Abstract
Background
Conversion from laparoscopic to open cholecystectomy may not be desirable due to the increased complication rate and prolonged convalescence. In Denmark, nationwide data show that 7.7% of the laparoscopic cholecystectomies are converted to open surgery. This article aims to document the relationship of gender to conversion rate and length of hospital stay after laparoscopic cholecystectomy in a national cohort of patients.
Methods
The gender of 5,951 patients from the 2007 National Danish Cholecystectomy Database was compared with conversion rate, length of hospital stay, and various risk factors using multivariate analyses.
Results
The findings showed that 14.3% of the patients had acute cholecystitis and that men had the highest risk (odds ratio [OR], 1.94; 95% confidence interval [CI], 1.66–2.27). The operative findings for the men included sequelae from previous acute cholecystitis more frequently than the findings for the women (OR, 1.89; 95% CI, 1.67–2.15). The rate for conversion from laparoscopic to open surgery was 7.7%, and male sex was highly associated with conversion (OR, 2.48; 95% CI, 2.04–3.01). Thus, 259 (5.8%) of the 4,451 operations for women were converted to laparotomy compared with 199 (13.3%) of the 1,500 operations for men. No significant sex differences were found in the proportion of bile duct lesions (those requiring reconstructive surgery as well as those that could be handled by endoscopy or T-tube drainage, suturing, or both) or in the 30-day mortality rate. The multivariate analyses showed that male sex was a significant factor for conversion but not for length of postoperative stay or readmission.
Conclusion
Men showed a significantly higher risk of the operation being converted from laparoscopic to open cholecystectomy than women (OR, 2.48; 95% CI, 2.04–3.01). The main reason for this may be that men more frequently had acute cholecystitis or sequelae from previous acute cholecystitis. These results can be used to give patients a better basis for their informed consent and better resource management in connection with the operation.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
The laparoscopic technique is by far the treatment of choice for the performance of cholecystectomy, and with growing experience, more patients have been treated by laparoscopy [1]. These authors concluded that this has resulted in lower morbidity rates, shorter hospital stays, and quicker returns to work [2]. The cosmetic result also is important for most patients. However, conversion to open surgery is sometimes necessary. This was the case for 7.7% of Danish patients in 2007 [3]. The conversion rate corresponds well with results from Switzerland in a study of 22,953 patients (conversion, rate 8.5%) [4]. Mortality rates seem to be higher when primary laparoscopic operations are converted to open surgery [5]. Identification of risk factors for conversion to open surgery will make the surgeon more capable to inform and prepare patients for the operation and the expected outcome.
This article aims to document the relationship of gender to conversion rate and length of postoperative hospital stay after laparoscopic cholecystectomy in the Danish population.
Methods
Patient data from the year 2007 was pulled from the national Danish Cholecystectomy Database [6], which comprises two sets of data, as described earlier [7]: (1) clinical data registered immediately after the operation by the surgeon through a secure Web site to the database and (2) administrative data from the National Patient Registry (Box 1). Several indicators can be derived from these data and used to monitor the quality of surgery [7, 8].
Length of postoperative hospital stay (LOS) was defined with operation day as day 0 [8]. The American Society of Anesthesiology (ASA) score was determined according to the standard of that organization. The diagnosis of “previous acute cholecystitis” required finding of a thick-walled fibrotic gallbladder with or without adhesions. “Previous pancreatitis” required that the patient had been hospitalized due to acute pancreatitis within the 3 months before the cholecystectomy.
The Danish Cholecystectomy Database was created in 2004 and made mandatory nationwide in 2006. A report is made each year, and statistics are sent to the respective departments to provide the most complete data set possible. The database has been validated with data from 2004 to 2005, and these data were found to be a valid tool for monitoring the quality of the database (97.1–100% agreement between journals and administrative data; kappa, 0.73–1.00) [7].
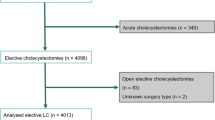
In 2007, 7,011 cholecystectomies were performed (Table 1). Of the patients involved, 828 were excluded due to data-recording errors, and 232 patients were excluded because they had primary open operations. A total of 5,951 patients with intended laparoscopic operations were analyzed. Of these patients, 1,500 (25.2%) were men.
Statistical analyses were conducted using SAS 9.1 (SAS Institute Inc., Cary, NC, USA). The normality of the scale variables was tested with the Kolmogorov–Smirnov test. Variables without normal distribution are given as median and range. Categorical variables are given as numbers and percentages. The Student t-test and chi-square test were used to analyse for potential associations with the patient’s sex, whereas the Mann–Whitney test (rank-sum) was used to rank scale variables. The results are considered to be statistically significant at a p value of 0.05 or less. Multiple logistic regression analyses were performed in several models.
Results
The men were significantly older than the women (p = 0.0002). The mean age was 47 years (range, 11–101 years) for the women and 53 years (range, 15–93 years) for the men. There was a minor but significant difference in body mass index (BMI) between the men (27.5 kg/cm2; 95% confidence interval [CI], 27.3–27.7) and the women (27.9 kg/cm2; 95% CI, 27.8–28.1). The average ASA score of 1.38 for the women was significantly lower than 1.43 for the men (p = 0.021), with a total of 5,727 patients (96.2%) scoring 1 or 2.
The distribution of the risk factors is shown in Table 2. There was a higher percentage of acute cholecystitis among the men than among the women. The men had sequelae more frequently after previous cholecystitis and previous pancreatitis, such as dense adhesions or a fibrous gallbladder wall found during the operation. The frequency of previous upper abdominal surgery was not significantly different between the sexes.
The primary outcomes are shown in Table 3. The findings show that significantly more of the operations were converted from laparoscopic to open surgery among the men than among the women (odds ratio [OR], 2.48; 95% CI, 2.04–3.01). Thus, 259 (5.8%) of 4,451 operations for the women were converted to laparotomy compared with 199 (13.3%) of 1,500 operations for the men. Altogether, 7.7% of the operations were converted to laparotomy.
The findings also showed a significant difference in the postoperative LOS, because men were more often admitted longer than 1 day (OR, 1.5; 95% CI, 1.33–1.70), and had a higher risk of an LOS longer than 3 days and of a readmittance (OR, 1.48; 95% CI, 1.28–1.71). The total number of hospitalization days at the primary hospitalization after surgery averaged 1.3 days for the women and 1.9 days for the men (p < 0.001), with a maximum of 73 days for the women and 78 days for the men. There were no differences in the proportion of biliary tract injuries or in mortality.
The overall 30-day mortality rate was 0.4%, with no specific relationship to gender (OR, 0.93; 95% CI, 0.34–2.53), and the proportion of biliary tract injuries was 0.5% (n = 27), again, with no relationship to sex (OR, 0.96; 95% CI, 0.39–2.70). Of these injuries, 12 (0.2%) were injuries with transection or ligation of the common bile duct that needed reconstruction, typically with a hepaticojejunostomy [9].
A multivariate model was tested with logistic regression analysis. As shown in Table 4, male gender was a significant factor for conversion (OR, 1.58; 95% CI, 1.27–1.96) as were age, BMI, acute cholecystitis, and sequelae after acute cholecystitis. Two models were set for LOS and readmission but did not show a significant correlation between sex and LOS. A fourth model tested with patients undergoing additional procedures also showed no significant association with sex (OR, 0.86; 95% CI, 0.73–1.01).
Discussion
The multivariate logistic regression analyses showed a significant sex-dependent difference in the risk for conversion to open surgery. Age, BMI, acute cholecystitis, and sequelae after prior acute cholecystitis also were significant predictors of conversion.
A recent study of 2,000 patients also found that men had a greater risk for conversion (OR, 2.0; 95% CI, 1.3–2.9), but when multivariate analysis was used to control for confounders, the significant difference disappeared [10]. A larger study including 22,953 patients from the years 1995 through 2003 found by multivariate analysis that the perioperative complication rate was higher for men (OR, 1.18; p < 0.02) [4]. Perioperative complications often are a good indication for conversion, and other studies [11–17] have shown an association of perioperative complications with a high risk for conversion, so this association is well in line with the results of the current study.
The differences in risk factors and conversion rates between men and women are hard to explain. Differences in anatomy or physiology such as volume of the abdomen, hormones, or fat distribution may play a role. Alternatively, behavioral differences may contribute (i.e., men may have a longer duration of symptoms before seeking a physician).
One article points to an association between men with great body weight and severity of gallbladder inflammation [4]. Greater body weight led to a greater risk of empyema formation and gallbladder perforation. Thus, 62% of perforations were found in men weighing more than 70 kg. A second study found a significant difference between men and women in the amount of inflammation found during surgery (OR, 1.9; p < 0.001) [10]. A third study reviewed 326 patients with acute cholecystitis and found that male sex was an independent risk factor for more complicated disease (OR, 1.76; p = 0.029) [18]. The findings also showed that the main reason for conversion was anatomic changes around the gallbladder [18].
Several other studies have suggested that anatomic changes due to inflammation and adherences were the main reasons for conversions [13–15, 17, 19–22]. An early study from 1992 to 1994 examined the relationship between the success rate for laparoscopic surgery and the time from onset of acute cholecystitis symptoms to surgery. The success rate dropped significantly after the first 4 days with pain [23]. These results have been confirmed in more recent studies [19, 24].
None of the aforementioned studies have addressed the reason for the apparent increased inflammation and adherence formation in men. One study of 80 patients with symptomatic gallbladder stones showed that men had a significantly higher amount of hydroxyproline (collagen component) in the connective tissues of the gallbladder wall and in the pericholecystic tissues than women [25]. Moreover, they found a significantly higher number of macrophages, mast cells, and eosinophilic granulocytes in tissue samples from the gallbladder wall and pericholecystic tissue of men. The authors point out the difference in hormone levels as an explanatory model, in which a higher testosterone level may lead to increased fibroblast activity and consequently collagen synthesis, fibrosis, and adherences. Further research into inflammatory processes and connective tissue formation in men and women is needed to explain the observed sex differences.
In contrast to the conversion rate, we found no significant association between male gender and LOS or readmissions. This confirms the results from a previous study [10]. Giger et al. [4] found that the risk of postoperative local complications was associated with male sex (OR, 1.26; p < 0.003). The risk of postoperative systemic complications was not associated with sex, whereas age, acute cholecystitis, conversion, ASA score, and duration of surgery were associated. Previous findings have shown LOS to be highly associated with complications, organizational quality, or both [7], meaning that it often is possible to achieve a fast-track optimized regimen in laparoscopic cholecystectomy by a simple reorganization of patient care in the department.
In conclusion, our nationwide data showed that men had a significantly higher risk for conversion of laparoscopic cholecystectomy to open surgery than women. The reason may be that men more frequently had acute cholecystitis or sequelae from previous acute cholecystitis. Whatever the reason for these differences, the increased risk for men should be included in the risk calculation before surgery. Our results can be used to improve preoperative information and give patients a better foundation for their informed consent. In resource management, it also is important to know the risks and be prepared for conversion.
References
Ainsworth A, Adamsen S, Rosenberg J (2005) Kolecystektomi i Danmark 1989–2003. Ugeskr Læger 167:2648–2650
Keus F, de Jong JAF, Gooszen HG, van Laarhoven CJHM (2006) Laparoscopic versus open cholecystectomy for patients with symptomatic cholecystolithiasis. Cochrane Database Syst Rev CD006231
Dansk Galde Database Årsrapport 2006 (2007). Retrieved November 2008 at http://kliniskedatabaser.dk/artikeldataVis.asp?id=27&m=2
Giger UF, Michel JM, Opitz I, Inderbitzin DT, Kocher T, Krähenbühl L (2006) Risk factors for perioperative complications in patients undergoing laparoscopic cholecystectomy. J Am Coll Surg 203:723–728
Wolf AS, Nijsse BA, Sokal SM (2009) Surgical outcomes of open cholecystectomy in the laparoscopic era. Am J Surg 197:781–784
Bardram L, Rosenberg J, Kristiansen V (2005) Dansk galde database–DGD. Ugeskr Læger 167:2618–2620
Harboe KM, Anthonsen K, Bardram L (2009) Validation of data and indicators in the Danish Cholecystectomy Database. Int J Qual Health Care 21:160–168
Galde Database Kliniske indikatorer. Retrieved November 2008 at http://kliniskedatabaser.dk/artikeldataVis.asp?id=27&m=2
Dansk Galde Database Årsrapport 2007 (2008). Retrieved July 2009 at http://kliniskedatabaser.dk/artikeldataVis.asp?id=27&m=2
Botaitis S, Polychronidis A, Pitiakoudis M, Perente S, Simopoulos C (2008) Does gender affect laparoscopic cholecystectomy? Surg Laparosc Endosc Percutan Tech 18:157–161
Russell JC, Walsh SJ, Reed-Fourquet L, Mattie A, Lynch J (1998) Symptomatic cholelithiasis: a different disease in men? Ann Surg 227:195–200
Livingston EH, Rege RV (2004) A nationwide study of conversion from laparoscopic to open cholecystectomy. Am J Surg 188:205–211
Kama NA, Kologlu M, Doganay M, Reis E, Atli M, Dolapci M (2001) A risk score for conversion from laparoscopic to open cholecystectomy. Am J Surg 181:520–525
Zisman A, Gold-Deutch R, Zisman E, Negri M, Halpern Z, Lin G, Halevy A (1996) Is male gender a risk factor for conversion of laparoscopic into open cholecystectomy? Surg Endosc 10:892–894
Lipman JM, Claridge JA, Haridas M, Martin MD, Yao DC, Grimes KL, Malangoni MA (2007) Preoperative findings predict conversion from laparoscopic to open cholecystectomy. Surgery 142:556–563
Ibrahim S, Hean TK, Ho LS, Ravintharan T, Chye TN, Chee CH (2006) Risk factors for conversion to open surgery in patients undergoing laparoscopic cholecystectomy. World J Surg 30:1698–1704
Tang B, Cuschieri A (2006) Conversions during laparoscopic cholecystectomy: risk factors and effects on patient outcome. J Gastrointest Surg 10:1081–1091
Lee HK, Han HS, Min SK, Lee JH (2005) Sex-based analysis of the outcome of laparoscopic cholecystectomy for acute cholecystitis. Br J Surg 92:463–466
Gharaibeh KIA, Qasaimeh GR, Al-Heiss H, Ammari F, Bani-Hani K, Al-Jaberi TM, Al-Natour S (2002) Effect of timing of surgery, tape of inflammation, and sex on outcome of laparoscopic cholecystectomy for acute cholecystitis. J Laparoendosc Adv Surg Tech A 12:193–198
Rosen M, Brody F, Ponsky J (2002) Predictive factors for conversion of laparoscopic cholecystectomy. Am J Surg 184:254–258
Bingener-Casey J, Richards ML, Strodel WE, Schwesinger WH, Sirinek KR (2002) Reasons for conversion from laparoscopic to open cholecystectomy: a 10-year review. J Gastrointest Surg 6:800–805
Simopoulos C, Botaitis S, Polychronidis A, Tripsianis G, Karayiannakis AJ (2005) Risk factors for conversion of laparoscopic cholecystectomy to open cholecystectomy. Surg Endosc 19:905–909
Bickel A, Rappaport A, Kanievski V, Vaksman I, Haj M, Geron N, Eitan A (1996) Laparoscopic management of acute cholecystitis: prognostic factors for success. Surg Endosc 10:1045–1049
Teixeira JPA, Saraiva AC, Cabral AC, Barros H, Reis JR, Teixeira A (2000) Conversion factors in laparoscopic cholecystectomy for acute cholecystitis. Hepatogastroenterology 47:626–630
Yol S, Kartal A, Vatansev C, Aksoy F, Toy H (2006) Sex as a factor in conversion from laparoscopic cholecystetomy to open surgery. JSLS 10:359–363
Disclosures
Simon E. Thesbjerg, Kirstine M. Harboe, Linda Bardram, and Jacob Rosenberg have no conflicts of interest or financial ties to disclose.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Thesbjerg, S.E., Harboe, K.M., Bardram, L. et al. Sex differences in laparoscopic cholecystectomy. Surg Endosc 24, 3068–3072 (2010). https://doi.org/10.1007/s00464-010-1091-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00464-010-1091-1