Abstract
Background
The main source of postoperative pain after laparoscopic repair of ventral hernia is thought to be fixation of implanted mesh. This study aimed to analyze whether a relation exists between the number of tacks used for fixation and postoperative pain.
Methods
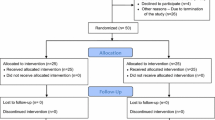
To reduce the number of prognostic variables, only patients with primary umbilical hernia who underwent laparoscopic repair with double-crown mesh fixation were enrolled in this study. Two groups differing only in the manner of tacking were compared. Group 1 (n = 40), collected from previous studies, showed no specific efforts to minimize the number of tacks. Group 2 was a cohort of 40 new patients who underwent double-crown fixation using the minimal number of tacks considered to provide adequate mesh fixation. To eliminate systematic and random errors, the study analyzed only for postoperative pain. The severity of the patients’ pain was assessed preoperatively and then 2, 6, and 12 weeks postoperatively using a visual analog scale (VAS) ranging from 0 to 100.
Results
The mean number of tacks used differed significantly between the two groups: group 1 (45.4 ± 9.6) vs group 2 (20.4 ± 1.4) (p = 0.001). Postoperative pain differed significantly only at the 3-month postoperative assessment: group 1 VAS (5.78) vs group 2 VAS (1.80) (p = 0.002).
Conclusions
Although postoperative pain differed significantly at the 3-month follow-up assessment, both VAS scores were so low that from a clinical point of view, this difference seems irrelevant. Fewer tacks do not create less pain, nor do more tacks create more pain. This absence of a correlation between the number of tacks used and postoperative pain may indicate that pain after laparoscopic repair of at least small ventral hernias possibly is generated according to some “threshold” principle rather than according to a cumulative effect created by more points of fixation.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Patients who undergo laparoscopic repair of ventral or incisional hernia (LRVIH) tend to have more pain postoperatively than those treated with any other minimally invasive procedure [1–3]. The main source of this pain is thought to be fixation of the implanted mesh. Mesh fixation in LRVIH involves the use of tacks, transabdominal sutures (TAS), or both. Although postoperative pain after LRVIH was traditionally linked to TAS [4, 5], a few recent studies have indicated that TAS is not the only cause of pain, pointing out the important role of tacks [6–8].
Currently, the most popular method of mesh fixation entails inserting two circles of tacks only and no TAS at all (the double-crown [DC] technique) [9]. The relation between the number of tacks used in LRVIH and postoperative pain has never been specifically analyzed, and this study aimed to address that issue.
Methods
Only healthy patients with primary umbilical hernias (PUHs) no larger than 2 cm who underwent a straightforward laparoscopic repair were enrolled in this study and subsequently divided into two groups. All repairs were performed by one of two surgeons well experienced with this technique using a completely standardized technique with the same materials.
The two groups differed only in the manner of tacking. The first group was historical and extracted from our previous studies [6, 10, 11]. This group consisted of 40 healthy PUH patients who underwent a “free-tacking” DC fixation without specific efforts to minimize the number of tacks used or to define a set minimum of tacks beforehand. For this group, a mesh size of 15 × 10 cm was routinely used.
The second group was a prospective cohort of 40 consecutive new patients who underwent DC fixation using the minimal number of tacks considered to provide an adequate fixation of the mesh. In this group, a mesh of 12 × 10 cm was routinely used. Assuming that intervals of 15 to 20 mm between tacks were sufficient, we considered 16 tacks adequate for the outer ring and 4 tacks sufficient for the inner ring. Hence, the desired number of tacks to be used was 20, with an option to add a few more tacks when considered needed. To ensure correct execution of the procedure, desired places for insertion of tacks were marked on the mesh before its insertion into the abdomen.
Operative technique
Pneumoperitoneum was established by use of the Veress needle. Three trocars (one 10 mm and two 5 mm trocars) were inserted left laterally. When present, hernial content, usually the omentum, was reduced and the surrounding area prepared for mesh placement. This frequently required release of the round ligament. A 1-mm-thick expanded polytetrafluoroethylene mesh (DualMesh; WL Gore & Associates, Flagstaff, AZ, USA) was used to overlap the hernia opening by at least 3 cm. No attempt was made to reapproximate the edges of the hernia opening.
The mesh was fixed using a DC of tacks (ProTack; TycoUSS, Norwalk, CT, USA) only. With this technique, the outer ring of tacks is placed along the periphery of the mesh, and the inner ring of tacks is placed around the hernia opening. All patients received identical postoperative analgesia and care.
Clinical follow-up evaluation
All patients were scheduled to return for an outpatient visit 2 weeks, 6 weeks, and 3 months after surgery. The severity of postoperative pain was determined by scores on a visual analog scale (VAS; range, 0–100) obtained preoperatively (baseline) and during the outpatient visits.
Statistical analysis
Data were collected in an Excel database, and statistical analyses were performed using the Statistical Package for Social Sciences (SPSS) for Windows version 15.0 (SPSS Inc., Chicago, IL, USA). Categorical variables were compared using the chi-square test, and continuous variables were compared using the independent-samples t test. A p value less than 0.05 was considered statistically significant.
Results
All requested data were available for all the patients. Both groups had similar patient demographic and hernia characteristics (Table 1). Of the postoperative characteristics, only the number of tacks used differed significantly between the two groups (p = 0.001). The mean number of tacks was 45.4 ± 9.6 in the group 1 and 20.4 ± 1.4 in group 2.
The primary outcome measure of this study, postoperative pain, did not differ significantly at 2 or 6 weeks postoperatively (Table 2). A significant difference (p = 0.002) between the two groups was observed only at the 3-month follow-up assessment. No recurrences or complications requiring surgical or invasive radiologic treatment occurred during the study period.
Discussion
Postoperative pain after LRVIH seems to be a relevant complaint during the early postoperative period, leading to increased consumption of pain medication, delayed bowel function, and extended hospital stay [12]. As is the case with mesh repair of inguinal hernias, an increasing number of clinicians now consider postoperative pain rather than recurrence the most important adverse effect of LRVIH. Consequently, current interest focuses increasingly on the genesis of pain after LRVIH and methods to reduce such pain.
The relation between postoperative pain after LRVIH and the number of tacks used has not been explicitly analyzed previously. Our previous prospective randomized trial, a study with a significant number of prognostic variables that did not specifically address the same problem considered in this study, could not demonstrate any correlation [6].
Some results of the previous study indicate that “free tacking” may frequently result in “overtacking.” When a 15 × 10-cm mesh with tacks placed 5 mm inside the outer rim of the mesh is used, the total perimeter of tacking is approximately 38 cm. If spacing of 15 to 20 mm between tacks is desired, 20 to 25 tacks should be sufficient for the outer circle, and about 4 to 6 tacks should suffice for the inner circle. Consequently, the total number of tacks used for a DC fixation of mesh should not exceed 30 tacks. However, we used more than 50% more tacks in our historic “free-tacking” group. For each of these operations, we unequivocally opened two tacking devices.
These results confirmed our impression that we had been prone to continue firing the tacking device until it was empty and, in general, to insert more tacks than necessary. We assume that this behavior is not an exception among surgeons performing LRVIH.
Applying a similar calculation to a 12 × 10-cm mesh, which is equally sufficient for repair of a PUH as a 15 × 10-cm mesh, a total of 20 tacks should be sufficient. This “controlled” tacking in group 2 resulted in insertion of 55% fewer tacks and unequivocally required not more than a single tacking device per operation.
Whereas the financial effects of “controlled” tacking are obvious, its effect on postoperative pain is less clear. The data obtained in this study did not demonstrate any significant difference in pain 2 and 6 weeks postoperatively. At 3 months, postoperative pain was significantly higher in group 1 (VAS score, 5.78 vs. 1.80). However, a VAS score of 5.78 is so low that from a clinical point of view, this difference seems irrelevant. The consensus of Dutch anesthesiologists suggests moderate pain (VAS > 40) as an indication for analgesics [13]. This cutoff point is obviously much higher than the highest postoperative VAS score measured in our study. However, consistently higher VAS scores in the “free-tacking” group may carry a potential to influence quality of life, resumption of activities, and the like. With our data, unfortunately we could not address this issue.
Theoretically, the potential negative consequence of decreasing the number of tacks could be internal herniation in the gaps between the tacks in the outer ring of the double crown. In our experience with more than 800 LRVIH procedures, this problem did not occur when tacks were placed at 15- to 20-mm intervals.
In their recently published study, Sharma et al. [14] describe application of tacks at 3-cm intervals, with no recurrences caused by internal herniation between tacks. Consequently, it seems safe to apply tacks at intervals of 15 to 20 mm.
Another possible consequence of fewer tacks could be an increased recurrence rate. Follow-up evaluation will continue, but we have no indication of that consequence to date.
The potential deficiency of this study is that it was not randomized, and the data for the first group were extracted from a previous study [6]. The data in that study were however collected prospectively, as in group 2 of the current study, with pain as one of the main outcome measures. The traditional disadvantages of retrospective data collection therefore do not seem applicable for this study.
The main reason for not proceeding with a prospective randomized study was ethical. Unnecessary “overtacking” carried a potential to induce more unnecessary postoperative pain, and we were already in possession of a historical group. In addition, it would needlessly increase operation costs.
The organization of this study also provided some advantages. To minimize the number of prognostic variables and to provide more accurate data on the relation between postoperative pain and the number of tacks used, we used a maximally homogeneous model of the procedure including the same site, a similar size of hernia, one type of prosthetic mesh and fixation device, a standardized technique, and identical postoperative care. This protocol made performance bias unlikely. However, the main disadvantage of such a protocol is that the results of this study are applicable only for a small PUH. For larger hernias, whose repair requires the use of more tacks, there remains the possibility of a threshold above which the number of tacks does make a difference in postoperative pain.
To minimize systematic and random errors, we analyzed only one outcome: postoperative pain. Postoperative pain is however a complex issue influenced by multiple factors. If different subgroup analyses had been made, the results may have been different.
A bit disappointing, the results of this study indicate that fewer tacks do not necessarily create less pain for the patient; nor do more tacks create more pain. This absence of a correlation between the number of tacks used and postoperative pain did not lend support to hypothesis that pain after LRVIH is generated by a cumulative effect resulting from more points of fixation [6]. This may indicate the possibility that pain is generated according to some “threshold” principle. The search for less painful methods of mesh fixation in LRVIH continues.
References
Costanza MJ, Heniford BT, Arca MJ, Mayes JT, Gagner M (1998) Laparoscopic repair of recurrent ventral hernias. Am Surg 64:1121–1127
Samuel K, Miller SK, Carey SD, Rodriguez FJ, Smoot RT Jr (2003) Complications and their management. In: LeBlanc KA (ed) Laparoscopic hernia surgery: an operative guide. Arnold, London, pp 161–169
Eriksen JR, Poornoroozy P, Jørgensen LN, Jacobsen B, Friis-Andersen HU, Rosenberg J (2009) Pain, quality of life, and recovery after laparoscopic ventral hernia repair. Hernia 13:13–21
Carbonell AM, Harold KL, Mahmutovic AJ, Hassan R, Matthews BD, Kercher KW, Sing RF, Heniford BT (2003) Local injection for the treatment of suture-site pain after laparoscopic ventral hernia repair. Am Surg 69:688–692
LeBlanc KA (2004) Laparoscopic incisional and ventral hernia repair: complications—how to avoid and handle. Hernia 8:323–331
Wassenaar E, Schoenmaeckers E, Raymakers J, van der Palen J, Rakic S (2010) Mesh-fixation method and pain and quality of life after laparoscopic ventral or incisional hernia repair: a randomized trial of three fixation techniques. Surg Endosc 24:1296–1302
Beldi G, Wagner M, Bruegger LE, Kurmann A, Candinas D (2011) Mesh shrinkage and pain in laparoscopic ventral hernia repair: a randomized clinical trial comparing suture versus tack mesh fixation. Surg Endosc 25(3):749–755
Nguyen SQ, Divino CM, Buch KE, Schnur J, Weber KJ, Katz LB, Reiner MA, Aldoroty RA, Herron DM (2008) Postoperative pain after laparoscopic ventral hernia repair: a prospective comparison of sutures versus tacks. JSLS 12:113–116
Morales-Conde S, Cadet H, Cano H, Bustos M, Martín J, Morales-Mendez S (2005) Laparoscopic ventral hernia repair without sutures—double-crown technique: our experience after 140 cases with a mean follow-up of 40 months. Int Surg 90(3 Suppl):S56–S62
Wassenaar EB, Schoenmaeckers EJ, Raymakers JT, Rakic S (2009) Recurrences after laparoscopic repair of ventral and incisional hernia: lessons learned from 505 repairs. Surg Endosc 23:825–832
Wassenaar EB, Raymakers JT, Rakic S (2008) Impact of the mesh fixation technique on operation time in laparoscopic repair of ventral hernias. Hernia 12:23–25
Bellows Ch, Berger D (2006) Infiltration of suture sites with local anesthesia for management of pain following laparoscopic ventral hernia repairs: a prospective randomized trial. JSLS 10:345–350
The Netherlands Society of Anesthesiologists. Guidelines postoperative pain 2003. ISBN 90-76906-66-1
Sharma A, Mehrota M, Khullar R, Soni V, Baijal M, Chowbey PK (2011) Laparoscopic ventral/incisional hernia repair: a single-centre experience of 1,242 patients over a period of 13 years. Hernia 15:131–139
Disclosures
Ernst J. P. Schoenmaeckers, Robert J. de Haas, Vincent Stirler, Johan T. F. J. Raymakers, and Srdjan Rakic have no conflicts of interest or financial ties to disclose.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Schoenmaeckers, E.J.P., de Haas, R.J., Stirler, V. et al. Impact of the number of tacks on postoperative pain in laparoscopic repair of ventral hernias: do more tacks cause more pain?. Surg Endosc 26, 357–360 (2012). https://doi.org/10.1007/s00464-011-1876-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00464-011-1876-x