 610 patients over 16 years old. Ann Surg 244:265–273
Choi D, Lim HK, Rhim H, Kim YS, Yoo BC, Paik SW, Joh JW, Park CK (2007) Percutaneous radiofrequency ablation for recurrent hepatocellular carcinoma after hepatectomy: long-term results and prognostic factors. Ann Surg Oncol 14:2319–2329
Liang HH, Chen MS, Peng ZW, Zhang YJ, Zhang YQ, Zhang YQ, Li JQ, Lau WY (2008) Percutaneous radiofrequency ablation versus repeat hepatectomy for recurrent hepatocellular carcinoma: a retrospective study. Ann Surg Oncol 15:3484–3493
Rossi S, Ravetta V, Rosa L, Ghittoni G, Torello Vieria F, Garbagnati F, Silini EM, Dionigi P, Calliada F, Quaretti P, Tinelli C (2011) Repeated radiofrequency ablation for management of patients with cirrhosis with small hepatocellular carcinomas: a long-term cohort study. Hepatology 53:136–147
Meloni MF, Goldberg SN, Moser V, Piazza G, Livraghi T (2002) Colonic perforation and abscess following radiofrequency ablation treatment of hepatoma. Eur J Ultrasound 15:73–76
Mulier S, Mulier P, Ni Y, Miao Y, Dupas B, Marchal G, De Wever I, Michel L (2002) Complications of radiofrequency coagulation of liver tumors. Br J Surg 89:1206–1222
Torzilli G, Del Fabbro D, Palmisano A, Marconi M, Makuuchi M, Montorsi M (2007) Salvage hepatic resection after incomplete interstitial therapy for primary and secondary liver tumors. Br J Surg 94:208–213
Disclosures
Roberto Santambrogio, Mara Costa, Matteo Barabino, Massimo Zuin, Emanuela Bertolini, Francesca De Filippi, Savino Bruno, and Enrico Opocher have no conflict of interest or financial ties to disclose.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Santambrogio, R., Costa, M., Barabino, M. et al. Recurrent hepatocellular carcinoma successfully treated with laparoscopic thermal ablation. Surg Endosc 26, 1108–1115 (2012). https://doi.org/10.1007/s00464-011-2007-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00464-011-2007-4