Abstract
Background
The value of robotic assistance for intracorporeal suturing is not well defined. We compared robotic suturing with laparoscopic suturing on the FLS model with a large cohort of surgeons.
Methods
Attendees (n = 117) at the SAGES 2006 Learning Center robotic station placed intracorporeal sutures on the FLS box-trainer model using conventional laparoscopic instruments and the da Vinci® robot. Participant performance was recorded using a validated objective scoring system, and a questionnaire regarding demographics, task workload, and suturing modality preference was completed. Construct validity for both tasks was assessed by comparing the performance scores of subjects with various levels of experience. A validated questionnaire was used for workload measurement.
Results
Of the participants, 84% had prior laparoscopic and 10% prior robotic suturing experience. Within the allotted time, 83% of participants completed the suturing task laparoscopically and 72% with the robot. Construct validity was demonstrated for both simulated tasks according to the participants’ advanced laparoscopic experience, laparoscopic suturing experience, and self-reported laparoscopic suturing ability (p < 0.001 for all) and according to prior robotic experience, robotic suturing experience, and self-reported robotic suturing ability (p < 0.001 for all), respectively. While participants achieved higher suturing scores with standard laparoscopy compared with the robot (84 ± 75 vs. 56 ± 63, respectively; p < 0.001), they found the laparoscopic task more physically demanding (NASA score 13 ± 5 vs. 10 ± 5, respectively; p < 0.001) and favored the robot as their method of choice for intracorporeal suturing (62 vs. 38%, respectively; p < 0.01).
Conclusions
Construct validity was demonstrated for robotic suturing on the FLS model. Suturing scores were higher using standard laparoscopy likely as a result of the participants’ greater experience with laparoscopic suturing versus robotic suturing. Robotic assistance decreases the physical demand of intracorporeal suturing compared with conventional laparoscopy and, in this study, was the preferred suturing method by most surgeons. Curricula for robotic suturing training need to be developed.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Intracorporeal suturing is one of the most difficult advanced laparoscopic skills to accomplish. Mastery of this skill may enable surgeons to expand the spectrum of advanced laparoscopic procedures they can offer to their patients [1].
Robotic surgery is a promising new technology with a number of advantages over standard laparoscopy; in addition to making operations from a distance feasible, it offers improved visualization through a three-dimensional imaging system and surgeon-controlled camera manipulation, improved instrumentation with increased range of motion, and downscaling of surgeon’s movements that increase precision and improved ergonomics [2, 3]. The advantages of robotic assistance over standard laparoscopy have been demonstrated by several studies for novice learners [4–7], but they are less clear for experienced surgeons. In addition, currently, no significant clinical advantages have been realized in general surgery by the introduction of robotics [2].
The purpose of this study was to assess the effect of robotic assistance on experienced surgeons’ performance and preference on a well-defined task (intracorporeal suturing and knot tying) compared with standard laparoscopy.
Methods
Attendees at the robotic station at the SAGES 2006 Learning Center participated voluntarily in a simulator-based study protocol comparing laparoscopic with robotic suturing. Study details were fully disclosed to station participants, and they were informed that the collected data might be published. To maintain confidentiality, data collection was anonymous, and data were recorded on coded sheets without identifiers linking participants’ names to the data. The only exclusion criterion for the study (but not for participation in the station) was unwillingness to give verbal consent.
After verbal consent was obtained, participants were randomly assigned a number and completed the demographic data portion of the questionnaire (see “Appendix”). To minimize bias, all instructors were blinded to the participants’ demographics.
Participants watched a video tutorial of suturing and knot tying and were asked to perform at least one repetition with conventional laparoscopic instruments and one with the da Vinci® robotic system (Intuitive Surgical Inc., Sunnyvale, CA) on a Karl Storz videotrainer box using the FLS suturing model (Fig. 1). The da Vinci surgical system is a telemanipulator using robotic technology with an important distinction from other robotic systems in that it does not take action by itself. It consists of a console, a patient-side cart with three or four robotic arms, and a video tower, and it uses tremor filtration, motion scaling, three-dimensional view, and longer instruments that provide a full seven degrees of freedom due to an extension/flexion and a tilt function of the tip [8, 9] (Fig. 2).
Half of the participants were randomly assigned to start on the robotic and half on the laparoscopic simulator. Task duration, errors, and knot security were recorded, and a score was calculated based on the following formula: 300 − (time + accuracy error × 10 + approximation error × 10 + security error × 100). The time limit was 5 min (300 s) per task. Details about the calculation of this objective score have been published previously [10]. After completion of both laparoscopic and robotic suturing tasks, subjects completed the second part of the questionnaire pertaining to task workload and suture modality preference. The validated NASA-TLX questionnaire [11], which rates the mental, physical, and temporal demand of a task as well as the performance, effort, and frustration of the subject, was used for workload measurement. Construct validity for both tasks was assessed by comparing the performance scores of subjects with various levels of experience. To further assess the effect of experience on performance, workload, and suturing preference, we also analyzed separately and compared the results of two groups: laparoscopic suturing experts defined as participants who indicated that they had used laparoscopic suturing in more than 50 cases and novices who had not performed laparoscopic or robotic suturing before.
Data were analyzed using the SigmaStat® software (SPSS Inc., Chicago, IL). ANOVA on ranks, the Mann–Whitney rank sum test, and the χ2 test were used for statistical comparisons. A p < 0.05 was considered significant.
Results
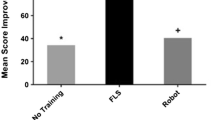
One hundred seventeen Learning Center attendees participated in the study. Eighty-four percent had prior laparoscopic suturing experience, but only 10% had prior robotic suturing experience. Participant characteristics are given in Table 1. Within the allotted time of 5 min, 83% of participants completed the suturing task laparoscopically and 72% with the robot. Construct validity was demonstrated for both simulated tasks according to the participants’ advanced laparoscopic experience, laparoscopic suturing experience, and self-reported laparoscopic suturing ability and according to prior robotic experience, robotic suturing experience, and self-reported robotic suturing ability (p < 0.001 for all comparisons, see Table 2). While participants achieved higher suturing scores with standard laparoscopy compared with the robot (84 ± 75 vs. 56 ± 63, respectively; p < 0.001), they found the laparoscopic task to be more physically demanding (NASA physical demand subscale score 13 ± 5 vs. 10 ± 5, respectively; p < 0.001, Fig. 3) and favored the robot as their method of choice for intracorporeal suturing (62 vs. 38%, respectively; p < 0.01). Differences between the expert and novice groups with regard to performance, workload scores, and suturing modality values are shown on Table 3.
Discussion
Advancements in technology have allowed many surgical procedures to be performed using minimally invasive techniques. With the use of novel energy source and stapling devices, many complex procedures can now be performed laparoscopically. Intracorporeal suturing is an important and necessary skill that all surgeons performing advanced laparoscopy should master [1]. Laparoscopic suturing is a difficult task to learn, as it is subject to the known limitations of laparoscopic surgery, including the loss of haptic feedback, limited degrees of freedom, the fulcrum and pivoting effect, and a two-dimensional view [2, 3].
Robotic systems have been developed to address the aforementioned constraints associated with laparoscopy and to improve precision. Such systems allow three-dimensional vision, motion scaling, camera control, automatic instrument change out, and tissue collision detection and thus may make difficult laparoscopic tasks such as suturing and knot tying easier, thus decreasing operator workload [2]. Indeed, in a recent study from our group that examined the benefits of robotic assistance during suturing by novice learners, we demonstrated that robotic assistance led to improved suturing performance, limited the number of inadvertent injuries to structures outside the operating field, shortened the learning curve of the task, and decreased operator workload in a live animal Nissen fundoplication model [12]. In another study, Moorthy et al. [13] demonstrated that the presence of a “wristed” instrument, tremor ablation, and motion scaling enhanced dexterity by nearly 50% compared with laparoscopic suturing and that three-dimensional vision enhanced dexterity by an additional 10–15%. Marecik et al. [14] evaluated robotic, laparoscopic, and hand-sewn suturing on porcine small intestine by residents. They reported that the robotic suture line created by midlevel residents was superior to laparoscopy although the times were equivalent. They also reported that the suturing was considered difficult by 92% in the laparoscopic group versus 17% in the robotic group [14]. In another experimental study on robotic suturing, Ruurda et al. [15] compared robotic and laparoscopic suturing on an end-to-end small intestine anastomosis model. They reported no difference in anastomosis time, number of stitches, and number of knots between the robotic and laparoscopic groups. They did, however, report shorter times per stitch and more suture ruptures in the robotic group and more stitch errors in the laparoscopic group [15]. A recent review by Kenngott [2] on robotic suturing reported that robotic systems in experimental studies had superior suturing capabilities compared with laparoscopic suturing and attributed the benefits to the three-dimensional visualization and the full seven degrees of freedom afforded by the robot.
While these benefits of robotic assistance to the inexperienced laparoscopist have been well documented in the literature [4–7], their importance for more experienced laparoscopists is a lot less clear. We therefore undertook the current study and chose to conduct it at the SAGES Learning Center to assess the impact of robotic assistance on a larger group of surgeons with more and variable laparoscopic experience. We found that robotic suturing was less demanding physically and the preferred method of suturing by the majority of our participants. We also demonstrated, however, that suturing scores were higher with standard laparoscopic instruments compared with robotic assistance. This finding is not unexpected, as most of our participants had significant prior advanced laparoscopic and laparoscopic suturing experience but minimal prior robotic experience. Furthermore, our subanalysis of experts in laparoscopic suturing and novices (Table 3) revealed that experts performed significantly better with standard laparoscopy and experienced higher workload when working with the robot, while novices had similar performance but less workload with the robot. Interestingly, while novices clearly indicated higher value to the robotic suturing system, experts assigned a similar value to both suturing modalities. In our opinion, these findings are indicative of a new learning curve for robotic suturing for expert laparoscopists, which is likely related to the different instruments and control of the instruments and the complete loss of haptic feedback, which is unique to the robotic task, rather than differences in the suturing task itself. Thus, experienced laparoscopists report a higher workload when they are trying to learn the new technique but still perform better than novices with robotic assistance, indicating a partial skill transfer. Despite this difficulty with the newer technique, the value ratings of experts were essentially identical for the two modalities, indicating that they realized some benefit with the robot. On the other hand, novice ratings were clearly in favor of the robot likely due to the easier accomplishment of the task. Prior studies corroborate our findings. In a group of eight physicians with variable laparoscopic experience, Yohannes et al. [4] demonstrated faster learning during the performance of laparoscopic dexterity tasks using robotic assistance compared with standard laparoscopy. The differences encountered were less pronounced for more experienced laparoscopists. In addition, Chang et al. [16] demonstrated that experienced laparoscopists registered initially inferior performance with the robot compared with conventional laparoscopy when performing intracorporeal suturing and knot tying. However, their robotic performance improved and surpassed that of laparoscopy after dedicated training. Thus, it is probable that expert laparoscopists have learned to overcome the constraints of laparoscopy, have little room for improvement, and experience a new learning curve when trying to adopt a new technique. This may be one of the reasons, in addition to increased cost, that surgeons hesitate to adapt the robotic technology.
It is also important to note that this is one of the first studies to demonstrate construct validity of the laparoscopic and robotic suturing tasks on the FLS model, as more experienced surgeons clearly outperformed the less experienced. This indicates that the SAGES/ACS-endorsed FLS suturing model is an excellent educational tool to teach both robotic and laparoscopic suturing.
A limitation of this study is that our participants had limited prior robotic experience compared with their laparoscopic experience. Thus, it was not possible to assess the value of the robot in a group of surgeons who were experts in both laparoscopic and robotic surgery. Furthermore, our pool of novices was small, not giving us the power needed to detect statistical differences for some parameters. In addition, the demographic data collected are subject to reporting and possibly recollection bias, but we do not believe that our results were affected significantly by these parameters. Finally, we did not assess the benefits of other suturing assisting devices that are available at a significantly lower cost than the robot.
In conclusion, construct validity was demonstrated for robotic suturing on the FLS model. Robotic assistance decreases the physical demand of intracorporeal suturing compared with conventional laparoscopy and, in this study, was the preferred suturing method by most surgeons. Curricula for robotic suturing training need to be developed.
References
Allen JW, Rivas H, Cocchione RN, Ferzli GS (2003) Intracorporeal suturing and knot tying broadens the clinical applicability of laparoscopy. JSLS 7:137–140
Kenngott HG, Muller-Stich BP, Reiter MA, Rassweiler J, Gutt CN (2008) Robotic suturing: technique and benefit in advanced laparoscopic surgery. Minim Invasive Ther Allied Technol 17:160–167
Stefanidis D, Korndorffer JR, Scott DJ (2005) Robotic laparoscopic fundoplication. Curr Treat Options Gastroenterol 8:71–83
Yohannes P, Rotariu P, Pinto P, Smith AD, Lee BR (2002) Comparison of robotic versus laparoscopic skills: is there a difference in the learning curve? Urology 60:39–45 (discussion 45)
Mohr CJ, Nadzam GS, Alami RS, Sanchez BR, Curet MJ (2006) Totally robotic laparoscopic Roux-en-Y gastric bypass: results from 75 patients. Obes Surg 16:690–696
Sanchez BR, Mohr CJ, Morton JM, Safadi BY, Alami RS, Curet MJ (2005) Comparison of totally robotic laparoscopic Roux-en-Y gastric bypass and traditional laparoscopic Roux-en-Y gastric bypass. Surg Obes Relat Dis 1:549–554
Mohr CJ, Nadzam GS, Curet MJ (2005) Totally robotic Roux-en-Y gastric bypass. Arch Surg 140:779–786
Gutt CN, Oniu T, Mehrabi A, Kashfi A, Schemmer P, Buchler MW (2004) Robot-assisted abdominal surgery. Br J Surg 91:1390–1397
Rassweiler J, Safi KC, Subotic S, Teber D, Frede T (2005) Robotics and telesurgery—an update on their position in laparoscopic radical prostatectomy. Minim Invasive Ther Allied Technol 14:109–122
Korndorffer JR Jr, Dunne JB, Sierra R, Stefanidis D, Touchard CL, Scott DJ (2005) Simulator training for laparoscopic suturing using performance goals translates to the operating room. J Am Coll Surg 201:23–29
Hart SG, Staveland LE (1988) Development of NASA-TLX (task load index): results of empirical and theoretical research. In: Hancock PA, Meshkati N (eds) Human mental workload. Elsevier, Amsterdam, pp 139–183
Stefanidis D, Wang F, Korndorffer JR Jr, Dunne JB, Scott DJ (2010) Robotic assistance improves intracorporeal suturing performance and safety in the operating room while decreasing operator workload. Surg Endosc 24(2):377–382
Moorthy K, Munz Y, Dosis A, Hernandez J, Martin S, Bello F, Rockall T, Darzi A (2004) Dexterity enhancement with robotic surgery. Surg Endosc 18:790–795
Marecik SJ, Prasad LM, Park JJ, Jan A, Chaudhry V (2008) Evaluation of midlevel and upper-level residents performing their first robotic-sutured intestinal anastomosis. Am J Surg 195:333–337 (discussion 337–338)
Ruurda JP, Broeders IA, Pulles B, Kappelhof FM, van der Werken C (2004) Manual robot assisted endoscopic suturing: time-action analysis in an experimental model. Surg Endosc 18:1249–1252
Chang L, Satava RM, Pellegrini CA, Sinanan MN (2003) Robotic surgery: identifying the learning curve through objective measurement of skill. Surg Endosc 17:1744–1748
Acknowledgments
The authors thank Chris Bell, MD, Lee Ann Lau, MD, Marc Zerey, MD, Makram Gedeon, MD, Andrew Harrell, MD, and George Walker, RN, for their help with the conduct of this study and data acquisition. We also thank Anahita Mostafavi and Amanda Walters, BS, for their help with data entry and analysis.
Disclosures
Dimitrios Stefanidis, William W. Hope, and Daniel J. Scott have no conflicts of interest or financial ties to disclose.
Author information
Authors and Affiliations
Corresponding author
Appendix: Robotic suturing questionnaire
Appendix: Robotic suturing questionnaire


Rights and permissions
About this article
Cite this article
Stefanidis, D., Hope, W.W. & Scott, D.J. Robotic suturing on the FLS model possesses construct validity, is less physically demanding, and is favored by more surgeons compared with laparoscopy. Surg Endosc 25, 2141–2146 (2011). https://doi.org/10.1007/s00464-010-1512-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00464-010-1512-1