Abstract
Background
Although a second hepatic resection (SHR) for recurrent hepatocellular carcinoma (HCC) is widely accepted, the indications for SHR have not been established. The risk factors for HCC recurrence after SHR were evaluated to investigate the indications for SHR.
Methods
Subjects included 51 patients who underwent a second hepatic resection for recurrence of HCV-related HCC. Sixteen patients received interferon therapy before or after the first operation. Six patients attained a sustained viral response (SVR) that was defined as return of the alanine aminotransferase (ALT) activity to within the reference range and no detectable serum HCV RNA for at least 1 year after interferon therapy. A biochemical response (BR), defined as a normalized ALT activity for at least 1 year after interferon therapy with or without the transient disappearance of serum HCV RNA, was attained in three patients. The other seven patients were defined as the nonresponse (NR) group.
Results
By univariate analysis, NR and lack of interferon therapy, high indocyanine green retention rate at 15 min (ICGR15), high aspartate aminotransferase activity, high ALT activity, large tumor, and multiple tumors were risk factors for HCC recurrence after SHR. By multivariate analysis, NR and lack of interferon therapy, high ICGR15, large tumor, and multiple tumors were independent risk factors.
Conclusions
Patients in whom active hepatitis has been controlled by interferon therapy are the best candidates for SHR. Interferon therapy should be recommended in patients undergoing resection of an HCV-related HCC because SHR can prolong life in SVR and BR patients.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Despite recent advances in diagnostic and treatment methods, the prognosis for hepatocellular carcinoma (HCC) remains unsatisfactory because the rate of recurrence after treatment is high, especially in patients with chronic hepatitis C [1, 2]. Recurrence after resection of HCC includes metastases from the primary carcinoma and newly developed foci of HCCs (multicentric occurrence) [3–5]. Chronic active hepatitis has been a risk factor for recurrence, especially for multicentric carcinogenesis, after resection of hepatitis C virus (HCV)-related HCC [1, 2, 6] and the recurrence rate at 5 years has been reported to be 70-80%. In addition, the recurrence rate after resection of HCV-related HCC is higher in patients with HCV viremia than in those without viremia [1]. Thus, interferon (IFN) treatment decreases the incidence of HCC and hence the recurrence rate after treatment in patients with chronic hepatitis C [7–16].
A second (repeat) hepatic resection (SHR) for recurrent HCC is now widely accepted as effective treatment [17–20]. However, the disease-free survival rate after SHR is low and the indications for SHR have not been established. Identification of risk factors is essential to improve the selection of patients who might benefit from SHR. This study examines the risk factors for HCC recurrence after SHR to develop objective criteria for SHR.
Patients and methods
Patients
Between October 1992 and May 2006, 53 patients underwent SHR for recurrence of HCV-related HCC. These patients had undergone first hepatic resection between April 1990 and March 2005. During that period, primary hepatic resection was performed for HCV-related HCC in 399 patients. Although the indications for SHR were almost the same as those for the first resection, we performed SHR only when the following two conditions were met [17]. First, the patient must have good liver function, comparable to that at the time of the initial resection. Second, the tumor must be localized so that it can be extirpated completely. For the exceptional patient with multiple recurrent tumors in the remnant liver who have not responded to other available treatments but whose liver function is adequate to tolerate SHR, we perform SHR as part of a multimodality treatment plan. In 2 of the 53 patients with multiple recurrent tumors, SHR was performed only for recurrent tumors for which transcatheter arterial embolization was not effective, as part of a multimodality treatment; the recurrent tumors could not be extirpated completely by SHR in the two patients. SHR was performed according to the standard indications in the remaining 51 patients who the subjects of this study (Table 1). The tumor-free survival rates were compared as a function of clinicopathologic variables. The median follow-up from operation until the detection of HCC recurrence or the study endpoint (31 July 2006) was 415 days (range = 62–4480 days). The median follow-up from operation until death or the study endpoint was 1264 days (range = 62–4480).
This study was conducted in accordance with the Helsinki Declaration and the guidelines of the Ethics Committee of our institution. Informed consent was obtained from each patient.
Interferon therapy
In 5 of 51 patients, primary HCC was detected after IFN therapy. In 11 patients, IFN therapy was performed after the first operation. IFNα was administered in 12 patients. IFNβ, IFNα2a, IFNα and IFNβ, and IFNα and rivabirin were administered in one patient each.
The response to IFN therapy was classified on the basis of changes in the HCV RNA levels and serum alanine aminotransferase (ALT) activity during and immediately after IFN administration and for at least 1 year after IFN therapy. Six patients attained a sustained viral response (SVR) that was defined as return of ALT activity to within the reference range and no detectable serum HCV RNA for at least 1 year after IFN therapy. A biochemical response (BR), defined as normalized ALT activity for at least 1 year after IFN therapy with or without transient disappearance of serum HCV RNA, was attained in three patients. The other seven patients were defined as the nonresponse (NR) group because they had no decrease in their ALT activity and had persistent serum HCV RNA. The serum samples were tested for anti-HCV antibody using an enzyme-linked immunoadsorbent assay (Ortho Diagnostic Systems, Tokyo, Japan). Serum HCV RNA was assayed by a reverse transcriptase-nested polymerase chain reaction using primers derived from a conserved 5′-untranslated region of the viral genome [7] and by a branched DNA probe method (Quantiplex HCV-RNA, Chiron Corp., Emeryville, CA).
Detection of recurrence
Serum concentration of α-fetoprotein and protein induced by vitamin K absence and antagonist II were measured 1 month after surgery and every 3 months thereafter. Ultrasonography, computed tomography, chest radiography, or some combination of these tests was done 1 month after surgery and every 3 months thereafter. When a recurrence of HCC was strongly suspected on the basis of tumor markers or imaging, selective hepatic angiography, ultrasound-guided biopsy, or both was conducted to establish a definitive diagnosis.
Histology
The system of the Liver Cancer Study Group of Japan [21] was used to categorize histologic findings. The histologic grade of differentiation (well, moderate, or poor) of HCC was determined according to a modification of Edmondson and Steiner [22]. The grade score (severity of active hepatitis) and stage score (degree of hepatic fibrosis) in noncancerous hepatic tissues were determined by the score of the histologic activity index [23], which was determined by four events, i.e., periportal necrosis with or without bridging necrosis, intralobular degeneration with focal necrosis, portal inflammation, and fibrosis.
Statistics
The survival rates were calculated by the Kaplan-Meier method and were compared with those from the log-rank test. The tumor-free survival time was measured from the date of resection until the detection of a recurrent tumor or the endpoint of this study (31 July 2006) in patients without recurrence. Cox’s proportional hazard model with stepwise variable selection was used for multivariate analysis. A p value of less than 0.05 was considered significant. Variables were selected on the basis of previous studies or our own clinical experience. The variables chosen were age (≥65 or <65), gender, history of alcohol abuse (intake of at least 86 g of ethanol daily for at least 10 years) [24], history and response to IFN therapy (SVR, BR vs. NR, and no treatment), total bilirubin (≥1 or <1 mg/dl), albumin concentration (≥3.5 or <3.5 g/dl), indocyanine green retention rate at 15 min (ICGR15, ≥20 or <20%), platelet count (≥10 × 104 or <10 × 104/μl), aspartate aminotransferase (AST) activity (>40 or ≤40 IU/L), ALT activity (>45 or ≤45 IU/L), serum α-fetoprotein concentration (AFP, >20 or ≤20 ng/ml), the largest diameter of the main tumor (>4 or ≤4 cm), the degree of differentiation of the main tumor (well-, moderate vs. poorly differentiated HCC), the number of tumors (single or multiple, including intrahepatic metastasis), microscopic portal invasion, the grading score (0, 1, or 2-4), the staging score (0-3 or 4), and operative method.
Results
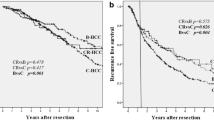
There was no operative mortality. Intractable pleural effusion that called for use of diuretics and treatment by thoracocentesis developed postoperatively in three patients, intra-abdominal infection in two patients, bile leakage in two patients, and gastric ulcer in two patients. The tumor-free and cumulative survival rates after SHR in the 51 patients are shown in Figure 1.
By univariate analysis, NR and lack of interferon therapy (p = 0.0089), high ICGR15 (p = 0.0068), high AST (p = 0.0607), high ALT (p = 0.0930), large tumor (>4 cm, p < 0.0001), and multiple tumors (p = 0.0105) were risk factors for HCC recurrence after SHR (Table 2). Multivariate analysis showed that NR and lack of IFN therapy, high ICGR15, large tumor, and multiple tumors were independent risk factors for HCC recurrence after SHR (Table 3). The tumor-free survival rate was higher in SVR and BR patients than in other patients, including NR patients and patients who did not undergo IFN therapy (p = 0.0089, Fig. 2). The tumor-free survival rate was higher in patients with small tumor (≤4 cm) than in patients with large tumor (>4 cm, p < 0.0001, Fig. 3). The clinicopathologic findings in patients who were sustained viral responders or biochemical responders and in other patients are shown in Table 4. The mean age and gender distribution were similar in the different groups. Although serum concentrations of total bilirubin, albumin, and ICGR15 were not significantly different between the groups, platelet count was significantly higher in patients who were sustained viral responders or biochemical responders than in other patients. The serum activities of AST and ALT were significantly lower in patients who were sustained viral responders or biochemical responders than in other patients. Thus, active hepatitis was controlled in SVR and BR patients. The proportion of patients with an elevated serum AFP concentration (>20 ng/ml), tumor size, differentiation of the main tumor, prevalences of portal invasion and multiple tumors, grading score, staging score, and operative methods were similar in the different groups.
Discussion
Treatment for recurrent HCCs includes SHR, ablation therapy such as microwave coagulation therapy and radiofrequency ablation therapy, and transarterial therapy such as transcatheter arterial embolization. Liver transplantation is another option in selected patients with impaired liver function. Although the value of SHR for recurrence has been demonstrated, indications for SHR are unclear. The tumor-free survival rate in patients with chronic hepatitis is unsatisfactory because multicentric carcinogenesis persists as long as hepatitis remains active. Recurrence is not uncommon following SHR, even when the resection is considered curative.
Although prognostic factors after first resection for HCC have been evaluated by many investigators, there are a few studies about prognostic factors after SHR. In addition, viral status in patients has not been evaluated in the previous study. In this study univariate analysis showed that NR and lack of IFN therapy, high ICGR15, high AST, high ALT, large tumor, and multiple tumors are risk factors for recurrence. In addition, the tumor-free survival rate was higher in SVR and BR patients than in other patients, nonresponders, and patients who did not undergo IFN therapy. Multivariate analysis showed NR and lack of IFN therapy, high ICGR15, large tumor, and multiple tumors are independent risk factors for HCC recurrence after SHR. Previous studies have indicated that active hepatitis with a sustained increase in the serum aminotransferase activity is a risk factor for recurrence [1, 2, 6, 25]. Other recent studies found that HCC is less likely to develop in patients in whom IFN normalized serum ALT activity, even when HCV RNA remained detectable [11, 12]. IFN therapy also suppresses carcinogenesis after surgery [13, 14, 16, 26, 27]. In this study, active hepatitis had been suppressed in SVR and BR patients, and the tumor-free survival rate after SHR was significantly higher in these patients than in others. Thus, the induction of remission of active hepatitis by IFN therapy suppressed carcinogenesis after SHR. The study of IFN therapy after tumor ablation by Shiratori et al. [16] showed that the rate of second or third recurrence was lower in the IFN group than in the control group, although the incidence of first recurrence of a new foci of HCC was similar in the two groups. It is possible that what is called the first recurrent tumor had already developed by the time of the first operation, and the remission of active hepatitis by IFN therapy suppressed subsequent carcinogenesis. Thus, SHR is likely to be associated with a low incidence of recurrence when IFN therapy has controlled chronic hepatitis C. IFNα was the first therapy for chronic hepatitis C. The combination of IFN and ribavirin increases SVR rates compared with IFN alone. The combination of a pegylated IFN and ribavirin significantly increases SVR rates and is now recognized as the standard therapy [28]. Such IFN therapy is recommended in patients with chronic hepatitis C, even after resection of primary HCC.
The independent risk factors for recurrence after SHR include large tumors and multiple tumors. Thus, a close follow-up after the first operation is important for detecting HCC recurrence at an early stage. When a small recurrent tumor is detected, liver resection or ablation therapy is indicated. We reported that anatomic resection is a favorable prognostic factor in patients in whom IFN was effective [29]. Thus, anatomic resection may be more useful than ablation therapy in such patients. On the other hand, SHR or transarterial therapy is usually used in patients with advanced recurrent tumors such as large tumors and multiple tumors because intrahepatic recurrence was strongly suspected to represent metastasis, in which case IFN therapy is unlikely to be effective. Such lesions require additional treatment such as anticancer chemotherapy.
In conclusion, patients in whom active hepatitis has been controlled by IFN therapy are the best candidates for SHR. IFN therapy should be recommended in patients undergoing resection of an HCV-related HCC because SHR prolongs life if there is a recurrence after liver resection.
References
Kubo S, Nishiguchi S, Shuto T et al. (1999) Effects of continuous hepatitis with persistent hepatitis C viremia on outcome after resection of hepatocellular carcinoma. Jpn J Cancer Res 90:162–170
Kubo S, Hirohashi K, Tanaka H et al. (2000) Risk factors for recurrence after resection of hepatitis C virus-related hepatocellular carcinoma. World J Surg 24:1559–1565
Kumada T, Nakano S. Takeda I et al. (1997) Patterns of recurrence after initial treatment in patients with small hepatocellular carcinoma. Hepatology 25:87–92
Kubo S, Kinoshita H, Hirohashi K et al. (1999) Patterns of and risk factors for recurrence after liver resection for well-differentiated hepatocellular carcinoma: a special reference to multicentric carcinogenesis after operation. Hepatogastroenterology 46:3212–3215
Sakon M, Umeshita K, Nagano H et al. (2000) Clinical significance of hepatic resection in hepatocellular carcinoma: analysis by disease-free survival curves. Arch Surg 135:1456–1459
Tarao K, Takemiya S, Tamai S et al. (1997) Relationship between the recurrence of hepatocellular carcinoma (HCC) and serum alanine aminotransferase levels in hepatectomized patients with hepatitis C virus-associated cirrhosis and HCC. Cancer 79:688–694
Nishiguchi S, Kuroki T, Nakatani S et al. (1995) Randomised trial of effects of interferon-alpha on incidence of hepatocellular carcinoma in chronic active hepatitis C with cirrhosis. Lancet 346:1051–1055
Kasahara A, Hayashi N, Mochizuki K et al. (1998) Risk factors for hepatocellular carcinoma and its incidence after interferon treatment in patients with chronic hepatitis C. Hepatology 27:1394–1402
Imai Y, Kawata S, Tamura S et al. (1998) Relation of interferon therapy and hepatocellular carcinoma in patients with chronic hepatitis C. Osaka Hepatocellular Carcinoma Prevention Study Group. Ann Intern Med 129:94–99
International Interferon-alpha Hepatocellular Carcinoma Study Group (1998) Effect of interferon-alpha on progression of cirrhosis to hepatocellular carcinoma: a retrospective cohort study. Lancet 351:1535–1539
Yoshida H, Shiratori Y, Moriyama M et al. (1999) Interferon therapy reduces the risk for hepatocellular carcinoma: national surveillance program of cirrhotic and noncirrhotic patients with chronic hepatitis C in Japan. IHIT Study Group. Inhibition of Hepatocarcinogenesis by Interferon Therapy. Ann Intern Med 131:174–181
Ikeda K, Saitoh S, Arase Y et al. (1999) Effect of interferon therapy on hepatocellular carcinogenesis in patients with chronic hepatitis type C: a long-term observation study of 1,643 patients using statistical bias correction with proportional hazard analysis. Hepatology 29:1124–1130
Ikeda K, Arase Y, Saitoh S et al. (2000) Interferon beta prevents recurrence of hepatocellular carcinoma after complete resection or ablation of the primary tumor—a prospective randomized study of hepatitis C virus-related liver cancer. Hepatology 32:228–232
Kubo S, Nishiguchi S, Hirohashi K et al. (2001) Effects of long-term postoperative interferon-α therapy on intrahepatic recurrence after resection of hepatitis C virus-related hepatocellular carcinoma: a randomized, controlled trial. Ann Intern Med 34:963–967
Kubo S, Nishiguchi S, Hirohashi K et al. (2002) Randomized clinical trial of long-term outcome after resection of hepatitis C virus-related hepatocellular carcinoma by postoperative interferon therapy. Br J Surg 89:418–422
Shiratori Y, Shiina S, Teratani T et al. (2003) Interferon therapy after tumor ablation improves prognosis in patients with hepatocellular carcinoma associated with hepatitis C virus. Ann Intern Med 138:299–306
Shuto T, Kinoshita H, Hirohashi K et al. (1996) Indications for, and effectiveness of, a second hepatic resection for recurrent hepatocellular carcinoma. Hepatogastroenterology 43:932–937
Shimada M, Takenaka K, Taguchi K et al. (1998) Prognostic factors after repeat hepatectomy for recurrent hepatocellular carcinoma. Ann Surg 227:80–85
Nakajima Y, Ko S, Kanamura T et al. (2001) Repeat liver resection for hepatocellular carcinoma. J Am Coll Surg 192:339–344
Minagawa M, Makuuchi M, Takayama T et al. (2003) Selection criteria for repeat hepatectomy in patients with recurrent hepatocellular carcinoma. Ann Surg 238:703–710
Liver Cancer Study Group of Japan (2003) General rules for the clinical and pathological study of primary liver cancer, 2nd ed. Kanehara & Co, Tokyo
Edmondson HA, Steiner PE (1954) Primary carcinoma of the liver: a study of 100 cases among 48,900 necropsies. Cancer 7:462–503
Desmet VJ, Gerber M, Hoofnagle JH et al. (1994) Classification of chronic hepatitis: diagnosis, grading and staging. Hepatology 19:1513–1520
Liver Cancer Study Group of Japan (1990) Primary liver cancer in Japan: Clinicopathological features and results of surgical treatment. Ann Surg 211:277–287
Shirabe K, Takenaka K, Taketomi A et al. (1996) Postoperative hepatitis status as a significant risk factor for recurrence in cirrhotic patients with small hepatocellular carcinoma. Cancer 77:1050–1055
Kubo S, Nishiguchi S, Hirohashi K et al. (2001) Influence of previous interferon therapy on recurrence after resection of hepatitis C virus-related hepatocellular carcinoma. Jpn J Cancer Res 92:59–66
Uenishi T, Kubo S, Hirohashi K et al. (2002) Relationship between response to previous interferon therapy and postoperative recurrence of hepatitis C virus-related hepatocellular carcinoma. Hepatol Res 24:404–412
Moreno-Otero R (2005) Therapeutic modalities in hepatitis C: challenges and development. J Virol Hepat 12:10–19
Kubo S, Tanaka H, Takemura S et al. (2007) Surgical treatment for hepatocellular carcinoma detected after successful interferon therapy. Surg Today 37:285–290
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Kubo, S., Takemura, S., Uenishi, T. et al. Second Hepatic Resection for Recurrent Hepatocellular Carcinoma in Patients with Chronic Hepatitis C. World J Surg 32, 632–638 (2008). https://doi.org/10.1007/s00268-007-9365-z
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00268-007-9365-z