Abstract
Background
Endoscopic mucosal resection using a cap-fitted panendoscope (EMRC) and an endoscopic submucosal dissection (ESD) are increasingly performed to treat superficial esophageal carcinoma (SEC). As an endoscopic procedure appropriate for en bloc complete resection, ESD requires a much higher level of skill and experience than EMRC.
Methods
This retrospective study reviewed 127 SECs in 112 patients treated by EMRC or ESD from January 1997 to September 2009.
Results
For lesions 10 mm in diameter or smaller, EMRC and ESD had equivalent en bloc resection rates with tumor-free margins (en bloc + R0 resection rates). For lesions 11 mm in diameter or larger, however, the rate was significantly higher in the ESD group than in the EMRC group (p < 0.01). The mean procedure time was significantly longer in the ESD group than in the EMRC group (p < 0.01) regardless of lesion size. No significant difference was found in esophageal perforation rate between the EMRC and ESD groups. Severe esophageal stricture developed after EMRC of eight lesions (14.3%) and after ESD of six lesions (8.5%). For patients with a mucosal defect involving more than three-fourths of the esophageal circumference, the incidence of severe esophageal stricture after procedure was significantly higher in the EMRC group than in the ESD group (p < 0.05). The overall local recurrence rate was 3.1% (4/127) during an average follow-up period of 39 months (range, 8–123 months). All local recurrences were detected as superficial cancers after EMRC and then treated endoscopically.
Conclusions
For lesions 10 mm in diameter or smaller, EMRC was found to be optimal. For lesions 11 mm in diameter or larger, however, ESD was superior to EMRC in efficacy as assessed by the en bloc + R0 resection rate. Furthermore, ESD was advantageous in preventing stricture formation. The operating endoscopist should carefully select EMRC or ESD according to lesion size.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
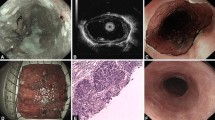
The frequency of detecting superficial esophageal carcinoma (SEC) has increased markedly with the recent technical innovation in endoscopy. Narrow-band imaging endoscopy was developed and found to be useful, especially for early detection of squamous cell carcinoma of the esophagus and pharynx [1, 2].
In Japan, SECs have been treated preferentially by endoscopic mucosal resection (EMR) [3] because the rates for surgical mortality and the incidence of postsurgical complications related to esophagectomy are high and because the patient’s quality of life is much better after EMR than after esophagectomy [4–6].
Long-term survival outcomes after EMR of the esophagus suggest a favorable prognosis [7]. However, conventional EMR techniques present limitations in terms of resectable lesion size, and large lesions should be resected in a piecemeal manner [8, 9]. Furthermore, the intense thermal denaturation of the lesion caused by the techniques have made it difficult to perform the precise histopathologic evaluation of the piecemeal-resected specimen needed to determine the risk for lymph node metastasis. In addition, local recurrence rates are reported to be higher after piecemeal resection than after en bloc resection [10].
Endoscopic submucosal dissection (ESD), a new endoscopic procedure that does not use a snare to dissect submucosal tissue, has the advantage of permitting en bloc and histologically complete resection of lesions. Developed for en bloc resection of gastric lesions about 10 years ago, ESD has been applied to the esophagus [11–14]. However, the lumen of the esophagus is narrow, and its thin wall constantly moves along with respiration and heartbeat. Therefore, ESD is more difficult to perform for esophageal than for gastric neoplasms. Using a cap-fitted panendoscope (EMRC) developed by Inoue et al. [15, 16], EMR is a much easier endoscopic procedure to master than ESD.
We retrospectively examined the clinical outcomes of EMRC and ESD for Japanese patients with SEC by assessing the following variables: en bloc resection rate with tumor-free margins (en bloc + R0 resection rate), mean procedure time, complication (perforation and bleeding) rate, incidence of severe esophageal stricture after procedure, and local recurrence rate.
Patients and methods
At Akita City Hospital, 155 esophageal cancers in 138 patients were treated by EMRC or ESD from January 1997 to September 2009. Our study enrolled 112 patients with 127 SECs who met the following eligibility criteria: histologically proven squamous cell carcinoma, tumor invasion depth of m1–sm1, no additional treatment immediately after procedure, no prior treatment of chemotherapy or radiation, and a patient follow-up period longer than 8 months with more than two follow-up endoscopies.
Chromoendoscopy by iodine staining has been conducted since the introduction of EMRC to determine the borders of the cancer area in all patients, whereas narrow-band imaging endoscopy with magnification has been performed since April 2007 to evaluate the depth of cancer invasion in all patients. All procedures were performed for patients under intravenous sedation with pentazocine (Pentazin; Sankyo Co., Ltd., Tokyo, Japan) and midazolam (Dormicam; Astellas Pharma Inc., Tokyo, Japan) or propofol (Diprivan; Astrazeneca KK, Osaka, Japan). Midazolam was used for sedation since January 1997 to March 2007, whereas propofol has been used during cardiorespiratory function monitoring since April 2007. The procedure was completed after total removal of an iodine-unstained lesion or after marking of a lesion. Circumferential resections were avoided due to the risk of provoking severe stricture formation postsurgery. Written informed consent was obtained from all the patients before the procedure was performed.
The EMRC procedure was performed from January 1997 to July 2003. For EMRC, a conventional endoscope having a single working channel (Q240; Olympus Optical Co, Ltd, Tokyo, Japan) with a plastic cap (distal attachment; Olympus, Tokyo, Japan) on its tip was introduced. An injection needle was used to inject the saline solution into the submucosa in an attempt to elevate the lesion above the muscle layer.
First, the mucosa was suctioned moderately to seal the outlet of the cap, and a small-diameter snare (SD-7P; Olympus), which passes through the instrumental channel of the endoscope, then was opened within the plastic cap. Second, the target mucosa was completely aspirated into the plastic cap and strangulated by the snare wire. A forced coagulation current then was applied to resect the lesion. If additional resection was necessary, all the steps of the procedure were repeated.
From August 2003 to September 2009, ESD was performed using a conventional endoscope with a single working channel (H260; Olympus). A disposable transparent attachment (D-201-1074; Olympus) was fitted onto the tip of the endoscope to obtain fine endoscopic views unaffected by respiratory movement and cardiac pulsation and to produce tension on connective tissue for submucosal dissection.
The ESD procedure was performed using an insulation-tipped diathermic (IT) knife (KD-610L; Olympus) and a conventional needleknife (KD-1L-1; Olympus) or a 2-mm short needleknife—a flush knife (DK2618JN20; Fujinon-Toshiba ES Systems Co., Ltd., Saitama, Japan). A conventional needleknife has been used since its introduction in April 2004, and a flush knife was used from May 2004 to September 2009.
The ESD procedure was performed as follows. Several points of the lesion were marked approximately 3 mm outside its margin using a needleknife and a forced coagulation current of 25 W (ICC 200; Erbe Elektromedizin Ltd, Tubingen, Germany). A glycerol and sodium hyaluronate solution containing small amounts of indigo carmine and epinephrine was injected into the submucosa. Next, a mucosal incision at the periphery of the lesion and marking of the lesion were performed with a needleknife and an IT knife in the end-cut mode (80 W). Additional glycerol was injected into the submucosal layer, and submucosal connective tissue beneath the lesion was dissected using a needleknife and an IT knife.
Resected specimens cut into 2-mm slices were examined histologically according to the Japanese Classification of Esophageal Carcinoma [17]. A carcinoma that extended up to 200 μm below the lower border of the lamina muscularis mucosae was defined as sm1. Patients whose histopathologic diagnosis involved a cancer invasion depth reaching the muscularis mucosae (m3) with vascular infiltration or reaching the submucosa (sm) with or without vascular infiltration were recommended to undergo additional treatments (e.g., esophagectomy with lymph node dissection or radiation therapy with or without chemotherapy against possible lymph node metastases).
The en bloc + R0 resection rate, mean procedure time, complication (perforation and bleeding) rate, incidence of severe esophageal stricture after procedure, and local recurrence rate were evaluated. The en bloc + R0 resection rate was further evaluated for lesion size. Procedure time, defined as the time from the moment of lesion marking to the completion of lesion resection, was measured. Perforation was diagnosed endoscopically when mediastinal connective tissue was observed during the procedure.
Bleeding related to the procedure was defined as bleeding that required postoperative hemostatic treatments (e.g., endoscopic clipping and surgical intervention). Severe esophageal stricture after procedure was present when a standard 11-mm-diameter endoscope could not pass through the stricture. Mucosal defects involving the esophageal circumference were categorized based on the following reference extents of involvement: three-fourths or less and more than three-fourths. Follow-up endoscopic examinations usually were performed 2 and 8 months after procedure, then annually thereafter. The presence of lymph node or distal metastases was evaluated by computed tomography at least once a year.
Differences in the en bloc + R0 resection rate, complication rate, and local recurrence rate between the EMRC and ESD groups were compared according to the Chi-square test. The Student’s t-test was performed concerning the mean procedure time. A p value less than 0.05 was considered statistically significant. A statistical software program (StatView; Abacus Concepts, Inc, Berkeley, CA, USA) was used for all statistical analyses.
Results
The clinicopathologic features of 127 SECs are shown in Table 1. There were no significant differences in lesion size, location, or depth of cancer invasion between the EMRC and ESD groups.
The en bloc + R0 resection rates in the EMRC and ESD groups according to lesion size are shown in Table 2. The EMRC and ESD groups showed equivalent en bloc + R0 resection rates for lesions 10 mm in diameter or smaller. For lesions 11 mm in diameter or larger, however, the ESD group had significantly higher histologically complete resection rates than the EMRC group (p < 0.01).
The mean procedure time was significantly longer in the ESD group than in the EMRC group regardless of lesion size (p < 0.01) (Table 3). Namely, the time in the ESD group was 43.5 ± 15.3 min also for lesions 10 mm in diameter or smaller.
The incidences of esophageal perforation according to lesion size are shown in Table 4. No significant differences were found between the EMRC and ESD groups with respect to any lesion size. All patients who had esophageal perforation could be treated conservatively by endoscopic clipping, intubation with a nasogastric tube, discontinuation of oral intake, and intravenous administration of antibiotics. There was no case of postoperative bleeding. Bleeding during procedure was frequent but managed successfully with hemostatic forceps (HDB2422 W; Pentax Ltd, Tokyo, Japan) in all cases.
The extents of mucosal defects and the incidences of severe esophageal stricture after procedure are shown in Table 5. The overall incidence of severe esophageal stricture was 14.3% after EMRC and 8.5% after ESD (nonsignificant difference). For patients with mucosal defects involving more than three-fourths of the esophageal circumference, however, the incidence of severe esophageal stricture was significantly higher after EMRC than after ESD (p < 0.05). All patients who had severe esophageal stricture after procedure were treated successfully by endoscopic balloon dilation.
Local recurrence rates for SEC in the EMRC and ESD groups are shown in Table 6. The overall local recurrence rate was 3.1% (4/127) during the average follow-up period of 39 months (range, 8–123 months). The EMRC and ESD groups showed no local recurrence with respect to lesions 10 mm in diameter or smaller. However, the local recurrence rate was significantly higher in the EMRC group than in the ESD group for lesions 21 mm in diameter or larger (p < 0.05). All local recurrences treated by EMRC were detected as superficial cancers and re-treated by additional endoscopic treatments (e.g., ESD or argon plasma coagulation). No treatment- or esophageal cancer-related deaths occurred in this study.
Discussion
Simple and easy to perform, EMRC has been widely accepted as a clinically useful endoscopic procedure for SEC in Japan. However, EMRC involves difficulty in conducting the en bloc complete resection of lesions 21 mm in diameter or larger [8, 9], although the latter approach seems to be the ideal procedure for reducing the local recurrence rate for SEC and for making an accurate histopathologic evaluation of the tumor. On the other hand, ESD is the best procedure for performing en bloc resection, but the procedure requires a high level of skill and experience [18–21]. Especially, esophageal ESD is more difficult to perform than gastric ESD because the wall is thinner in the esophagus than in the stomach and constantly moves along with respiration and heartbeat. Therefore, the selection of an adequate endoscopic procedure for SEC is very important.
In the current study, both the EMRC and ESD groups succeeded with en bloc complete resection of all lesions 10 mm in diameter or smaller. Furthermore, the EMRC group presented a much shorter mean procedure time than the ESD group. Therefore, EMRC was found to be the best endoscopic procedure for lesions 10 mm in diameter or smaller. Our study also indicated that the en bloc + R0 resection rate was significantly higher for the ESD group than for the EMRC group with respect to lesions 11 mm in diameter or larger (p < 0.01).
Local recurrence is an important issue with curative treatment. Local recurrence occurs after piecemeal resection because tumor cells are left in the spaces of the resected mucosa. The en bloc + R0 resection rate for the EMRC group was only 4.5% (1/22) for lesions 21 mm in diameter or larger, in contrast to the complete resection rate achieved by ESD (i.e., 96.7%, 29/30) for these lesions. This fact explains why the EMRC group had a significantly higher local recurrence rate than the ESD group for lesions 21 mm in diameter or larger (p < 0.05).
An accurate histopathologic evaluation also is important for determining whether the patient needs additional treatments (e.g., esophagectomy and radiation therapy with or without chemotherapy). However, the evaluation is difficult to perform due to the intense thermal denaturation of the lesion caused by EMRC. In fact, ESD had a significantly longer mean procedure time than EMRC regardless of lesion size (p < 0.01). But the mean procedure time for ESD is not a severely negative variable considering its advantages, namely, low local recurrence rate, accurate histopathologic diagnosis, and precise pathologic staging. We believe that ESD is the best endoscopic procedure for resection of lesions 11 mm in diameter or larger.
The most serious complication during an endoscopic procedure is esophageal perforation that is potentially life threatening and may provoke severe mediastinitis. In this study, no significant difference in the esophageal perforation rate was found between the EMRC and ESD groups regardless of lesion size. Considering the difficulty of mastering ESD, we did not expect the ESD group to present favorable safety as represented by a perforation rate as low as 1.4% (1/71). We assessed neither the efficacy nor the safety of ESD performed by less experienced physicians.
The most serious complication after surgery is severe esophageal stricture that could provoke severe dysphagia and considerably decrease the patient’s quality of life. Katada et al. [22] demonstrated that a mucosal defect involving more than three-fourths of the esophageal circumference was significantly associated with the development of severe esophageal stricture after EMR.
In the current study, we found no severe esophageal stricture after procedure when the defect involved less than three-fourths of the esophageal circumference. Additionally, our results indicate that severe esophageal stricture developed statistically more frequently after EMRC than after ESD for patients with mucosal defects involving more than three-fourths of the esophageal circumference. To prevent severe esophageal stricture after procedure, therefore, maximum caution should be exercised against the excessive removal of the mucosa during procedure. Nevertheless, the mucosal defect caused by EMRC often is greater than expected because EMRC uses a snare, and the shape of the resected lesion cannot be controlled. Our study indicates that ESD is much more advantageous than EMRC in the aspect of reducing the risk for the stricture.
The current study involved limitations inherent to a retrospective study (e.g., selection bias, omission of required data, and confounding factors) but concurrently presented a great advantage of minimizing skill bias among operating endoscopists—the most important confounding factor for a clinical study assessing therapeutic outcomes of different endoscopic procedures. Consequently, our study provided favorable clinical outcomes in terms of efficacy, as represented by the 97.2% (69/71) en bloc complete resection rate, and in terms of safety, as represented by the 1.4% (1/71) peroration rate. These outcomes probably are attributable to the fact that operating endoscopists to perform ESD of the esophagus were restricted to two endoscopists proficient at ESD of the stomach (T.Y. and A.Z.).
Esophageal perforation provokes mediastinitis and may lead to a life-threatening situation. Therefore, the endoscopist who intends to perform ESD of the esophagus is strongly advised to accumulate plenary experience in ESD of the stomach. The local recurrence rate of lesions 11 to 20 mm in diameter was as low as 4.5% (1/22) for patients who underwent EMRC. Therefore, EMRC of these lesions may be a good optional endoscopic procedure for endoscopists who are short on experience in ESD.
To the best of our knowledge, our study is the first investigation to compare EMRC with ESD concerning the incidence of severe esophageal stricture after procedure during a follow-up period longer than 10 years.
In conclusion, our study demonstrates that ESD is superior to EMRC for the resection of SEC lesions 11 mm in diameter or larger because ESD has better efficacy, as assessed by the en bloc + R0 resection rate compared with EMRC, and because ESD is advantageous in preventing the risk of severe esophageal stricture after procedure. On the other hand, EMRC is appropriate only for SEC lesions 10 mm in diameter or smaller because it has en bloc + R0 resection rates comparable with those for ESD and is much faster than ESD. Therefore, the operating endoscopist should carefully select EMRC or ESD according to lesion size.
References
Watanabe A, Tsujie H, Taniguchi M, Hosokawa M, Fujita M, Sasaki S (2006) Laryngoscopic detection of pharyngeal carcinoma in situ with narrow-band imaging. Laryngoscope 116:650–654
Nonaka S, Saito Y (2008) Endoscopic diagnosis of pharyngeal carcinoma by NBI. Endoscopy 40:347–351
Makuuchi H, Yoshida T, Ell C (2004) Four-step endoscopic esophageal mucosal resection (EEMR) tube method of resection for early esophageal cancer. Endoscopy 36:1013–1018
Kato H, Tachimori Y, Mizobuchi S, Igari H, Ochiai A (1993) Cervical, mediastinal, and abdominal lymph node dissection (three-field dissection) for superficial carcinoma of the thoracic esophagus. Cancer 72:2879–2882
Roth JA, Putnam JB Jr (1994) Surgery for cancer of the esophagus. Semin Oncol 21:453–461
Kato H, Tachimori Y, Watanabe H, Yamaguchi H, Ishikawa T, Itabashi M (1990) Superficial esophageal carcinoma: surgical treatment and the results. Cancer 66:2319–2323
Shimizu Y, Tsukagoshi H, Fujita M, Hosokawa M, Kato M, Asaka M (2002) Long-term outcome after endoscopic mucosal resection in patients with esophageal squamous cell carcinoma invading the muscularis mucosae or deeper. Gastrointest Endosc 56:387–390
Inoue H, Takeshita K, Hori H, Muraoka Y, Yoneshima H, Endo M (1993) Endoscopic mucosal resection with a cap-fitted panendoscope for esophagus, stomach, and colon mucosal lesions. Gastrointest Endosc 39:58–62
Ishihara R, Ishii H, Uedo N, Takeuchi Y, Yamamoto S, Yamada T, Masuda E, Higashino K, Kato M, Narahara H, Tatsuta M (2008) Comparison of EMR and endoscopic submucosal dissection for en bloc resection of early esophageal cancers in Japan. Gastrointest Endosc 68:1066–1072
Ishihara R, Ishii H, Takeuchi Y, Kato M, Yamamoto S, Yamamoto S, Masuda E, Tatsumi K, Higashino K, Uedo N, Tatsuta M (2008) Local recurrence of large squamous cell carcinoma of the esophagus after endoscopic resection. Gastrointest Endosc 67:799–804
Oyama T, Tomori A, Hotta K, Morita S, Kominato K, Tanaka M, Miyata Y (2005) Endoscopic submucosal dissection of early esophageal cancer. Clin Gastroenterol Hepatol 3:67–70
Fujishiro M, Yahagi N, Kakushima N, Kodashima S, Muraki Y, Ono S, Yamamichi N, Tateishi A, Shimizu Y, Oka M, Ogura K, Kawabe T, Ichinose M, Omata M (2006) Endoscopic submucosal dissection of esophageal squamous cell neoplasms. Clin Gastroenterol Hepatol 4:688–694
Fujishiro M, Yahagi N, Kakushima N, Kodashima S, Ichinose M, Omata M (2006) En bloc resection of a large semicircular esophageal cancer by endoscopic submucosal dissection. Surg Laparosc Endosc Percutan Tech 16:237–241
Ishii N, Horiki N, Itoh T, Uemura M, Maruyama M, Suzuki S, Uchida S, Izuka Y, Fukuda K, Fujita Y (2010) Endoscopic submucosal dissection with a combination of small-caliber-tip transparent hood and flex knife is a safe and effective treatment for superficial esophageal neoplasias. Surg Endosc 24:335–342
Inoue H, Endo M, Takeshita K, Yoshino K, Muraoka Y, Yoneshima H (1992) A new simplified technique of endoscopic esophageal mucosal resection using a cap-fitted panendoscope (EMRC). Surg Endosc 6:264–265
Inoue H, Kawano T, Tani M, Takeshita K, Iwai T (1999) Endoscopic mucosal resection using a cap: techniques for use and preventing perforation. Can J Gastroenterol 13:477–480
Japanese Society for Esophageal Diseases (2002) Guidelines for clinical and pathologic studies on carcinoma of the esophagus. Kanehara, Tokyo, Japan
Choi IJ, Kim CG, Chang HJ, Kim SG, Kook MC, Bae JM (2005) The learning curve for EMR with circumferential mucosal incision in treating intramucosal gastric neoplasm. Gastrointest Endosc 62:860–865
Watanabe K, Ogata S, Kawazoe S, Watanabe K, Koyama T, Kajiwara T, Shimoda Y, Takase Y, Irie K, Mizuguchi M, Tsunada S, Iwakiri R, Fujimoto K (2006) Clinical outcomes of EMR for gastric tumors: historical pilot evaluation between endoscopic submucosal dissection and conventional mucosal resection. Gastrointest Endosc 63:776–782
Kakushima N, Fujishiro M, Kodashima S, Muraki Y, Tateishi A, Omata M (2006) A learning curve for endoscopic submucosal dissection of gastric epithelial neoplasms. Endoscopy 38:991–995
Yamashita T, Zeniya A, Otani S (2010) Endoscopic submucosal dissection (ESD) using the needleknife: its superiority to ESD using the insulation-tipped diathermic knife in physicians intending to master ESD. Surg Laparosc Endosc Percutan Tech 20:180–185
Katada C, Muto M, Manabe T, Boku N, Ohtsu A, Yoshida S (2003) Esophageal stenosis after endoscopic mucosal resection of superficial esophageal lesions. Gastrointest Endosc 57:165–169
Acknowledgment
The authors are grateful to Dr. Satoshi Sakima for his critical review of the manuscript.
Disclosures
Tatsuya Yamashita, Akira Zeniya, Hajime Ishii, Tsuyotoshi Tsuji, Satoko Tsuda, Kunio Nakane, and Masafumi Komatsu have no conflicts of interest or financial ties to disclose.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Yamashita, T., Zeniya, A., Ishii, H. et al. Endoscopic mucosal resection using a cap-fitted panendoscope and endoscopic submucosal dissection as optimal endoscopic procedures for superficial esophageal carcinoma. Surg Endosc 25, 2541–2546 (2011). https://doi.org/10.1007/s00464-011-1584-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00464-011-1584-6