Abstract
Background
In the last few years, technical advances have produced a dramatic shift from traditional open surgery toward a minimally invasive approach, even in oncological procedures. We present our initial experience with laparoendoscopic single-site surgery (LESS) in the surgical treatment of early-stage endometrial cancer patients.
Methods
Between July 2009 and May 2010, 20 consecutive low-risk early endometrial cancer patients were enrolled in this single institution prospective cohort trial.
Results
The median age of the patients was 57 years (range = 42–68) and median body mass index was 24 kg/m2 (range = 21–30). Median operative time was 105 min (range = 85–155) and median estimated blood loss was 20 ml (range = 10–180). The larger skin and fascial incision required for the single-port approach was 2.5 cm (median = 2.2 cm; range = 2.0–2.5). No laparoscopic/laparotomic conversion was registered, and no insertion of additional ports was necessary. Median ileus was 16 h (range = 12–20) and median time to discharge was 1 day (range = 1–2). All patients were completely satisfied with the cosmetic results and postoperative pain control.
Conclusions
Laparoendoscopic single-site surgery could represent a surgical option for extra-fascial hysterectomy in early-stage endometrial cancer patients, with the potential to further decrease invasiveness of the conventional laparoscopic approach.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
The undeniable advantages of laparoscopic surgery (LPS) have made it increasingly attractive as an alternative to laparotomy for the treatment of gynecological malignancies, especially for the management of early endometrial cancer [1, 2]. In recent years, many authors have demonstrated the feasibility of LPS in these women [3, 4] and its superiority in terms of postoperative pain and shorter hospital stay [5]. There seem to be the same or fewer postoperative complications after LPS than after laparotomy [6], probably because of the laparoscopic expertise of the operating surgeon and the patient’s comorbidities. Interestingly, this approach does not seem to modify the incidence of recurrence and overall survival [7]. More recently, robot-assisted LPS has been proposed as a minimally invasive alternative to LPS for the treatment of endometrial cancer. Robotic procedures have been used increasingly and initial studies are promising, showing an improved operative time compared to LPS [8, 9]; however, they are more costly and require more and larger ports than standard LPS.
Currently, the efforts of laparoscopic surgeons are aimed at further reducing the morbidity associated with minimally invasive technology while maintaining the same high standard of surgical care. One way to achieve this goal is to perform laparoendoscopic single-site surgery (LESS). Preliminary results suggest an early postoperative benefit in terms of postoperative pain for the LESS patients compared to standard LPS patients [10–12]. As far as hysterectomy is concerned, there are two case–control studies showing the feasibility of total-LESS [11] or LESS-assisted vaginal hysterectomy [12] in benign uterine disease.
The aim of this pilot study was to evaluate the feasibility of the total-LESS approach in a consecutive series of low-risk early endometrial cancer patients.
Material and methods
Patients and surgical characteristics
Between July 1, 2009, and May 28, 2010, 72 endometrial cancer patients were referred to the Division of Gynecologic Oncology, Department of Obstetrics and Gynecology, Catholic University of the Sacred Heart in Rome, Italy. All these patients were prospectively evaluated for LESS treatment. Inclusion criteria were FIGO stage IA; well (G1) and moderate (G2) differentiated endometrial cancer and no evidence of lymph node and/or adnexal and/or cervical involvement at computed tomography/magnetic resonance imaging; adequate vaginal access; uterine size <12 weeks of pregnancy; no history of previous longitudinal major surgery; BMI ≤ 35, and ASA score ≤ II.
The study was approved by the institutional review board, and patients were informed about the LESS technique and signed a written informed consent acknowledging the risk of laparoscopic and/or laparotomic conversion.
Patient demographics and surgical and postoperative data were prospectively collected. Clinical and diagnostic information regarding actual disease was also noted. Operative time (OT) was defined as the interval between incision start to closure. Operative complications were defined as bowel, bladder, ureteral, or vascular injuries, and an estimated blood loss (EBL) > 500 ml. Anemia was considered when hemoglobin levels were <8 g/dl and fever when body temperature was at least 38°C in two consecutive measurements at least 6 h apart, excluding the first day after surgery. Postoperative pain assessment (in the immediate postoperative period and 7–14 days postoperatively) was performed in all patients using a validated Visual Analog Pain Scale (VAS) and scored from 0 to 10 (0 = no pain and 10 = agonizing pain). After surgery, analgesic therapy with paracetamol 1,000 mg was administered only on the patient’s demand. Patients were allowed to go home when they were fully mobile, apyrexial, and passing urine satisfactorily. Postoperative complication was defined as any adverse event that occurred within 30 days from surgery and was considered severe if it resulted in unplanned admission, blood transfusion, or a secondary surgical procedure.
Cosmetic outcome of the umbilical scar was evaluated at day 1 and at day 30 after surgery by the patient and by the surgeon separately, expressing a subjective satisfaction value from 1 to 10 (0 = bad and 10 = excellent).
Surgical technique
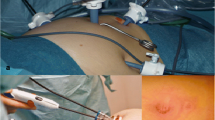
While under general anesthesia the patient was positioned in the dorsal lithotomic position with both legs supported in stirrups with a Trendelenburg tilt. In order to achieve an ergonomic approach, the first surgeon was positioned at the head of the patient, the first assistant (video laparoscope) was at the right side (sitting), and the second assistant (uterine manipulator) was in the middle between the legs (Fig. 1). The surgical procedure was performed through a multichannel single port (TriPort, Olympus Winter & Ibe GmbH, Hamburg, Germany), as previously reported [13–15].
Once pneumoperitoneum (12 mmHg) was achieved, intra-abdominal visualization was obtained with a 5-mm 30° telescope with flexible handling (EndoEYE, Olympus Winter & Ibe GmbH) or, alternatively, with a 5-mm 0° telescope with a flexible tip (EndoEYE) (Fig. 3A). Working straight and/or double-bended 5-mm instruments (Olympus Winter & Ibe GmbH) were inserted into the remaining two ports; these included grasper, cold scissor, suction/irrigation bipolar coagulator, and a multifunctional versatile laparoscopic device that grasps, coagulates, and transects simultaneously (PKS cutting forceps, 5–43 cm, Gyrus ACMI, Hamburg, Germany) (Fig. 3A). A combination of a standard 33-cm-long straight instrument with a 43-cm-long straight instrument or a straight instrument with a double-bended one was adopted in order to prevent clashing between instruments and to facilitate surgical maneuvers. Changes in the position of the instruments and optics were carried out according to the needs of the surgeon.
A careful inspection of the entire abdominal cavity was performed as the first surgical step in order to identify any suspicious peritoneal lesion that would exclude the patient from having the procedure completed by laparoscopy. Peritoneal washing was routinely performed. After bilateral cauterization of the fallopian tubes, an intrauterine manipulator was positioned. After coagulation and section of the right round ligament and access into the retroperitoneal space, the ureter was visualized and a hemostatic clip was positioned at the origin of the uterine artery (Fig. 2). Adnexal resection was performed throughout using PKS bipolar cutting forceps. In order to safely cauterize and dissect the ovarian vessels, a window was opened between the left ovarian pedicle above and the ureter below. The vesicouterine and vesicovaginal spaces were developed starting from the lateral peritoneal incisions and the fascia covering the cervix, displaying the upper third of the vagina. The posterior peritoneum was incised, developing the cranial part of the rectovaginal space. This procedure allows excellent skeletonization of the uterine vessels, medially to the ureter along the uterus, which can be easily cauterized and sectioned. Consequently, an adequate margin of the vagina was prepared to perform colpectomy using a bipolar hook (PKS Plasma J hook, Gyrus ACMI, Hamburg, Germany) or a double-bended monopolar hook. The vagina was incised circumferentially following the porcelain valve of the uterine manipulator as a guide. The uterus and the adnexa were extracted through the vagina and sent for frozen section. During the procedure, the manipulator was never removed from the uterus in order to avoid any leakage of cancer cells through the cervix. The vaginal vault was closed with single stitches using the extracorporeal knotting technique or the vaginal way. A hydropneumatic test for bladder integrity was performed at the end of the procedure. Each layer of the access port is separately sutured.
A frozen section analysis was performed for all patients. According to our internal protocol, lymph node dissection was judged unnecessary for low-risk early-stage endometrial cancer.
Statistical analysis
Statistical analysis was performed using the Mann-Whitney test to evaluate the relationship between pairs of categorical variables. Differences between the groups were considered statistically significant at P ≤ 0.05 (95% confidence interval).
Results
During the study period, 20 of 72 patients (27.8%) met all the inclusion criteria and were enrolled in this trial. No possible candidate patient refused to be enrolled in the study. Table 1 shows the clinicopathological and procedural characteristics of the study population. The median age was 57 (range = 42–68) and median BMI was 26 kg/m2 (range = 21–32). In 10 patients (50%), previous minor abdominal surgical procedures were found. Median EBL and OT were 20 ml (range = 10–180) and 105 min (range = 85–155), respectively. As shown in Fig. 4, after one half of the cases (10 patients), we observed a significant decrease in the median OT (95 vs. 117.5 min; P < 0.0001). The larger skin and fascial incision required by the LESS approach was 2.5 cm (median = 2.2 cm; range = 2.0–2.5). The median time to introduce the port from skin incision to the start of achieving pneumoperitoneum required was 75 s (range = 45–190).
Port placement was successfully executed in all cases without incident or inadvertent port removal. No fascial, vascular, or visceral injuries, loss of pneumoperitoneum, or intraoperative port-site bleeding occurred. In all patients, a total LESS hysterectomy was performed without conversion and additional port insertion. The vaginal cuff was closed by laparoscopy or by vaginal way in 8 (40%) and 12 patients (60%), respectively.
In all but two patients (90%), frozen section analysis confirmed the presence of low-risk early endometrial cancer. In the remaining 2 cases (10%), a pelvic lymphadenectomy throughout a conversion to standard LPS was performed.
After surgery there was no wound hematoma, wound infection, or delayed bleeding. Median time of ileus was 16 h (range = 12–20). Median time to discharge was 1 day (range = 1–2): on day 1 in 17 cases (85.0%) and on day 2 in 3 cases (15.0%).
Definitive histology substantially confirmed frozen section analysis, except for one case that was managed without lymphadenectomy in which a cervical stroma involvement was found. In this patient, after adequate counseling, a laparoscopic pelvic lymphadenectomy was performed and adjuvant treatment was administered.
All patients conveyed complete satisfaction with the cosmetic result and postoperative pain control. Median postoperative pain evaluation according to the VAS scale at rest and after Valsalva’s maneuver is reported in Table 2. Although no patient required analgesic therapy 20 min after surgery, the median VAS value at rest was 3 (range = 1–7) after 2 h, while it was 4 (range = 2–8) after Valsalva’s maneuver. The perception of pain progressively decreased during the next evaluations: at 8 h the VAS was 2 (range = 2–5) at rest and 3 (range = 2–6) after Valsalva’s maneuver. All patients were discharged home with optional analgesic therapy only. After 7 days the median VAS score was 2 (range = 1–3) at rest and 2 (range = 1–3) after Valsalva’s maneuver. The VAS evaluation was repeated 14 days after surgery: median value was 1 (range = 0–2) at rest and also after Valsalva’s maneuver.
On discharge, median satisfaction values with respect to cosmetic outcome (Fig. 3B) expressed by the patient and the surgeon were 8 (range = 7–9) and 9 (range = 7–10), respectively. Thirty days later, the median values improved to 9 (range = 8–9) and 9 (range = 9–10), respectively. No complications were registered in the early (30 days) postoperative period.
Discussion
The role of minimally invasive surgery for early endometrial cancer patients continues to evolve. Data from the literature has confirmed that standard and robot-assisted LPS are associated with safe and effective outcomes that are comparable to those reported for laparotomic treatment of endometrial cancer [1–3]. Thanks to these data, minimally invasive surgery has become the gold standard in the surgical management of these patients.
In recent years, many efforts have been made by laparoscopic surgeons to further reduce the surgical invasiveness of minimally invasive approaches. One way to achieve this goal is to reduce the trauma of access ports by reducing their size to a 3-mm diameter or less or perform surgery using single-port access.
We have previously reported our first case of total LESS hysterectomy [13] and, in the last year, other authors have shown the feasibility of total LESS [11] and LESS-assisted vaginal hysterectomy for the management of benign and preneoplastic uterine disease [12]. As far as gynecological cancer is concerned, some authors [14, 16] described the feasibility of single-port surgery for specific situations such as early endometrial cancer and BRCA1 + patients who are to undergo hysterectomy and bilateral salpingo-oophorectomy.
To our knowledge, ours is the first pilot study aimed at evaluating the feasibility and the early postoperative outcomes of total LESS hysterectomy in a consecutive series of low-risk early endometrial cancer patients. We were able to complete the total hysterectomy successfully without conversion to standard laparoscopy, insertion of an additional port, or intraoperative and early postoperative complications. Conversion to standard laparoscopy was necessary in two cases in order to perform a safe and radical pelvic lymphadenectomy, according to the frozen sections analysis on the specimen. Median operative time was longer compared to standard LPS [1–4], but in our study we observed a rapid trend in the decrease in operative time after almost ten procedures (Fig. 4). Even though the number of cases in our study is small, our results in terms of postoperative outcomes are substantially comparable to those reported for standard laparoscopy [1–4]. Moreover, as we previously reported for benign adnexal disease [10], previous surgery in the patient does not prevent us from performing this technique.
The surgical technique of the LESS approach is the same as that for standard laparoscopic hysterectomy at our institution; this is important because we believe that single-access surgery should be like the standard laparoscopic technique in order to maintain safety, reproducibility, and oncologic criteria. In this context it is important to point out some specific technical issues that allow to us overcome some specific limitations of single-port surgery, such as reduced visualization, loss of triangulation, and instrument interference, as recently reported by Ramirez [15]: (1) use of a 5-mm 30° telescope with a flexible handle or alternatively, a 5-mm 0° video laparoscope with a flexible tip (Fig. 3A); (2) use of two straight instruments of different lengths (43 and 33 cm long) or double-bent instruments to reduce clashing and changing (Fig. 3A); (3) multifunctional instruments that are able to grasp, coagulate, and dissect; (4) uterine manipulator reducing the limits due to the absence of an auxiliary port; and (5) closure of the uterine artery at the origin (Fig. 2), after adequate extraperitoneal dissection and ureter visualization, to reduce the need of bipolar coagulation at the paracervical region, with lower risk of bleeding and ureter injury. Thanks to all these solutions, in this initial experience we performed total LESS hysterectomy without an additional port, as proposed by others [17]; we used the transumbilical port during the whole procedure. Furthermore, we believe that these arrangements, together with progressive improvement in surgical skills, could facilitate the use of the total LESS hysterectomy procedure by decreasing the initial difficulties related to this new approach by progressively lowering the OT and offering some advantages in terms of less invasiveness, faster recovery time, less postoperative pain, and better cosmetic outcome.
Presently, at our department we aim to expand the gynecological indications for the use of the LESS approach and to standardize this innovative technique and help it spread into a greater number of hospital situations. LESS appears to be a safe and adequate surgical option for hysterectomy in low-risk early endometrial cancer patients, with the potential to further decrease the invasiveness of the conventional laparoscopic approach and minimize morbidity. Furthermore, a recent report [18] described the technique and the feasibility of single-port laparoscopic pelvic and para-aortic node sampling and lymphadenectomy.
Single port represents the last revolution in minimally invasive surgery, and innovative instruments and methods will continue to evolve as technology advances. Like any refinement of an accepted technique, and even more in the setting of cancer patient treatment, it needs close scrutiny. A prospective clinical trial comparing LESS to standard LPS is essential to discern and to what extent incremental benefits exist.
References
Magrina JP (2005) Outcomes of laparoscopic treatment for endometrial cancer. Curr Opin Obstet Gynecol 17:343–346
Tozzi R, Malur S, Koehler C, Schneider A (2005) Analysis of morbidity in patients with endometrial cancer: is there a commitment to offer laparoscopy? Gynecol Oncol 97:4–9
Palomba S, Falbo A, Mocciaro R, Russo T, Zullo F (2009) Laparoscopic treatment for endometrial cancer: a meta-analysis of randomized controlled trials (RCTs). Gynecol Oncol 112:415–421
Malzoni M, Tinelli R, Cosentino F, Perone C, Rasile M, Tinelli A (2009) Total laparoscopic hysterectomy versus abdominal hysterectomy with pelvic lymphadenectomy for early-stage endometrial cancer: a prospective randomized study. Gynecol Oncol 112:126–133
Langerbrekke A, Istre O, Hallqvist AC, Hartgill TW, Onsrud M (2002) Comparison of laparoscopy and laparotomy in patients with endometrial cancer. J Am Assoc Gynecol Laparosc 9:152–157
Tinelli R, Malzoni M, Cicinelli E, Fiaccavento A, Zaccoletti R, Barbieri F, Tinelli A, Perone C, Cosentino F (2011) Is early stage endometrial cancer safely treated by laparoscopy? Complications of a multicenter study and review of recent literature. Surg Oncol 20(2):80–87
Ghezzi F, Cromi A, Uccella S, Siesto G, Giudici S, Serati M, Franchi M (2010) Laparoscopic versus open surgery for endometrial cancer: a minimum 3-year follow-up study. Ann Surg Oncol 17:271–278
Bandera CA, Magrina JF (2009) Robotic surgery in gynecologic oncology. Curr Opin Obstet Gynecol 21:25–30
Peiretti M, Zanagnolo V, Bocciolone L, Landoni F, Colombo N, Minig L, Sanguineti F, Maggioni A (2009) Robotic surgery: changing the surgical approach for endometrial cancer in a referral cancer center. J Minim Invasive Gynecol 16:427–431
Fagotti A, Rossitto C, Marocco F, Gallotta V, Bottoni C, Scambia G, Fanfani F (2011) Perioperative outcomes of laparoendoscopic single-site surgery (LESS) versus conventional laparoscopy for adnexal disease: a case-control study. Surg Innov 18(1):29–33
Yim GW, Jung YW, Paek J (2010) Transumbilical single-port access versus conventional total laparoscopic hysterectomy: surgical outcomes. Am J Obstet Gynecol 203:26.e1–26.e6
Kim TJ, Lee YY, Cha HH (2010) Single-port-access laparoscopic-assisted vaginal hysterectomy versus conventional laparoscopic-assisted vaginal hysterectomy: a comparison of perioperative outcomes. Surg Endosc 24:2248–2252
Fanfani F, Fagotti A, Scambia G (2010) Laparoendoscopic single-site surgery for total hysterectomy. Int J Gynaecol Obstet 109:76–77
Escobar PF, Starks DC, Fader AN, Barber M, Rojas-Espalliat L (2010) Single-port risk-reducing salpingo-oophorectomy with and without hysterectomy: surgical outcomes and learning curve analysis. Gynecol Oncol 119:43–47
Ramirez PT (2009) Single-port laparoscopic surgery: Is a single incision the next frontier in minimally invasive gynecologic surgery? Gynecol Oncol 114:143–144
Fader AN, Escobar PF (2009) Laparoendoscopic single-site surgery (LESS) in gynecologic oncology: technique and initial report. Gynecol Oncol 114:157–161
Lee YY, Kim TJ, Kim CJ (2009) Single-port access laparoscopic-assisted vaginal hysterectomy: a novel method with a wound retractor and a glove. J Minim Invasive Gynecol 16:450–453
Escobar PF, Fader AN, Rasol N (2010) Single-port laparoscopic pelvic and para-aortic node sampling or lymphadenectomy: development of a technique and instrumentation. Int J Gynecol Cancer 20:1268–1273
Disclosure
F. Fanfani, C. Rossitto, M. L. Gagliardi, V. Gallotta, S. Gueli Alletti, G. Scambia, and A. Fagotti have no conflicts of interest or financial ties to disclose.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Fanfani, F., Rossitto, C., Gagliardi, M.L. et al. Total laparoendoscopic single-site surgery (LESS) hysterectomy in low-risk early endometrial cancer: a pilot study. Surg Endosc 26, 41–46 (2012). https://doi.org/10.1007/s00464-011-1825-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00464-011-1825-8