Abstract
Background
Glue mesh fixation is thought to cause less pain compared to tack mesh fixation during laparoscopic total extraperitoneal inguinal hernia repair (TEP). However, the clinical benefits of glue mesh fixation are still controversial. This study aimed to evaluate the acute pain, chronic pain, and recurrence rate between these two fixation methods.
Methods
After reviewing all patients in our prospective hernia repair database from February 2008 to December 2017, we identified 583 patients who underwent TEP with tack mesh fixation and 70 patients with glue fixation by a single surgeon. Acute post-operative pain and activity level were evaluated using a Visual Analog Score (VAS) and the modified Medical Outcome Study (MOS) score. The primary endpoint was chronic pain 6 months after TEP. The secondary endpoints were acute pain, activity level, complications, and recurrence.
Results
After adjustment for potential confounding factors, the glue mesh fixation had significant lower VAS at 2 h post operation during rest and coughing and on the first day after surgery during coughing (p = 0.005, p < 0.001, and p = 0.011). The modified MOS on the first day was higher in the glue group (p < 0.001). There were no reduced risk of chronic pain or increased risk of recurrence for the glue group compared to the tack group [Odds ratio (OR) = 0.237, p = 0.169; OR = 2.498, p = 0.299]. In the sub-group analysis for recurrent hernia repair, glue fixation is associated with better modified MOS (p = 0.031) on first day and lower VAS on the operative day and first day at rest (p = 0.003 and p = 0.024) after surgery.
Conclusions
Glue fixation method was superior to tack fixation method in acute post-operative pain and early post-operative activity level after laparoscopic TEP repair. However, both fixation methods had similar incidence of chronic pain-, recurrence-, and procedure-related complications after laparoscopic TEP repair.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Inguinal hernia repair is one of the most common surgical procedures in the world. In comparison with the widely adopted conventional Litchtenstein repair, laparoscopic inguinal hernia repair has the advantages of less acute post-operative pain, quicker recovery, earlier return to normal daily activities, less chronic pain, and better cosmetic appearances [1]. Although the incidence of chronic pain was reduced in patients treated by laparoscopic approach [2], severe long-lasting pain had been reported in up to 6% [3].
The chronic pain is thought to result from nerve damage or chronic inflammation over tack fixation points in laparoscopic hernia repair [4]. To avoid this mechanical injury, non-penetrating mesh fixation with adhesive materials has been advocated [5]. The glue mesh fixation may reduce acute and chronic pain, but it may also increase the risk of mesh migration and hernia recurrence. A recent meta-analysis of randomized trials in laparoscopic inguinal hernia repair concluded that the glue mesh fixation had a lower incidence of chronic pain and did not increase morbidity or recurrence compared to tack fixation [6]. However, a Swedish nationwide register-based study showed no statistical difference in chronic pain and recurrence between tack or glue fixation for laparoscopic total extraperitoneal inguinal hernia repair (TEP) [7]. Therefore, the benefits of glue fixation are still undecided.
In this study, we retrospectively reviewed prospective data from patients with laparoscopic TEP repair using either tack or glue mesh fixation. The study aimed to evaluate the acute pain, the incidence of chronic pain, morbidity, and recurrence rate between these two fixation methods.
Materials and methods
Patients
This is a retrospective study using a prospective laparoscopic hernia repair database of our institution. Between February 2008 and December 2017, 840 patients underwent laparoscopic TEP hernia repair by a single surgeon who had experience in laparoscopic TEP since 2003 with more than 200 laparoscopic TEP surgeries before collecting this prospective database. According to our previous published data between 2011 and 2016 [8,9,10,11,12], the main historical outcomes of laparoscopic TEP repair are as follows: average operative time is around 50–60 min, 1–2% hernia recurrence rate, 7–8% post-operative seroma, and 4–5% chronic pain. Although this study enrolled cases over 9 years, both fixation techniques were continuously used throughout these 9 years. Therefore, any change or evolving of the surgical techniques was evenly distributed in both groups, and the risk of technical evolving induced study bias is low. The choice of tack or glue fixation was according to patient’s preference.
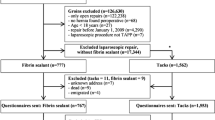
The primary endpoint was chronic pain 6 months after TEP. The secondary endpoints included acute pain, complications, and recurrence. The inclusion criteria in this study were primary or recurrent symptomatic inguinal hernia requiring surgical intervention. Our prospective laparoscopic hernia repair database did not include previous major lower abdominal surgery, concomitant surgical procedures, and emergent surgery. Patients who had an unregistered fixation method or lost follow-up before 6 months after their operation were excluded. Finally, we identified 583 patients who underwent TEP with tack mesh fixation and 70 patients with glue fixation. The flow diagram for the patient selection is shown in Fig. 1. The data analysis were approved by the ethics committee of our institution (IRB code: 08-X-040).
Operative technique
All patients underwent general anesthesia and received a single dose of prophylactic antibiotics before surgery. Foley catheter drainage was only reserved for patients with a history of low abdominal or low urinary tract surgery. A sub-umbilical incision was made for the 12-mm camera port, and the pre-peritoneal space was created by a balloon dissector. Then, the other two 5-mm working ports were placed vertically in the midline. After the hernia sac dissection and ligation, a polypropylene monofilament mesh or a Surgisis mesh (Cook Surgicl, Bloomington, IN) not smaller than 10 × 15 cm was placed to cover the whole myopectineal orifices. Most of the heavyweight meshes and lightweight meshes we used were Bard Mesh (Bard/Davol Inc.) and Optilene Mesh (B Braun), respectively.
In the tack group, the mesh was attached to the Cooper’s ligament and the anterior-lateral abdominal wall lateral to the iliopubic tract by laparoscopic tackers (Protack; Covidien, Norwalk, CT, USA). In the glue group, n-butyl-2-cyanoacrylate glue (Histoacryl; B. Braum, AG, Melsungen, Germany) was applied through a 5 Fr. catheter to fix the mesh on the same area as in the tack group. The costs of tackers and glue for each case were 600 USD and 100 USD, respectively.
Post-operative care and follow-up assessment
After surgery, all patients were treated with standardized post-operative care, including early oral intake, early ambulation, and use of on-demand pain killers. Post-operative pain during rest and coughing was evaluated using a Visual Analog Score (VAS) on a 0–10 scale for pain at 2 h, 1 day, and 1 week after operation by an independent clinic nurse.
All patients were also assessed in the outpatient clinic at 1 week, 3 months, and 6 months for post-operative pain, complications, and activity level. The post-operative activity level was measured using the modified Medical Outcome Study (MOS; item 3–12/36 items) score at 1 day, 1 week, and 3 months. Chronic pain was assessed during an interview with the surgeon at the outpatient clinic or via phone six months after the operation. Then, patients were followed up annually at the outpatient clinic.
Statistical analysis
Differences between groups were compared using Pearson Chi square for categorical variables and two-sample t test or Mann–Whitney U test for continuous variables. Continuous variables were tested for normality using Kolmogorov–Smirnov test. The potential confounding variables identified in our preliminary analysis, such as sex, age, body mass index, mesh material, and intra-operative complications were adjusted with multivariable linear and logistic regression models. All statistical assessments were two-tailed and considered statistically significant as p < 0.05. Statistical analyses were carried out with IBM SPSS statistical software version 22.
Results
Baseline characteristics
The baseline characteristics of the 583 patients in the tack group and 70 patients in the glue group are shown in Table 1. The mean ages were 54.3 ± 15.5 years and 58.8 ± 12.7 years in the tack and glue groups, respectively (p = 0.015). The mean body mass index (BMI) of the tack group was higher than that of the glue group (23.9 ± 3.0 and 22.7 ± 3.1, p = 0.001). Patients in the glue group also had higher proportion of diabetes mellitus than patients in the tack group (15.7% and 5.7%, p = 0.002). There were no significant differences between groups for sex, risk factors, other comorbidities, clinical symptoms, and previous recurrent hernia history.
Post-operative outcomes
The peri-operative parameters and outcomes are shown in Table 2. There were more lightweight mesh repairs in the glue group than in the tack (80% and 34.8%, p < 0.003). The median operative time was longer in the glue group. (70 min and 60 min, p = 0.001). The intra-operative peritoneal tear and post-operative urinary retention were both more common in the glue group (p < 0.001 and p < 0.017). There were no significant differences between groups for hernia type, hospital stay, the days to return normal daily activity, and post-operative complications such as seroma, wound infection, and urinary tract infection. The recurrence rates were also comparable in the tack and glue groups (3.1% and 2.9%, p = 0.916). However, the median follow-up time for recurrence was shorter in the glue group (6 months and 10 months, p < 0.001).
Acute post-operative pain and Convalescence
In unadjusted analysis, the mean pain score at 2 h and 1 day post-operatively during rest and coughing were significant higher in the tack group (Table 3). Meanwhile, there was no significant difference in the mean morphine equivalent dose between groups. The mean MOS scores at 1 day and 1 week were lower in the tack group. After adjustment analysis with all potential confounding factors such as sex, age, BMI, mesh material, and intra-operative complications, the fixation method still had significant impact on the VAS at 2 h during rest and coughing and on the first day during coughing [VAS-rest-2 h, 95% Confidence interval(CI) (− 1.758, − 0.317), p = 0.005; VAS-cough-2 h, 95% CI (− 2.199, − 0.702), p < 0.001; VAS -cough-1 day, 95% CI (− 2.199, − 0.702), p = 0.011] (Table 4). The MOS score on the first day also revealed significant differences between groups after adjustment analysis. [MOS, 95% CI (1.701, 4.396), p < 0.001].
Chronic pain and hernia recurrence
In unadjusted analysis, the tack group had more chronic pain than the glue group (8.7% versus 1.4%, p = 0.033). However, after adjustment analysis with all potential confounding factors, such as sex, age, body mass index, mesh material, and intra-operative complications, there was no reduced risk of chronic pain for the glue group compared to the tack group [Odds ratio (OR) = 0.237, 95% CI (0.031, 1.845), p = 0.169] (Table 5). Although the median follow-up is relatively short (median 10 and 6 months in each group), the risk of hernia recurrence did not increase in the glue group when compared to the tack group [OR = 2.498, 95% CI (0.444, 14.040), p = 0.299].
Repair for recurrent hernia
In our sub-group analysis comparing the outcomes of the tack and glue fixation in recurrent hernia repair, glue fixation is associated with better modified MOS (23.7 vs. 20.6; p = 0.031) on the first day and lower VAS at 2 h and on the first day rest (5.21 vs. 2.87; p = 0.003 and 3.83 vs. 2.25; p = 0.024) after surgery (Table 6). However, there was no significant difference in the incidences of post-operative complication, chronic pain, and hernia recurrence between groups.
Discussion
Although laparoscopic inguinal hernia repair has greatly improved the quality of life after inguinal hernia repair, acute and chronic post-operative pain leading to short-term and long-term disabilities are still common following even the laparoscopic approach [13]. Both acute or chronic post-operative pain after laparoscopic repair could be associated with mechanical mesh fixation, and this is the main reason that the non-mechanical mesh fixation (glue or non-fixation method) has been developed [14]. Therefore, a comprehensive evaluation of the short- and long-term effects of both mechanical and non-mechanical mesh fixation, which remain scarce in the literature, is mandatory. Our study was more valuable than other similar studies for its relative larger sample size, including bilateral and recurrent hernia repairs and a comprehensive short- and long-term effect evaluation, including acute pain, activity level, morbidity, chronic pain, and recurrence. In the current study, the non-mechanical fixation method (the glue group) was superior to the mechanical fixation method (the tack group) in acute post-operative pain and early post-operative activity level (modified MOS) after laparoscopic inguinal hernia repair. However, both fixation methods had similar incidence of chronic pain-, recurrence-, and procedure-related morbidity after laparoscopic TEP repair.
There are four randomized control trials (RCT) comparing tack and glue fixation during laparoscopic TEP in the literature thus far. [15,16,17,18] In these early RCTs, acute post-operative pain was either no different between groups or lower in the glue group. However, these acute pain differences were less significant within the 1st post-operative day, which was contrary to the current study and our past RCT experiences. According to our previous experience in randomized control trials, the acute pain was always most severe immediately after the procedure, then the pain progressively resolved with time [10]. Therefore, either the sample size should be large enough or the pain scale differences should be big enough to result in statistical differences in a RCT. For a small-scale RCT in the literature to gain a significant difference in post-operative acute pain, the statistical difference is always presented in the first few hours or on the first few days. Thus, these early RCT revealed confusing results in acute post-operative pain for the following reasons: no acute pain difference due to under-powered RCT, acute pain benefit revealed only 24 h after procedure, or using an uncommon instrument scale without a defined assessment time. Although the current study is a retrospective review of prospectively collected data, with the benefits of the relative larger sample size and correction of all the potential inter-group biases with a multivariable linear model, it resulted in clear benefits for non-mechanical fixation in reducing acute pain in the first few hours and on the first day.
The questionnaire for convalescence after TEP repair is scarce for previous RCTs. There was only one trial which compared quality of life (QOL) scores 4 weeks and 6 months after the procedure, revealing no differences between mechanical tacking and non-mechanical bio-glue fixation [17]. According to the literature and our experiences, the activity or QOL scores are usually contrary to the presentation timing of acute pain. These scores usually reach the lowest point immediately after the procedure then progressively return to pre-operative status with time. Therefore, late evaluation (> 7 days) of activity or QOL scores for a minor surgery, like laparoscopic TEP repair, logically demonstrates a negative result. The early recovery period after groin hernia repair is of the most importance to hernia patients in predicting the duration of sick leave after the procedure. Our comprehensive time scale evaluation with the modified MOS provided valuable clinical information that the non-mechanical glue fixation is superior to the mechanical stapling fixation early after the laparoscopic TEP repair for groin hernias.
Chronic pain is an undesirable problem after hernia surgery, and reducing chronic pain is also the main purpose of using glue fixation. Many variables, such as the sex, age, BMI, pore size of the mesh, operative dissection method, intra-operative complication, and fixation method, might affect the results [4]. After correcting for these confounding factors, no significant difference in chronic pain between groups was observed in our study. Similar findings were noted in the previous randomized control trials [15,16,17,18]. In addition, a nationwide register-based study also revealed no statistical difference in chronic pain between laparoscopic TEP with tack or glue fixation [7]. Therefore, we conclude, glue fixation is not beneficial in reducing the incidence of chronic pain in laparoscopic TEP repair.
Post-operative pain, one of the most important outcome parameters after laparoscopic groin hernia repair, had rarely been compared between primary and recurrent hernia repairs. A Herniamed Registry study in 2016, which compared the outcome differences between laparoscopic repair for primary and recurrent inguinal hernias, revealed significant differences in pain at rest (4.08 and 6.16%), pain on exertion (8.03 and 11.44%), and chronic pain requiring treatment (2.31 and 3.83%) [19]. Therefore, they conclude, post-operative pain is still more common in recurrent inguinal hernia repair than that in primary repairs even in the laparoscopic era. In our sub-group analysis, however, glue fixation for recurrent hernia is associated with lower acute post-operative pain, but it is not associated with more chronic pain or further recurrence. This is the first study that details the clinical benefits of non-mechanical (glue) fixation in laparoscopic recurrent hernia repair, which improved the functional activity and pain score in patients with recurrent inguinal hernias.
Although the laparoscopic mesh repair technique has the advantage of a tension free design, early or late mesh migration, either due to patient’s activity or a large hernia defect, is still a concern when using a non-mechanical or no fixation method. Previous clinical trials and this study showed no differences in recurrence rate between these non-mechanical and mechanical fixation methods. [15,16,17,18] In a retrospective single-arm study with 10-year follow-up, the recurrence rate was only 1.1% from 703 patients undergoing laparoscopic TEP with glue fixation [20]. Though this is not a comparative study, the reported recurrence rate of glue fixation seems comparable to tack fixation. Although the current study also revealed no difference in the recurrence rate between difference fixation methods, it was limited by its relative short follow-up period and non-randomized trial. Therefore, a RCT with long-term follow-up is still essential to confirm this issue.
The median operative time in the glue group is longer than the tack group. It might result from no commercial device for laparoscopic glue fixation. It took more time when we applied glue through a 5 Fr. catheter. We found more peri-operative complications in the glue fixation group, such as post-operative urinary retention and intra-operative peritoneal tear. We also found the patients in the glue group were significantly older than those in the tack group. We proposed that the older the patient the higher the possibility that there was a benign prostate obstruction, which commonly leads to urinary retention after groin surgery. In addition, older patients are also associated with more connective tissue weakness due to aging and thus face a higher possibility of peritoneal tear during dissection.
After we adjusted for age and other confounding factors, we did not find significant differences in peri-operative complications among groups. Beside these, there was only one randomized trial that revealed a higher incidence of seroma formation in patients with glue fixation [15]. However, other randomized trials and our study all showed no significant difference in seroma formation between different fixation methods in laparoscopic TEP repair [16,17,18]. Therefore, we propose that in the typical glue fixation method, the glue fixation itself did not lead to seroma formation in the hernia sac, but it may be related to some specific glue application methods which might impair serous fluid absorption or seal the serous fluid in the sac after the surgery. Further evaluation of the association between glue fixation technique and seroma formation is essential in the near future.
The choice of heavyweight or lightweight mesh was according to patient’s preference randomly. Therefore, the main drawback of this observational study is inter-group heterogeneity among some major confounding factors, such as age, BMI, and mesh materials. To correct this heterogeneity or to minimize the heterogeneity induced bias, data processing and analysis through statistical methods are commonly used in the literature. To account for differences in observed confounders in the treatment groups, investigators must frequently carry out analytic adjustments to control confounding when estimating treatment effects. The most common adjustment method is logistic regression of the outcome on treatment and a subset of the pretreatment confounders. The alternative popular methods for control of confounding in observational studies are based on the propensity score matching. In the current study, we used multivariable regression to adjust this variable (mesh material) in Tables 4 and 5.
In fact, we also tried to adjust our data by using propensity matching analysis before our submission. The patients were divided into tack mesh fixation and glue mesh fixation groups. The 70 patients in the glue group were matched in a case–control approach with the propensity score analysis with 583 patients in the tack group. To increase comparability between the two groups, propensity score matching on a 1:3 basis was performed using R version 3.6.1 by matching. Patients were matched based on sex, age and mesh material. Finally, 186 patients were extracted from 583 patients, with no significant differences in the aforementioned variables between the two groups. (Supplement Tables 1 and 2) According to this propensity score-matching method, we actually found similar outcomes as is the logistic regression analysis. Based on these two statistical adjustment analyses, we drew a solid conclusion that the glue fixation method was superior to tack fixation method in acute post-operative pain and early post-operative activity level after laparoscopic TEP repair. However, both fixation methods had similar incidence of chronic pain after laparoscopic TEP repair.
There are still some other limitations of the current study. First, although all data were prospectively collected in our database, selection bias cannot be avoided due to its retrospective nature. Second, for recurrence, the follow-up time should be longer to get more convincing results. Finally, the study was derived from a single experienced surgeon in a single institution. Therefore, these results may not be applicable to other centers with different case loads and experience.
In conclusion, the non-mechanical fixation method was superior to the mechanical fixation method in acute post-operative pain and early post-operative activity level after laparoscopic TEP repair. However, both fixation methods had similar incidence of chronic pain-, recurrence-, and procedure-related complications after laparoscopic TEP repair. In addition, our study also revealed that TEP with glue fixation improved both the functional activity and pain score in patients with recurrent inguinal hernias. However, a large-scale RCT with long-term follow-up is vital to clarify these unsolved issues in hernia recurrence.
References
Langeveld HR, van’t Riet M, Weidema WF, Stassen LP, Steyerberg EW, Lange J, Bonjer HJ, Jeekel J (2010) Total extraperitoneal inguinal hernia repair compared with Lichtenstein (the LEVEL-Trial): a randomized controlled trial. Ann Surg 251:819–824
Schmedt CG, Sauerland S, Bittner R (2005) Comparison of endoscopic procedures vs Lichtenstein and other open mesh techniques for inguinal hernia repair: a meta-analysis of randomized controlled trials. Surg Endosc 19:188–199
Aasvang EK, Mohl B, Bay-Nielsen M, Kehlet H (2006) Pain related sexual dysfunction after inguinal herniorrhaphy. Pain 122:258–263
Niebuhr H, Wegner F, Hukauf M, Lechner M, Fortelny R, Bittner R, Schug-Pass C, Kockerling F (2018) What are the influencing factors for chronic pain following TAPP inguinal hernia repair: an analysis of 20,004 patients from the Herniamed Registry. Surg Endosc 32:1971–1983
Wong JU, Leung TH, Huang CC, Huang CS (2011) Comparing chronic pain between fibrin sealant and suture fixation for bilayer polypropylene mesh inguinal hernioplasty: a randomized clinical trial. Am J Surg 202:34–38
Antoniou SA, Kohler G, Antoniou GA, Muysoms FE, Pointner R, Granderath FA (2016) Meta-analysis of randomized trials comparing nonpenetrating vs mechanical mesh fixation in laparoscopic inguinal hernia repair. Am J Surg 211:239–249.e232
Gutlic N, Rogmark P, Nordin P, Petersson U, Montgomery A (2016) Impact of mesh fixation on chronic pain in total extraperitoneal inguinal hernia repair (TEP): a nationwide register-based study. Ann Surg 263:1199–1206
Chung SD, Huang CY, Chueh SC, Tsai YC, Yu HJ (2011) Feasibility and safety of total extraperitoneal inguinal hernia repair after previous lower abdominal surgery: a case-control study. Surg Endosc 25:3353–3356
Chung SD, Huang CY, Wang SM, Hung SF, Tsai YC, Chueh SC, Yu HJ (2011) Laparoendoscopic single-site totally extraperitoneal adult inguinal hernia repair: initial 100 patients. Surg Endosc 25:3579–3583
Tsai YC, Ho CH, Tai HC, Chung SD, Chueh SC (2013) Laparoendoscopic single-site versus conventional laparoscopic total extraperitoneal hernia repair: a prospective randomized clinical trial. Surg Endosc 27:4684–4692
Lin CD, Wu CH, Liu YB, Tsai YC (2016) Feasibility and safety of laparoendoscopic single-site surgery of total extraperitoneal inguinal hernia repair after previous open groin hernia repair: a comparative study. Surg Endosc 30:2086–2089
Wu CC, Chueh SC, Tsai YC (2016) Is contralateral exploration justified in endoscopic total extraperitoneal repair of clinical unilateral groin hernias—a prospective cohort study. Int J Surg (London, England) 36:206–211
Liem MS, van der Graaf Y, van Steensel CJ, Boelhouwer RU, Clevers GJ, Meijer WS, Stassen LP, Vente JP, Weidema WF, Schrijvers AJ, van Vroonhoven TJ (1997) Comparison of conventional anterior surgery and laparoscopic surgery for inguinal-hernia repair. N Engl J Med 336:1541–1547
(1999) Laparoscopic versus open repair of groin hernia: a randomised comparison. The MRC Laparoscopic Groin Hernia Trial Group. Lancet (London, England) 354:185-190
Lau H (2005) Fibrin sealant versus mechanical stapling for mesh fixation during endoscopic extraperitoneal inguinal hernioplasty: a randomized prospective trial. Ann Surg 242:670–675
Subwongcharoen S, Ruksakul K (2013) A randomized controlled trial of staple fixation versus N-butyl-2-cyanoacrylate fixation in laparoscopic inguinal hernia repair. J Med Assoc Thail 96(Suppl 3):S8–13
Chan MS, Teoh AY, Chan KW, Tang YC, Ng EK, Leong HT (2014) Randomized double-blinded prospective trial of fibrin sealant spray versus mechanical stapling in laparoscopic total extraperitoneal hernioplasty. Ann Surg 259:432–437
Moreno-Egea A (2014) Is it possible to eliminate sutures in open (Lichtenstein technique) and laparoscopic (totally extraperitoneal endoscopic) inguinal hernia repair? A randomized controlled trial with tissue adhesive (n-hexyl-alpha-cyanoacrylate). Surg Innov 21:590–599
Kockerling F, Jacob D, Wiegank W, Hukauf M, Schug-Pass C, Kuthe A, Bittner R (2016) Endoscopic repair of primary versus recurrent male unilateral inguinal hernias: are there differences in the outcome? Surg Endosc 30:1146–1155
Berney CR, Descallar J (2016) Review of 1000 fibrin glue mesh fixation during endoscopic totally extraperitoneal (TEP) inguinal hernia repair. Surg Endosc 30:4544–4552
Author information
Authors and Affiliations
Corresponding authors
Ethics declarations
Disclosures
Dr. Chih-Chin Yu, Ching-Shui Huang, Yung-Tai Chen, Shih-Chieh Jeff Chueh, Chi-Wen Lo, and Yao-Chou Tsai have no conflicts of interest or financial ties to disclose.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Yu, CC., Chen, YT., Huang, CS. et al. A comprehensive study comparing tack and glue mesh fixation in laparoscopic total extraperitoneal repair for adult groin hernias. Surg Endosc 34, 4486–4493 (2020). https://doi.org/10.1007/s00464-019-07234-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00464-019-07234-7